前置胎盤產婦合并胎盤植入危險因素及對產婦與新生兒的影響
曹殿玲
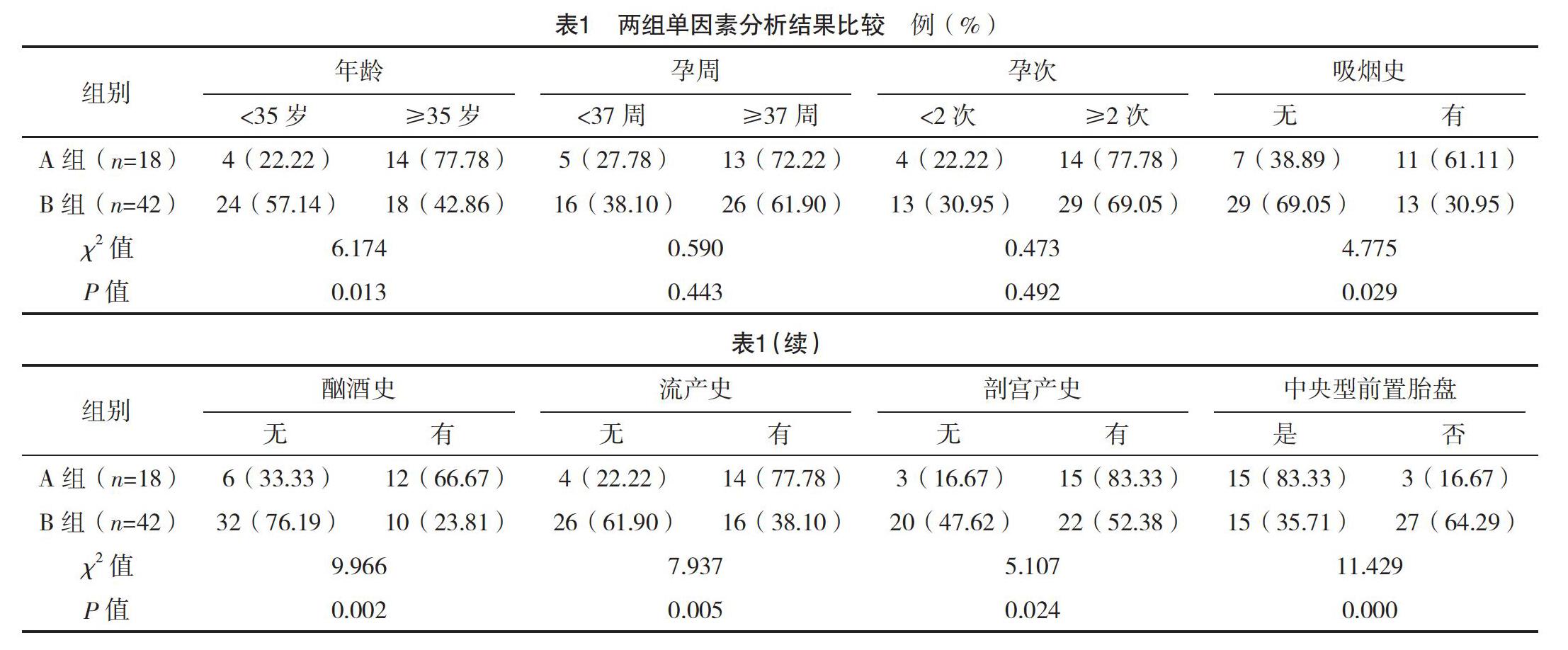
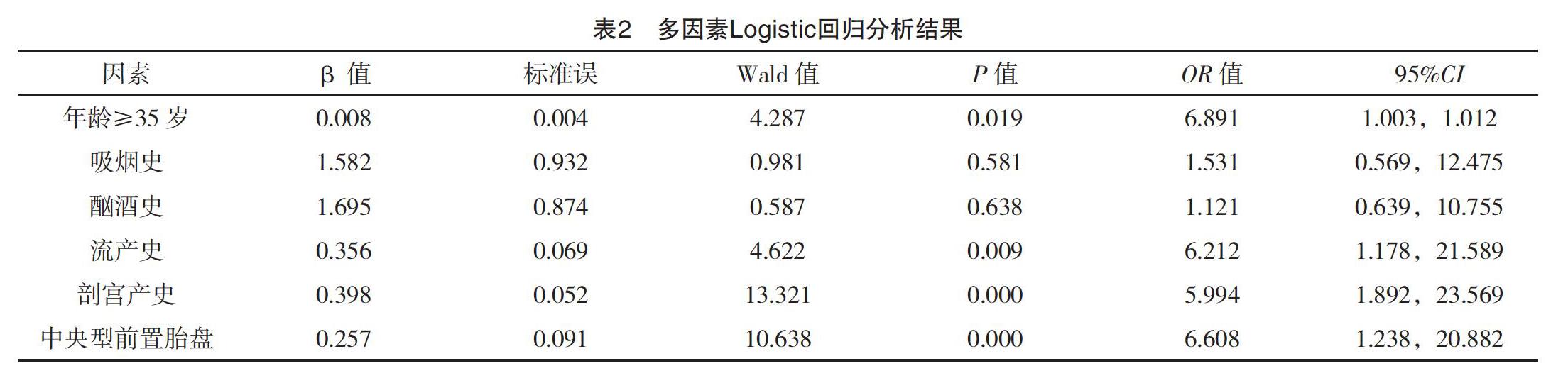
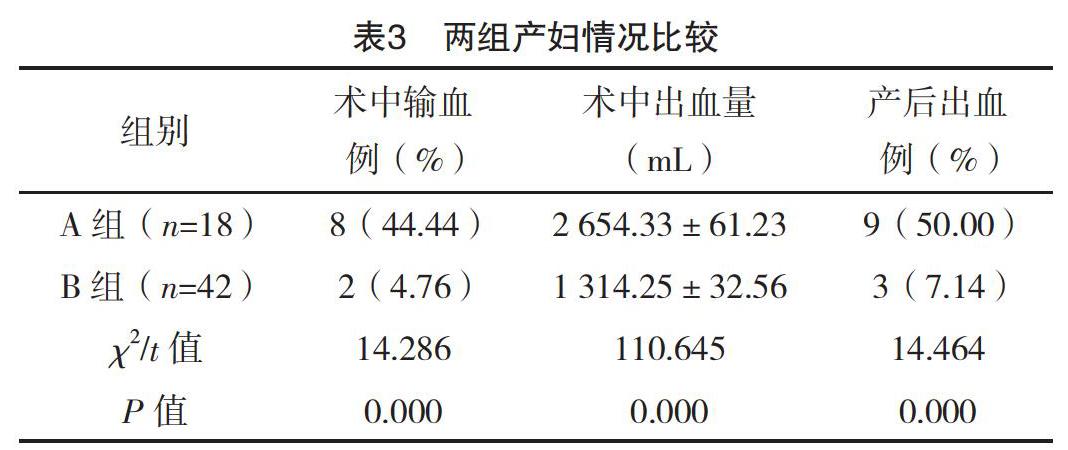
【摘要】 目的:分析前置胎盤產婦合并胎盤植入危險因素及對產婦與新生兒的影響。方法:選取本院2015年1月-2018年11月產科收治的60例前置胎盤產婦作為觀察對象,對其臨床資料進行回顧性分析。對所有產婦年齡、吸煙史、酗酒史、流產史、剖宮產史、前置胎盤類型等進行分析。根據是否合并胎盤植入分為A、B組,A組(n=18)發生胎盤植入,B組(n=42)未發生胎盤植入。對兩組產婦情況及新生兒情況進行分析。結果:兩組年齡、吸煙史、酗酒史、流產史、剖宮產史及前置胎盤類型比較,差異均有統計學意義(P<0.05),但兩組孕周、孕次比較,差異均無統計學意義(P>0.05)。多因素分析結果顯示,年齡≥35歲、流產史、剖宮產史及中央性前置胎盤是合并胎盤植入的獨立危險因素(P<0.05);A組產婦術中輸血率、產后出血率及術中出血量均高于B組,差異均有統計學意義(P<0.05);A組新生兒窒息率(44.44%)與早產率(27.78%)均高于B組的4.76%、0,差異均有統計學意義(P<0.05)。A組新生兒1 min Apgar評分(7.02±0.42)分、出生體重(3.07±0.47)kg均低于B組的(8.32±0.88)分、(3.99±0.89)kg,差異均有統計學意義(P<0.05)。結論:前置胎盤嚴重威脅產婦及新生兒安全,合并胎盤植入與年齡、流產史、剖宮產史、中央性前置胎盤存在密切的關聯,合并胎盤植入后,產婦和新生兒風險均明顯增加。
【關鍵詞】 前置胎盤 胎盤植入 危險因素
[Abstract] Objective: To analyze the risk factors of placenta previa combined with placental implantation and its influence on the pregnant women and newborns. Method: The clinical data of 60 pregnant women with placenta previa admitted to the obstetrics department of our hospital, from January 2015 to November 2018 were retrospectively analyzed. The age, smoking history, alcoholism history, abortion history, cesarean section history and type of placenta previa were analyzed. According to the combination of placental implantation or not, they were divided into group A and B. Placental implantation occurred in group A (n=18) and no placental implantation occurred in group B (n=42). The parturient and neonatal condition of two groups were analyzed. Result: There were significant differences in age, smoking history, alcohol abuse history, abortion history, cesarean section history and placenta previa type between the two groups (P<0.05). However, there were no statistically significant differences in gestational weeks and gestational times between the two groups (P>0.05). Multivariate analysis showed that age≥35 years, history of abortion, cesarean section and central placenta previa were independent risk factors for placental implantation (P<0.05). The intraoperative blood transfusion rate, postpartum hemorrhage rate and intraoperative hemorrhage volume in group A were higher than those in group B, the differences were statistically significant(P<0.05). The neonatal asphyxia rate (44.44%) and premature delivery rate (27.78%) in group A were higher than 4.76%, 0 in group B, the differences were statistically significant(P<0.05). The 1 min Apgar score (7.02±0.42) scores and birth weight (3.07±0.47) kg in group A were lower than (8.32±0.88) scores, (3.99±0.89) kg in group B, the differences were statistically significant(P<0.05). Conclusion: Placenta previa is a serious threat to maternal and neonatal safety, placenta previa combined with placenta implantation is closely related to age, abortion history, cesarean section history and central placenta previa, after placenta implantation, maternal and neonatal risks increase significantly.
[2]曾義,李杰,段光友,等.再次剖宮產產后出血危險因素分析:2442例產婦的回顧性研究[J].第三軍醫大學學報,2019,41(3):265-269.
[3]劉芳,羅瑋.伴瘢痕子宮的前置胎盤產婦手術情況及新生兒結局觀察[J].中外醫學研究,2018,16(32):8-10.
[4]黨志霞.胎盤植入產婦相關危險因素及結局分析[J].中外醫療,2018,37(31):43-45.
[5]蔡本碩,杜鵑.某醫院前置胎盤患者術中出血相關因素的回顧性分析[J].東南大學學報(醫學版),2018,37(5):908-911.
[6]吳爭勇,劉麗群.彩超診斷中央性前置胎盤并胎盤植入的臨床分析[J].現代診斷與治療,2018,29(20):3253-3254.
[7]陳陶玲,李銀華,張小英.產前超聲檢查在前置胎盤及植入孕婦分娩大出血預測中的臨床應用價值[J/OL].心電圖雜志(電子版),2018,7(3):27-30.
[8]楊凱樂,劉展,謝菲,等.前置胎盤并胎盤植入的高危因素及對妊娠結局的影響[J].實用預防醫學,2018,25(9):1105-1107.
[9]郭吉敏,曹滿瑞,劉小平,等.MRI征象回歸模型在植入型兇險性前置胎盤的應用[J].臨床放射學雜志,2018,37(8):1325-1328.
[10]劉冬紅,李華麗,李維玲.前置胎盤伴胎盤植入術中應用宮頸COOK雙球囊及卡前列素氨丁三醇防治產后出血療效觀察[J].中國計劃生育學雜志,2018,26(8):731-733.
[11]覃獻珍.導致中央型前置胎盤剖宮產后出血的危險因素分析[J].世界最新醫學信息文摘,2018,18(66):35.
[12] Karami M,Jenabi E,Fereidooni B.The association of placenta previa and assisted reproductive techniques:a meta-analysis[J].The Journal of Maternal-Fetal & Neonatal Medicine,2017:1-18.
[13]薛曉玲.前置胎盤合并剖宮產史患者產后大出血危險因素研究[J].中外女性健康研究,2018(12):84,87.
[14]邱文山,黎法文,林小蘭,等.90例兇險性前置胎盤的回顧性研究及危險因素分析[J].廣東醫科大學學報,2018,36(2):211-213.
[15]李玉梅,楊文才,陳健聰,等.一站式球囊封堵術輔助中央性前置胎盤剖宮產術的護理路徑管理[J].實用醫院臨床雜志,2018,15(3):125-127.
[16]王恒宇,何明祥,漆洪波.兇險性前置胎盤腹主動脈球囊阻斷下剖宮產術子宮切除的相關影響因素及母嬰結局研究[J].醫學信息,2018,31(8):49-52.
[17]張力維,李青,齊淑琴,等.前置胎盤伴胎盤植入危險因素分析及宮頸子宮下段環形縫合術對母嬰結局的影響[J].中國現代醫生,2018,56(6):56-59.
[18] Feng Y,Li X Y,Xiao J,et al.Risk Factors and Pregnancy Outcomes:Complete versus Incomplete Placenta Previa in Mid-pregnancy[J].Current Medical Science,2018,38(4):597-601.
[19]連旭波,韋春杏.妊娠期兇險型前置胎盤的核磁共振成像診斷價值與妊娠結局的關系[J].中國計劃生育和婦產科,2018,10(1):28-31.
[20]石巍.子宮破裂及前置胎盤與瘢痕子宮再妊娠患者剖宮產產后出血的關聯性分析[J].內蒙古醫學雜志,2017,49(12):1436-1438.
[21]李娟,付金紅,張慧娟,等.兇險性前置胎盤植入原因及母嬰結局的影響回顧性研究[J].河北醫藥,2017,39(23):3575-3578.
[22]王志英.前置胎盤導致選擇性剖宮產產婦大出血的影響因素研究[J].中外女性健康研究,2018(12):73-75.
[23]董南,胥琪琪,葉敏清,等.兇險型前置胎盤狀態伴胎盤植入中期妊娠引產一例[J/OL].中華產科急救電子雜志,2018,7(1):54-57.
(收稿日期:2019-06-10) (本文編輯:田婧)