Lesson Sixty-three The V2transition ratio
——a new electrocardiographic criterion for distinguishing left from right ventricular outflow tract tachycardia origin
●心電學英語
Lesson Sixty-three The V2transition ratio
——a new electrocardiographic criterion for distinguishing left from right ventricular outflow tract tachycardia origin
Outflow tract ventricular tachycardia(OTVT)represents the most common subgroup of idiopathic ventricular tachycardia(VT).The clinical presentation of OTVT is heterogeneous,ranging from isolated premature ventricular contractions(PVCs)to repetitive nonsustained VT to sustained VT.
Detailedintracardiac electrical mapping has demonstrated that the vast majority of OTVTs originate from the anterior and superior septal aspect of the right ventricular outflow tract(RVOT),just inferior to the pulmonic valve.Less commonly,the site of origin can be localized to the right ventricular(RV)infundibulum,RV free wall,and posterior aspect of the interventricular septum.In approximately 10%to 15%of cases,the arrhythmia originates from the left ventricular outflow tract (LVOT)and can be mapped to the region of the aortic cusps.Rarely,OTVTs can be ablated from within the anterior interventricular vein,aorto-mitral continuity,or the root of the pulmonary artery.
Because OTVT has a focal origin and occurs in patients with structurally normal hearts,it is an arrhythmia that is particularly conducive to localization with the 12-lead electrocardiography(ECG).Typically,OTVT originating in the RV manifests an inferior axis in the frontal plane and left bundle branch block(LBBB)configuration with precordial R/S transition at or after lead V3.By contrast,LVOT VT usually manifests either a right bundle branch block(RBBB)/inferior axis or a LBBB/inferior axis with a precordial R/S-wave transition at or before lead V3.
Criteria to distinguish RVOT from LVOT origin for patients with precordial transition occurring at lead V3have been lacking.The aim of this study was to develop an ECG algorithm for reliably predicting the site of origin of OTVTs with lead V3precordial R/S transition.We hypothesized that comparison of the PVC/VT with the sinus rhythm(SR)QRS morphology would be an effective means of distinguishing LVOT from RVOT VT.
Methods
This study was designed in 2 parts:1)a retrospective review of OTVT ablation cases in order to develop the ECG algorithm;and 2)a prospective assessment of the algorithm on a second group of patients.
Patients with PVCs/VT manifesting a LBBB/inferior axis and a precordial transition(from R/S<1 to R/S>1)at lead V3were included.The majority of patients had normal left ventricular function by echocardiography.Patients with ECG evidence of prior myocardial infarction,RBBB during SR,or whose clinical arrhythmia could not be abolished with catheter ablation were excluded.
Mapping and ablation protocol
A standard quadripolar catheter was positioned in the RV apical position,and a 4mm nonirrigated catheter was initially positioned in the RVOT for mapping.In patients with sufficient ectopy,activation mapping wasperformed,recording the earliest local bipolar activation time compared with surface QRS of the clinical PVC. Pace-mapping at a threshold just above local capture was performed in all cases with careful comparison of the paced surface QRS morphology with that of the clinical PVC.All idiopathic PVCs/VT in this series originated from the septal side of the RVOT just beneath the pulmonic valve.
The decision to extend mapping to a LVOT site was made if no adequate RVOT sites were identified or ablation in the RVOT was unsuccessful in abolishing the arrhythmia.The LVOT sites were mapped via a retrograde aortic approach.All mapping was performed after heparin bolus,maintaining an activated clotting time>250 s.In addition to standard fluoroscopy,a 3-dimensional electroanatomic mapping system and intracardiac echocardiography were used to localize the anatomic position of the ablation catheter within the outflow tract. ECG measurement protocol
Sinus rhythm and VT ECG morphology were measured on the same 12-lead ECG.During the clinical arrhythmia,the following measurements were obtained during both SR and the PVC/VT:1)R-and S-wave amplitudes in leadⅠ,Ⅱ,Ⅲ,aVF,and V1to V3;2) R-wave duration in leads V1to V3;3)QRS duration;and 4)QRS frontal axis(Figure 1).The T-P segment was considered the isoelectric baseline for measurement of R-and S-wave amplitudes.The QRS duration was measured from the site of earliest initial deflection from the isoelectric line in any lead to the time of latest activation in any lead.The R-wave duration was measured from the site of earliest initial deflection from the isoelectric line to the time at which the R-wave intersected the isoelectric line.For all cases,QRS measurements were performed on isolated PVCs representative of the clinical VT before the induction of sustained VT and compared with the SR QRS complex.As a means of accounting for1respiratory variation,we standardized our SR measurements by measuring the largest R-and S-wave over a 10s window at 25mm/s sweep speed.The transition ratio was calculated in leads V2and V3by computing the percentage R-wave during VT(R/R+S) VT divided by the percentage R-wave in SR(R/R+S) SR.
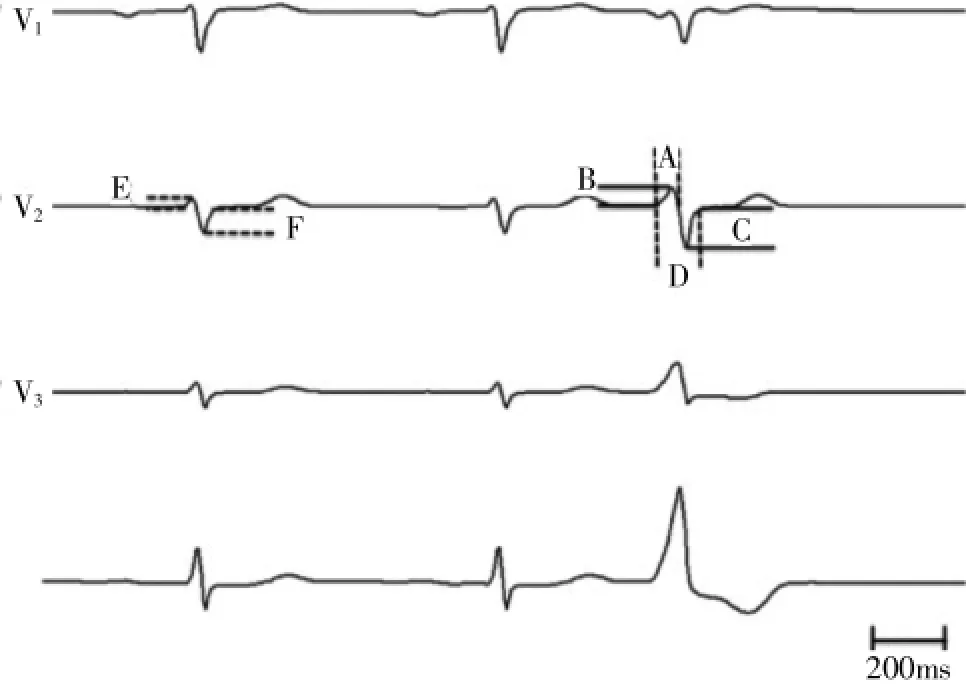
Figure 1Electrocardiographic Measurements.Leads V2and V3of normal sinus beat followed by a premature ventricular contraction (PVC)representative of the clinical outflow tract ventricular tachycardia.Measurements are as follows:A=PVC R-wave duration(ms);B=PVC R-wave amplitude(mV);C=PVC S-wave amplitude(mV);D=PVC QRS duration(ms);E= sinus rhythm R-wave amplitude(mV);and F=sinus rhythm S-wave amplitude(mV).The transition ratio was calculated in each leadwiththefollowingformula:[B/(B+C)VT÷E/(E+F)SR].
We hypothesized that a PVC/VT precordial transition to R>S at an interspace equal to or earlier than the location of the SR transition would suggest an LVOT origin,whereas a transition at an interspace later than the SR transition would suggest an RVOT origin.The sensitivity and specificity for this measure was assessed.
Results
Retrospective analysis
We identified 40 cases of successful OTVT ablation with lead-V3transition that met our inclusion criteria.The RVOT cohort consisted of 80%anteroseptal sites and 20%posteroseptal sites.The LVOT cohort consisted of 35%LCC,15%RCC,40%left-right coronary cusp junction,and 10%great cardiac vein near the anterior interventricular vein.
The R-wave amplitude was greater for LVOT compared with RVOT PVCs in leads V2(P<0.001)and V3(P<0.001).The R-wave duration ratio of the PVC to SR in lead V2(P=0.002)and lead V3(P=0.026)was also significantly greater for LVOT compared with RVOT PVCs.The V2transition ratio was significantly greater for LVOT(range 0.42 to 2.89)compared with RVOT origin(range 0.02 to 0.57)(P<0.001);however, the V3transition ratio was not significantly different be-tween PVCs of LVOT versus RVOT origin(P=0.093). The overall QRS duration was longer for LVOT compared with RVOT PVCs(P=0.048).
In a multivariate logistic regression,including R-wave duration in leads V1and V2,R-wave amplitude in leads V2and V3,and the R-wave transition ratio in lead V2,the V2R-wave transition ratio was the only independent predictor of PVC origin(P<0.001,95%CI: 0.01~0.41).
A V2transition ratio≥0.6 predicted an LVOT origin with a sensitivity of 95%and specificity of 100%. This cutoff yielded a positive predictive value of 100% and a negative predictive value of 95%.A more practical cutoff of≥0.5 yields a sensitivity of 95%and specificity of 95%.
The simple qualitative measure of PVC precordial transition(R>S)occurring at or before the SR transition (R>S)had a sensitivity of 47%and specificity of 64% for identifying an LVOT origin.However,a PVC precordial transition occurring later than the SR transition had a 19%sensitivity and 100%specificity for RVOT origin. Therefore,a PVC that transitions later than SR effectively rules out an LVOT origin.The surface ECGs of representative PVCs with lead V3R/S transition are illustrated adjacent to2their corresponding sinus beats in Figure 2.
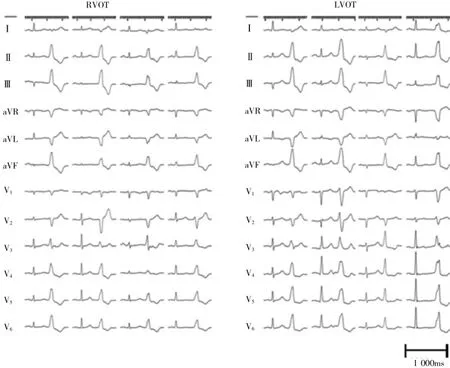
Figure 2Representative Outflow Tract PVC Surface ECG Recordings.The SR QRS and PVC morphologies from the retrospective cohort demonstrating the relatively earlier SR precordial transition in RVOT(left)compared with patients with LVOT PVC origin(right).The ECG speed:25 mm/s.Lead gain standardized to 1/16.
Prospective analysis
The ECG measurements of the ensuing 21 cases of OTVT who underwent successful RF ablation at our institution were performed.The algorithm was able to correctly predict the site of successful ablation(LVOT vs. RVOT)in 91%(19 of 21)of cases.With the simple qualitative measure alone,where LVOT origin is suggested by a PVC transition at or earlier than the SR transition,there was 71%accuracy in diagnosing the PVC origin.On the other hand,when the PVC transition occurred later than the sinus rhythm transition,anLVOT origin could be excluded with 100%accuracy.A proposed algorithm combining the qualitative and quantitative measures is shown in Figure 3.
Conclusions
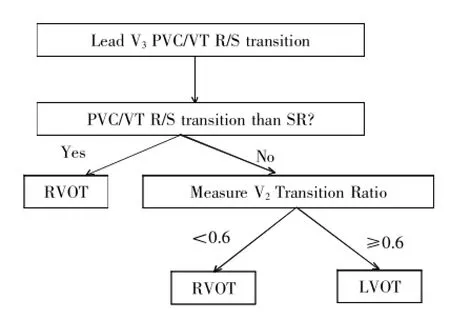
Figure 3Diagnostic Algorithm for Outflow Tract VT With Lead V3PVC/VT R/S Transition.If the PVC/ventricular tachycardia (VT)transition to an R>S occurs later than the SR transition (i.e.,SR transition lead V1or V2),then the PVC origin is the RVOT(100%specificity).If the PVC transition occurs at or earlier than the SR transition(i.e.,SR transition lead V3or later),then the V2transition ratio is measured.If the transition ratio is<0.6,then RVOT origin is likely.If the transition ratio is≥0.6,then LVOT origin is likely(sensitivity 95%, specificity 100%).
We present a novel electrocardiographic measure of the ratio of the VT and SR precordial transition,"the V2transition ratio,"which can reliably distinguish left from right outflow tract PVC/VT origin in patients with OTVT and lead V3precordial R/S transition.A V2transition ratio 0.6 predicts an LVOT origin with high sensitivity and specificity.A precordial transition later than the SR transition excludes an LVOT VT origin.
詞匯
transition n.過渡,臨時轉調,轉折語
heterogeneous adj.各種各樣的
infundibulum n.漏斗
cusps n.尖,尖點,牙尖
conducive adj.有助的
configuration n.配置,構形,輪廓
precordial adj.心前的
algorithm n.算法
abolished v.徹底廢除,取消,完全破壞
quadripolar n.四極
ensuing n.接著發生的,隨后的
注釋
1.accounting for在醫學文獻上常表達“校正”,“應對”之意,如Without accounting for stenosis interaction,the value of FFR for each stenosis would have been significantly overestimated.不校正狹窄之間的相互影響,每一狹窄的FFR值將被明顯高估。
2.adjacent to表示“接近”,“近…處”,“與…鄰近”,“毗連…”,當修飾名詞時,常放在被修飾名詞的后面,本文中放在句子后面,是因為PVC后有介詞短語修飾;也常放在動詞后面構成地點狀語,如Ventricular pacing was performed adjacent to the His bundle and proximal right bundle branch.于希氏束附近和右束支近端實施心室起搏。
參考譯文
第63課V2移行比率——鑒別左右心室流出道心動過速起源的新心電學標準
流出道室性心動過速(OTVT)是最常見的特發性室性心動過速(VT)。OTVT臨床表現各異,從單一的室性期前收縮(PVC)到反復短暫VT及持續性VT。
精細的心內電標測證實大多數OTVT起源于右室流出道(RVOT)前上間隔,位于肺動脈瓣下方。不常見的起源部位有右心室流出道漏斗部、右心室游離壁和后間隔部位。約10%~15%患者,心律失常起源于左心室流出道(LVOT),并可標測到主動脈竇部位。罕見的有經前間隔靜脈、主動脈-二尖瓣連接處或肺動脈根部消融的OTVT。
因為OTVT為局灶起源且發生于心臟結構正常患者,因此,這種心律失常特別有利于從12導聯心電圖定位。起源于右心室的OTVT典型的表現為額面電軸向下、呈左束支傳導阻滯(LBBB)圖形,且心前導聯R/S移行位于V3或V3以后。相反,LVOT VT通常表現為右束支傳導阻滯(RBBB)/電軸向下或LBBB/電軸向下而R/S移行位于V3或V3以前。
對于心前導聯移行位于V3的RVOT與LVOT,尚無鑒別標準。……

