肺生殖細胞瘤伴骨轉移一例報告
孫紅瑩 孫紅芳 孫莉 李明嫻
病例資料
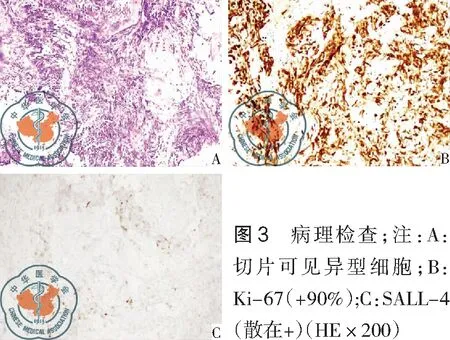
患者,男,17歲,因“間斷咳嗽半個月,加重伴發熱、左側胸痛3 d”入院。患者半個月前著涼后出現咳嗽、咳痰,偶伴有活動后氣短,3 d患者無明顯誘因咳嗽癥狀加重,并出現左側胸痛,伴有發熱。入院查體:體溫37.2 ℃,血壓120/70 mmHg,呼吸20次/min,脈搏90次/min,神清語明,皮膚鞏膜無黃染,全身淺表淋巴結未觸及,聽診雙肺呼吸音粗,左下肺可聞細小濕啰音,心臟及腹部查體未見異常。輔助檢查,肺部CT:左肺下葉支氣管截斷,局部可見團塊狀軟組織密度影約6cm,縱隔、左肺門淋巴結腫大,見圖1;甲胎蛋白(AFP) 41.39 ng/ml;PET-CT:左肺下葉支氣管開口處高代謝腫塊,SUV最大值8.9,CT值30.7 Hu,考慮中心型肺癌,伴遠端阻塞性肺不張及阻塞性炎癥;左肺門及縱膈(7組)淋巴結轉移癌;第8胸椎、第4腰椎、左側第8肋骨、左側髂骨轉移癌,SUV最大值8.9。血常規:白細胞10.09×109/L,中性粒細胞百分比0.81,中性粒細胞絕對值8.20×109/L;超敏C反應蛋白77.10 mg/L;纖維支氣管鏡檢查:鏡下管腔內未見新生物,但左肺下葉支氣管管腔閉塞,開口處黏膜粗糙、充血、水腫、質軟,觸之易出血,見圖2,取細胞沖洗液及支氣管刷片送檢,并于左下肺支氣管開口處經支氣管壁穿刺活檢,均找到癌細胞,傾向生殖細胞瘤,免疫組化表達顯示:Ki-67(+70%)CK-pan(±),CD20(-),CD3(-),SALL4(+),CD117(NS),PLAP(-),Oct3/4(-),重復CD117(-),CD30(-),AFP(-),HMB45(-),Vimentin(-)。由于免疫組化表達不典型,3 d后再行支氣管鏡檢查并送檢病理,病理結果:結合免疫組化符合生殖細胞瘤;免疫組化:Ki-67(+90%),CK-pan(±),TTF-1(-),CK7(-),CK5/6(-),P63(±),CD56(-),CgA(-),Syn(-),SALL4(散在+),Oct3/4(-),見圖3。

圖1 肺CT:左肺下葉支氣管截斷,局部可見團塊狀軟組織密度影,大小約6 cm,CT值為33 HU;縱隔、左肺門淋巴結腫大

圖2 纖維支氣管鏡檢查:左肺下葉開口粘膜粗糙,充血,水腫,管腔閉塞
討 論
生殖細胞瘤是由3種原始胚層細胞演變而來的胚胎性腫瘤,在胚胎期,生殖細胞起源于卵黃囊的內胚層,沿著原腸后端中線附近遷移,至后腹壁生殖嵴聚集后并入發育中的生殖腺,通常于胚胎后期降入女性盆腔或男性陰囊。若部分生殖細胞在遷移過程中落后或超前,移位到其它器官,沒有退化的生殖細胞便保留了分化潛能,可能發生腺外生殖細胞瘤。腺外生殖細胞癌常見發生于松果體、鞍上池、縱隔、腹膜后、骶尾部等部位。兒童中惡性生殖細胞腫瘤發病率低,年發病率約為2.4/100萬,多發于男性青少年,占兒童惡性腫瘤的2.9%[1-7]。惡性生殖細胞瘤多為實質性,腫塊多數邊界不清,易向周圍結構浸潤及侵犯,較早地出現遠處轉移。
肺是惡性生殖細胞瘤最常見轉移部位,但原發的肺生殖細胞瘤罕見。本例患者臨床表現不典型,肺部CT表現與中央型肺癌類似,以咳嗽、發熱、胸痛等阻塞性肺炎的癥狀為首發,無明顯癥狀時即發生多處骨轉移,診斷較為困難,容易誤診。AFP是一種胎兒蛋白,生理性的AFP合成于卵黃囊、胚胎肝臟和胃腸道[3]。血清中甲胎蛋白水平升高是惡性生殖細胞瘤的重要生化指標[9-14]。該患者甲胎蛋白水平升高,更支持了肺生殖細胞瘤的診斷。
肺部生殖細胞瘤極為罕見,影像學缺乏特異性,診斷主要依靠病理檢查,因此,對于以肺部占位及甲胎蛋白升高主要表現的男性患者、特別是青少年,應考慮到生殖細胞瘤可能,并行病理學檢查以確診。
1 湯靜燕, 李志光. 兒童腫瘤診斷治療學[M]. 北京: 人民軍醫出版社, 2011: 6.
2 Rossig C, Juergens H, Schrappe M, et al. Effective childhood cancer treatment: the impact of large scale clinical trials in Germany and Austria[J]. Pediatr Blood Cancer, 2013, 60(10): 1574-1581.
3 Brecht IB, Bremensdorfer C, Schneider DT, et al. Rare malignant pediatric tumors registered in the German Childhood Cancer Registry 2001-2010[J]. Pediatr Blood Cancer, 2014, 61(7): 1202-1209.
4 Samuelsson BO, Ridell B, R?ckert L, et al. Non-Hodgkin lymphoma in children: a 20-year population-based epidemiologic study in western Sweden[J].J Pediatr Hematol Oncol, 1999, 21(2): 103-110.
5 Winkler K, Bieling P, Bielack S, et al. Local control and survival from the Cooperative Osteosarcoma Study Group studies of the German Society of Pediatric Oncology and the Vienna Bone Tumor Registry[J]. Clin Orthop Relat Res, 1991, (270): 79-86.
6 Neth O, Seidemann K, Jansen P, et al. Precursor B-cell lymphoblastic lymphoma in childhood and adolescence: clinical features, treatment, and results in trials NHL-BFM 86 and 90[J]. Med Pediatr Oncol, 2000, 35(1): 20-07.
7 Lukens JN. Progress resulting from clinical trials. Solid tumors in childhood cancer[J]. Cancer, 1994, 74(9 Suppl): 2710-2718.
8 邢建軍, 苗陽. 血清甲胎蛋白在腫瘤鑒別診斷中的意義[J]. 中國實用醫藥, 2014, 9(20): 242-243.
9 Drozynska E, Bien E, Polczynska K, et al. A need for cautious interpretation of elevated serum germ cell tumor markers in children. Review and own experiences[J]. Biomark Med, 2015, 9(9): 923-932.
10 Schneider DT, Calaminus G, G?bel U. Diagnostic value of alpha 1-fetoprotein and beta-human chorionic gonadotropin in infancy and childhood[J]. Pediatr Hematol Oncol, 2001, 18(1): 11-26.
11 Kobayashi T, Kawakita M, Terachi T, et al. Significance of elevated preoperative alpha-fetoprotein in postchemotherapy residual tumor resection for the disseminated germ cell tumors[J]. J Surg Oncol, 2006, 94(7): 619-623.
12 Beck SD, Foster RS, Bihrle R, et al. Significance of primary tumor size and preorchiectomy serum tumor marker level in predicting pathologic stage at retroperitoneal lymph node dissection in clinical Stage A nonseminomatous germ cell tumors[J]. Urology, 2007, 69(3): 557-559.
13 Kim A, Ji L, Balmaceda C, Diez B, et al. The prognostic value of tumor markers in newly diagnosed patients with primary central nervous system germ cell tumors[J]. Pediatr Blood Cancer, 2008, 51(6): 768-773.
14 G?bel U, Calaminus G, Schneider DT, et al. Management of germ cell tumors in children: approaches to cure[J]. Onkologie, 2002, 25(1): 14-22.