妊娠期糖尿病孕婦不同孕周陰道菌群變化及對妊娠結局的影響:前瞻性隊列研究
楊昕暉 彭笑笑 馬麗麗 趙國玉 馬秀華 郭晶


引用本文:楊昕暉,彭笑笑,馬麗麗,等. 妊娠期糖尿病孕婦不同孕周陰道菌群變化及對妊娠結局的影響:前瞻性隊列研究[J]. 中國全科醫學,2024,27(29):3587-3594. DOI:10.12114/j.issn.1007-9572.2024.0191. [www.chinagp.net]
YANG X H,PENG X X,MA L L,et al. Title vaginal microbiota changes of gestational diabetes mellitus pregnant women at different gestational weeks and the impact on pregnancy outcome:a prospective cohort study[J]. Chinese General Practice,2024,27(29):3587-3594.
? Editorial Office of Chinese General Practice. This is an open access article under the CC BY-NC-ND 4.0 license.
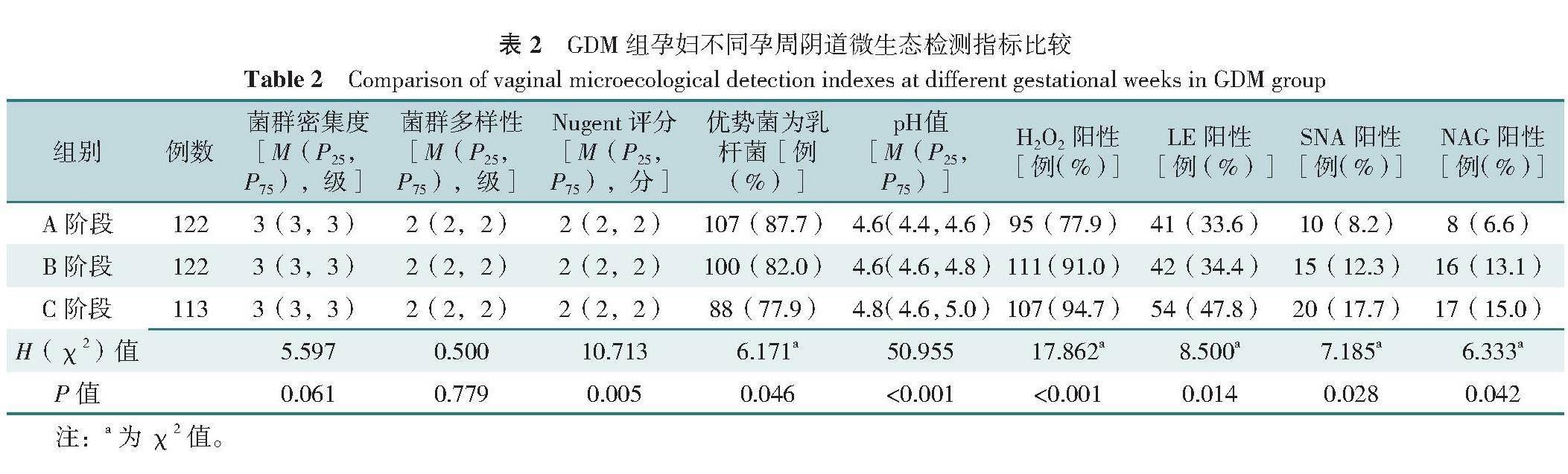
【摘要】 背景 妊娠期糖尿病(GDM)是妊娠期常見并發癥,既往研究表明,GDM孕婦生殖道感染性疾病的患病風險較高,但相關隊列研究少見。目的 了解GDM孕婦不同孕周陰道菌群變化特點,對比GDM孕婦與非GDM孕婦陰道菌群差異,觀察陰道菌群異常對妊娠結局的不良影響。方法 本研究采用連續抽樣法,選取2022年3月—2023年3月在首都醫科大學大興教學醫院建立檔案并規范保健的孕婦,在妊娠24~28周行75 g口服糖耐量試驗(OGTT)檢查,診斷是否為GDM。采用傾向得分匹配法(PSM)進行GDM組與非GDM組1∶1匹配,于妊娠24~28周(A階段)、妊娠32~35周(B階段)和妊娠37~40周(C階段)分別采集陰道分泌物,進行3次陰道微生態檢測,并進一步分為GDM陰道菌群正常組、GDM陰道菌群異常組、非GDM陰道菌群正常組及非GDM陰道菌群異常組,隨訪至分娩后7 d以評估妊娠結局。結果 本研究最初納入426名參與者,141例發生GDM。經過PSM匹配,GDM組和非GDM組成功匹配122對,作為研究隊列。本研究中有9例GDM孕婦和5例非GDM孕婦發生早產(妊娠<37周),故最終有113例GDM孕婦和117例非GDM孕婦進入C階段。A階段陰道菌群優勢菌為乳桿菌所占比例高于C階段,陰道pH值、陰道菌群異常發生率、細菌性陰道病(BV)及外陰陰道假絲酵母菌病(VVC)發生率均低于C階段(P<0.05)。A階段GDM組優勢菌為乳桿菌所占比例高于非GDM組,陰道菌群異常和VVC發生率均低于非GDM組(P<0.05)。C階段GDM組優勢菌乳桿菌比例低于非GDM組,陰道菌群異常發生率高于非GDM組(P<0.05)。GDM陰道菌群異常組(n=65)不良妊娠結局發生率高于GDM陰道菌群正常組(n=57)(P<0.05);GDM陰道菌群異常組不良妊娠結局的發生風險是GDM陰道菌群正常組的1.830倍(RR=1.830,95%CI=1.293~2.590,P<0.001)。結論 GDM孕婦在妊娠37~40周時,陰道菌群異常發生率高于妊娠24~28周。相比于非GDM孕婦,GDM孕婦在妊娠24~28周時陰道菌群異常發生率低,而在妊娠37周后,陰道菌群異常發生風險升高。妊娠期陰道菌群異常是發生不良妊娠結局的危險因素,建議加強妊娠期陰道微生態的檢測與管理。
【關鍵詞】 妊娠期糖尿病;妊娠中期;妊娠晚期;陰道菌群;妊娠結局;隊列研究
【中圖分類號】 R 714.256 【文獻標識碼】 A DOI:10.12114/j.issn.1007-9572.2024.0191
Title Vaginal Microbiota Changes of Gestational Diabetes Mellitus Pregnant Women at Different Gestational Weeks and the Impact on Pregnancy Outcome:a Prospective Cohort Study
YANG Xinhui1,PENG Xiaoxiao2,MA Lili3,ZHAO Guoyu3,MA Xiuhua3*,GUO Jing1
1.Department of General Medicine,Beijing Friendship Hospital,Capital Medical University,Beijing 100050,China
2.Department of General Medicine,Daxing Teaching Hospital of Capital Medical University,Beijing 102600,China
3.Department of Gynecology and Obstetrics,Daxing Teaching Hospital of Capital Medical University,Beijing 102600,China
*Corresponding author:MA Xiuhua,Chief physician/Professor/Doctoral supervisor;E-mail:mxhdxqyy@126.com
【Abstract】 Background Gestational diabetes mellitus(GDM) is a common complication of pregnancy,and previous studies have shown that pregnant women with GDM have a higher risk of developing infectious diseases of the reproductive tract than healthy pregnant women,but relevant cohort studies are rare. Objective To investigate the variation characteristics of vaginal microbiota in pregnant women with GDM at different gestational weeks,to compare the differences of vaginal microbiota between GDM and non-GDM women,and to observe the effects of vaginal microbiota changes on pregnancy outcomes. Methods In this study,we used a consecutive sampling method to recruit pregnant women who established their records and regulated health care at Daxing Teaching Hospital of Capital Medical University from March 2022 to March 2023. They underwent 75 g oral glucose tolerance test(OGTT) at 24-28 weeks of gestation to diagnose GDM. The GDM group was matched 1∶1 with the non-GDM group using propensity score matching method(PSM). Sample of vaginal secretions were collected at 24-28 weeks(stage A),32-35 weeks(stage B) and 37-40 weeks(stage C) for three vaginal microecological examination,respectively. Based on the results,participants were further divided into the GDM normal vaginal flora subgroup,GDM abnormal vaginal flora subgroup,non-GDM normal vaginal flora subgroup and non-GDM abnormal vaginal flora subgroup,and were followed up until 7 d after delivery to assess pregnancy outcome. Results A total of 426 participants were initially enrolled in this study,and GDM occurred in 141 cases. After PSM mathing,the GDM and non-GDM groups were successfully matched in 122 pairs. In this study,because 9 women with GDM and 5 women without GDM had preterm birth(<37 weeks of gestation),113 women with GDM and 117 women without GDM ended up in stage C. The proportion of the dominant vaginal flora of Lactobacillus was higher in stage A than in stage C. Moreover,the vaginal pH,the incidence of vaginal flora abnormalities,and the incidence of BV and VVC were lower than those in stage C(P<0.05). The proportion of dominant bacteria as Lactobacillus in the GDM group was higher than that in the non-GDM group,and the incidence of abnormal vaginal flora and VVC was lower than that in the non-GDM group in stage A(P<0.05). In contrast,the proportion of the dominant bacterium Lactobacillus was lower in the GDM group than in the non-GDM group,and the incidence of abnormal vaginal flora was higher than in the non-GDM in stage C(P<0.05). The incidence of adverse pregnancy outcomes was higher in the GDM abnormal vaginal flora subgroup(n=65)than in the GDM normal vaginal flora subgroup(n=57)(P<0.05). In more details,the risk of adverse pregnancy outcomes in the GDM abnormal vaginal flora group was 1.830 times higher than that in the GDM normal vaginal flora group(RR=1.830,95%CI=1.293-2.590,P<0.001). Conclusion Compared with non-GDM pregnant women,GDM pregnant women had a lower incidence of vaginal flora abnormalities at 24-28 weeks of gestation and an increased risk of vaginal flora abnormalities after 37 weeks of gestation. GDM pregnant women with abnormal flora have higher risk of adverse pregnancy outcomes,so we recommend enhanced testing and management of vaginal microecology during pregnancy.
【Key words】 Gestational diabetes mellitus;Pregnancy trimester,second;Pregnancy trimester,third;Vaginal microbiota;Pregnancy outcome;Cohort study
妊娠期糖尿病(gestational diabetes mellitus,GDM)是由于妊娠期糖代謝異常而首次發生或發現的一類糖尿病,與多種不良妊娠結局相關,全球患病率為14.0%[1],我國患病率為14.8%[2]。隨著生育政策調整,孕婦年齡及孕產次增加,GDM發病率呈逐年增長趨勢。……