Lesson Fifty-eight Is ST elevation in aVR a marker of LMCA or ostial LAD stenosis?
●心電學英語
Lesson Fifty-eight Is ST elevation in aVR a marker of LMCA or ostial LAD stenosis?
The lead aVR is oriented to'look'at the right upper side of the heart,and can provide specific information about the right ventricle outflow tract and basal part of the septum.Because of its location and the fact that it displays reciprocal information covered by leads aVL,Ⅱ,V5and V6,lead aVR is often ignored,even when considering complex ECGs.
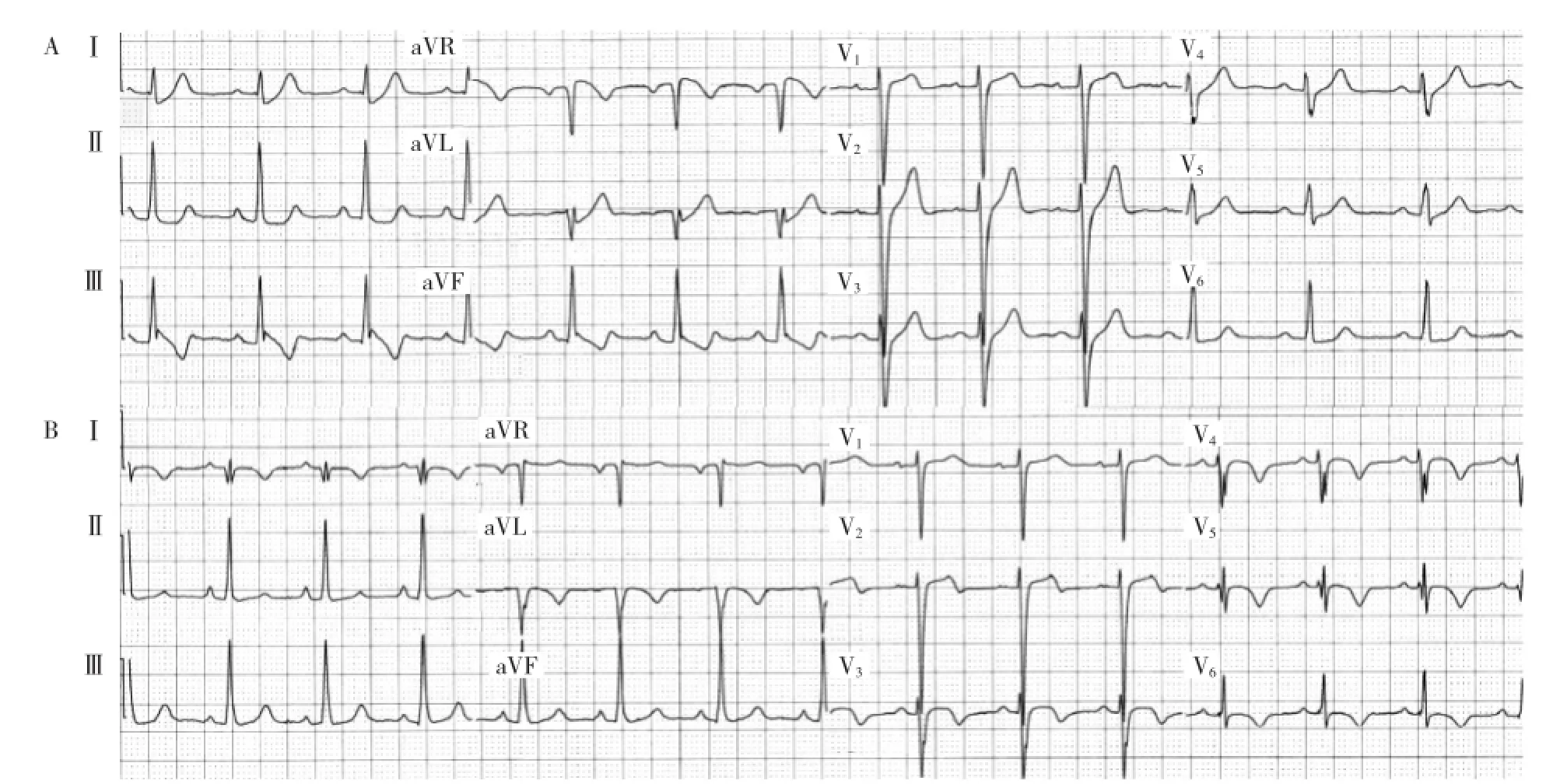
Figure 1Initial(A)and follow-up(B)electrocardiograms of a 44-year-old man presenting with chest heaviness and shortness of breath.Angiogram revealed a total proximal occlusion of the left anterior coronary artery without other significant disease.Note the ST elevation in aVR than V1.Also note the hyperacute T waves in the precardial leads and the ST abnormalities in the inferiolateral leads.
AcuteCoronarySyndromeandSTElevationinaVR
Studies by Engelen et al found that ST segment elevation in aVR strongly predicted LAD occlusion proximal to the first septal perforator(Figure 1).Yamaji et al observed that aVR ST segment elevation greater than the
ST segment elevation in V1predicts acute left main coronary artery(LMCA)occlusion with a sensitivity of
81%and a specificity of 80%(Figure 2).This finding also predicts clinical outcomes.Gaitonde et al demonstrated in a prospective study that in acute myocardial infarction,patients with an ST segment elevation that is greater in lead aVR than in lead V1prompted early angiography,withholding of clopidogrel and early referral to coronary artery bypass grafting,resulting in improved clinical outcomes1.
Kosuge et al found that in patients with non-ST segment elevation myocardial infarction,ST segment elevation of 0.5 mm or greater in aVR was a useful predictor of LMCA or three-vessel coronary artery disease(sensitivity 78%,specificity 86%)(Figure 3).Furthermore,they found that aVR ST segment elevation was the strongest predictor of adverse events at 90 days in patients with non-ST segment elevation myocardial infarction.Barrabes et al,in a study of 775 patients with theirfirst non-ST segment elevation myocardial infarction, showed that aVR ST segment elevation was associated with higher rates of in-hospital death,recurrent ischemia and heart failure.
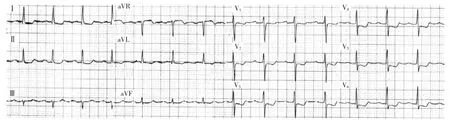
Figure 2Electrocardiogram of a 71-year-old woman presenting with chest pain.Angiogram revealed high-grade stenosis of the distal left main coronary artery involving the take-offs of the left anterior descending and circumflex coronary arteries.Note the ST elevation in aVR and the diffuse ST depressions.
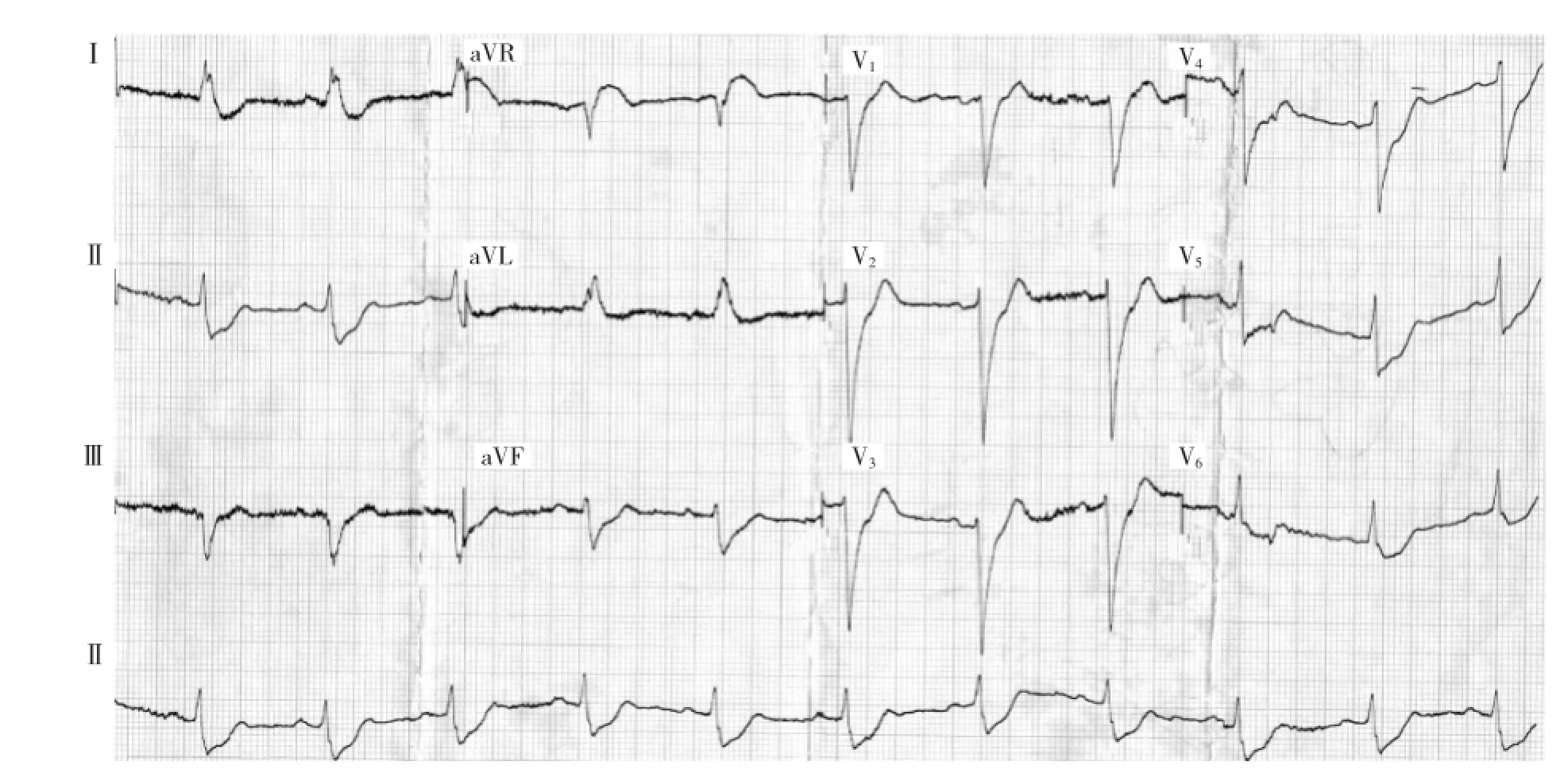
Figure 3Electrocardiogram of a 54-year-old man with chest pain and a history of coronary artery bypass surgery.Angiogram revealed an occluded left main coronary artery,a subtotal occlusion of the left anterior descending coronary artery after the anastamosis of left internal mammary artery,an ostial stenosis of saphenous vein graft to the obtuse marginal artery,and a diffuse moderate disease of the right coronary artery.Note the ST elevation in aVR and the ST depressions in the anterior and inferior leads.
Kotoku et al reported on the relationship between the ST segment level in lead aVR and the length of the LAD.ST segment levels(especially in leadsⅡand V6),the site of LAD occlusion and the length of the LAD affect the ST segment level in lead aVR in patients with a first ST elevation acute anterior wall myocardial infarction.Proximal LAD occlusion is associated with ST segment elevation in lead aVR,while a long LAD occlusion is associated with ST segment depression in lead aVR.Kotoku et al also reported that a prominent Q wave in lead-aVR in anterior wall acute myocardial infarction is related to severe regional wall motion abnormality in the apical and inferior regions,with an LAD wrapping around the apex2.
LMCA occlusion is another clinical situation in which prompt diagnosis by the clinician can help initiate life-saving invasive therapy.The typical electrocardiographic finding in patients with preserved flow through the LMCA is widespread ST segment depression maximally in leads V4to V6,with inverted T waves and ST segment elevation in lead aVR.ST elevation in lead aVR,when accompanied by either anterior ST elevationor widespread ST segment depression,may indicate LMCA occlusion.Figure 4 showed ECG changes of complete ostial occlusion of LMCA determined by emergent angiography.The ECG shows marked ST elevation in aVR>>V1and ST depression in multiple leads(V2~V6,Ⅰ,Ⅱ,aVL,aVF).
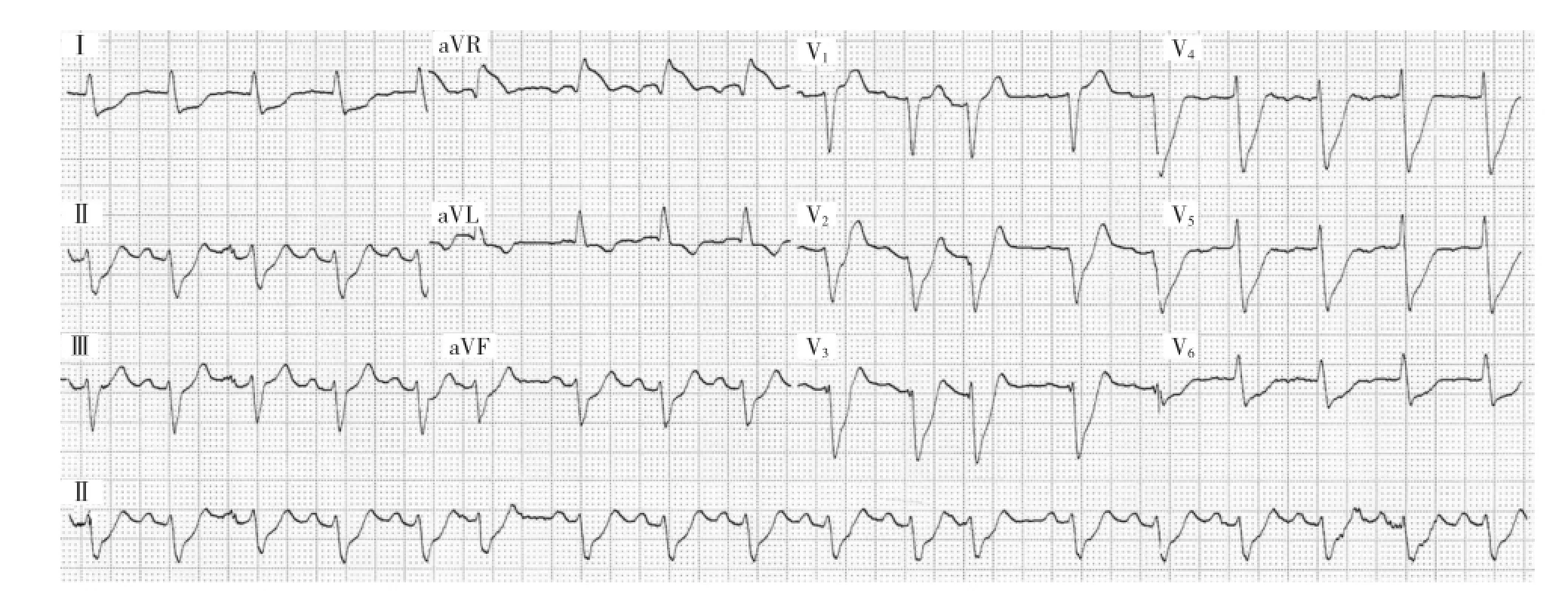
Figure 4This patient presented to ED with severe ischaemic chest pain,vomiting,syncope(due to runs of VT)and cardiogenic shock.He was taken for emergent angiography and found to have a complete ostial occlusion of left main coronary artery.
Kanei et al reported in a study of 106 patients that ST segment depression in lead aVR in inferior wall ST segment elevation myocardial infarction predicts left circumflex infarction or larger right coronary artery infarction involving a large posterolateral branch.
Stress Testing and ST Elevation in aVR
Data regarding the significance of STE in lead aVR in the setting of exercise treadmill testing(ETT)are limited.In the present study,Uthamalingam S et al tested the hypothesis that ETT-induced STE in lead aVR is a useful indicator of hemodynamically significant LMCA or ostial LAD stenosis.
A database search of patients undergoing cardiac catheterization at his institution between January 2008 and July 2009 was performed to identify 3 groups of patients∶1)those with significant LMCA or ostial LAD disease(≥50%luminal diameter reduction)in addition to any other coronary lesions(≥70%luminal diameter reduction for mid and distal LAD segments);2)those with coronary artery disease(CAD)(≥70%luminal diameter reduction)but not LMCA or ostial LAD disease;and 3)those free of significant CAD(LMCA and all 3 major vessels free of any stenosis≥50%). Ostial LAD stenosis included any lesion proximal to the first septal perforator.All patients(n=454)had undergone ETT according to the standard Bruce protocol≤6months beforetheclinicallyindicatedcardiac catheterization.LMCA(n=38)or ostial LAD stenosis(n=42)was present in 75 patients(5 patients had both).The remainder had either CAD of varying severity that did not involve the LMCA or ostial LAD(n= 276)or no significant CAD(n=103).
Patients with acute coronary syndromes or prior coronary artery bypass grafting were excluded.Patients who had undergone pharmacological stress also were excluded,as were those whose baseline ECG studies indicated left bundle branch block,intraventricular conduction delays≥120ms,left ventricular hypertrophy with marked strain pattern(down-sloping ST-segment depression[STD]≥1 mm with biphasic or inverted T waves),or marked anterior T-wave inversions(the Wellens pattern3)concerning for active ischemia or possible LMCA or proximal LAD stenosis.
ECG data(rest and stress)
In addition to lead aVR,lead aVL,the inferior leads(Ⅱ,Ⅲ,and aVF),and pre-cordial leads V1and V4to V6were evaluated,and the amount of STD or STE at 80 ms after the J point both at rest and during peak stress was tested in univariate regression analysis.In lead aVR,only horizontal or up-sloping STE was con-sidered indicative of ischemia.J-point elevation only with down-sloping ST segment was not.
Univariate logistic regression analysis was performed of patients with 1VD,2VD,and 3VD without LMCA or ostial LAD stenosis to determine the correlation of each with STE in lead aVR.There was no significant correlation between 1VD,2VD,or 3VD without LMCA or ostial LAD stenosis and STE in lead aVR.In contrast,STE in lead aVR was a significant(P<0.0001,AUC∶0.76)positively correlated predictor of selected cases of pure,isolated LMCA or ostial LAD stenosis(n=34).Because leads V5and V6are reciprocal to lead aVR,STD in either of these leads as a univariate predictor of LMCA or ostial LAD stenosis was determined.Although both were correlated strongly(lead V5:P<0.0001,AUC∶0.69;lead V6:P<0.0001,AUC:0.70),the AUC for each was significantly less than that for STE in lead aVR(0.82)(both P<0.001).Finally, although stress-induced STE in lead V1was also a significant predictor of LMCA or ostial LAD stenosis(P<0.0001,AUC∶0.59)it too was significantly less than that for STE in lead aVR(P<0.0001 for AUC comparison)and did not add independent information in multivariate analysis.
Using a cut-point of 1-mm STE in lead aVR, chi-square tests were used to compare the prediction of LMCA or ostial LAD stenosis with 1VD,2VD,and 3VD without LMCA or ostial LAD stenosis.Thus,76%of patients with LMCA or ostial LAD stenosis had 1-mm STE in lead aVR with stress,compared with 17%,27%,and 39%,respectively,with 1VD,2VD,and 3VD without LMCA or ostial LAD stenosis Only 8 patients(8%)without significant CAD had 1-mm STE in lead aVR with stress.
Optimal ECG lead aVR cut-point and Bayesian analysis
The optimal cut-point for the amount of stress-induced STE in lead aVR was defined by the greatest sum of sensitivity and specificity for the detection of significant LMCA or ostial LAD stenosis.Cut-points of 0.5-, 1.0-,1.5-,and 2.0-mm horizontal STE were tested. The greatest sensitivity-specificity sum(1.56)was reached at 1.0-mm STE.Thus,sensitivity was 75%, specificity was 81%,positive predictive accuracy was 44%,negative predictive accuracy was 94%,and overall predictive accuracy was 80%.
詞匯
ignore v.忽視,不顧,不理會,駁回
withhold v.克制,使...停止,把...留下,拒給
wrap n.&v.包裹物,包裝,披肩,毯子,外衣;包,包上,包扎,纏繞,覆蓋,用...包
circumflex adj.&v.音調符號的,卷曲的,彎曲的;使...彎曲
univariate adj.單變量的
logistic n.&adj.算術;邏輯的,計算的
注釋
1.句子“Gaitonde et al demonstrated…prompted early angiography,withholding of clopidogrel and early referral to coronary artery bypass grafting,resulting in improved clinical outcomes.”中,“withholding”是動名詞作prompted的賓語,而“resulting…”是分詞短語用作伴隨狀語。
2.句子“Kotoku et al also reported…the apical and inferior regions,with an LAD wrapping around the apex.”中的“wrapping…”分詞短語是with賓語“LAD”的補語,而“with…”整個介詞短語是“anterior wall acute myocardial infarction”的名詞修飾語。
3.Wellens pattern指前降支嚴重狹窄的特異性心電圖表現,V2~V3上出現對稱性T波深倒置(>2mm)(A型Wellens T波),或T波呈先正后負的正負雙相改變(B型Wellens T波)。
參考譯文
第58課aVR ST段抬高是左冠狀動脈主干或前降支開口狹窄的特征嗎?
aVR面對心臟右上方,可提供右心室流出道和間隔基底部的特別信息。由于它的位置及其顯示的信息與aVL、Ⅱ、V5和V6所覆蓋的彼此相反,因此,即使分析復雜的心電圖時,也常常忽視aVR。
急性冠狀動脈綜合征與aVR ST段抬高
Engelen等研究發現aVR ST段抬高強烈預示前降支(LAD)阻塞部位位于第一穿間隔支之前(圖1)。Yamaji等觀察到aVR ST段抬高超過V1預測急性左冠狀動脈主干(LMCA)阻塞的敏感性為81%,特異性為80%(圖2)。這種表現還能預測臨床預后。Gaitonde等在一前瞻性研究中證實,急性心肌梗死時aVR ST段抬高超過V1者,促使早期造影、停用波利維及早期轉向冠狀動脈搭橋術,結果是臨床預后得到改善。
Kosuge等發現非ST段抬高患者aVR ST段抬高0.5mm或以上是LMCA或多支冠狀動脈病變的有效預測指標(敏感性78%,特異性86%)(圖3)。此外,他們發現aVR ST段抬高是非ST段抬高心肌梗死患者90d不良事件的最強預測指標。Barrabes等對775例首次發生非ST段抬高心肌梗死患者的研究表明,aVR ST段抬高患者的住院死亡、再發心肌缺血及心力衰竭發生率較高。

