活體供腎移植急性排斥反應發生與供受者年齡的關系
王 振,錢葉勇,李 昆,柏宏偉,李 鋼,范 宇,劉路鵬,常京元,石炳毅
解放軍第309醫院 全軍器官移植研究所泌尿二科,北京 100091
活體供腎移植急性排斥反應發生與供受者年齡的關系
王 振,錢葉勇,李 昆,柏宏偉,李 鋼,范 宇,劉路鵬,常京元,石炳毅
解放軍第309醫院 全軍器官移植研究所泌尿二科,北京 100091
目的探討活體供腎移植受者發生急性排斥反應(acute rejection,AR)的年齡因素。方法對本移植中心2006年1月-2013年12月327例行活體供腎腎移植受者隨訪,供者年齡≥55歲定義為老年供者,受者年齡<30歲定義為年輕受者。記錄供、受者的臨床基線特征;移植后第1、3、6、12、24、36、48、60個月均行隨訪,內容包括基本體格檢查、病史、實驗室檢查、AR發病情況。應用單因素和Cox比例風險模型進行多因素分析,確定AR發病危險因素。結果AR組隨訪時間為(35.9±13.2)個月,非AR組為(36.3±15.4)個月;腎移植術后受者前3個月內AR的發生率為7.3%(24/327)。AR組血肌酐水平、尿蛋白發生率高于同時間非AR組(P<0.05)。多因素分析顯示,老年供者年輕受者是AR的獨立危險因素,相對危險度(relative risk,RR)為3.67(95% CI:2.61 ~ 4.58,P=0.002)。結論接受老年供腎的年輕受者是AR的獨立危險因素。
老年人(55歲);免疫原性;急性排斥反應;腎移植;活體供腎
親屬活體器官捐獻供腎移植作為家庭自救的主要方式,成為治療尿毒癥的最有效手段[1]。研究表明,接受老年供腎的腎移植受者效果不佳,然而供腎者的年齡是一個固定的變量[2-3]。因此,針對其他引發腎功能損傷的危險因素并給予針對性的防治,是提高老年供者活體供腎移植效果的關鍵[4]。急性排斥反應(acute rejection,AR)引起移植腎急性損害,嚴重影響移植腎存活。減少AR發生,對于提高老年供腎移植的移植效果至關重要[5-6]。本研究對327例腎移植受者進行長期隨訪,描述其急性排斥反應發病情況,探討年齡與AR的關系,旨在為改善腎移植受者預后、提高活體移植效果提供依據。
對象和方法
1 研究對象 納入對象為我中心2006年1月-2013年12月所行327例活體供腎、成人首次腎移植供受者。所有受者依據排斥反應分為排斥組和非排斥組。老年供者的定義:供腎者年齡≥55歲,年輕受者的定義:移植受者年齡<30歲。依據供受者年齡分為以下4組:老年供腎給年輕受者組,老年供腎給正常受者(>30歲)組,正常供腎給正常受者組,正常供腎給年輕受者組。本研究獲得醫院倫理委員會的批準,均鑒定知情同意。
2 免疫治療 所有腎移植受者根據群體反應性抗體(panel reaction antibody,PRA)水平,接受CD25單克隆抗體誘導治療、兔抗胸腺細胞球蛋白(rabbit antithymocyte globulin,rATG)誘導治療方案或無誘導治療方案。術后維護免疫抑制劑為常規三聯用藥,包括鈣調磷酸酶抑制劑(環孢素或他克莫司)、抗增殖類藥物(霉酚酸酯或硫唑嘌呤)、聯合規律減量的類固醇激素。
3 研究方法 在腎移植術時完成所有供受者的人口學資料和病史資料收集,包括供體的年齡、性別、體質量指數(body mass index,BMI)和腎小球濾過率(glomerular filtration rate,GFR),受者的年齡、性別、透析時間、PRA、BMI以及冷缺血時間、熱缺血時間、人類白細胞抗原不匹配數(HLA mismatched,HLA MM)、供體腎動脈數目和免疫抑制方案。收集的所有數據均以電子文檔形式記錄在中國腎移植科學登記系統。研究的首要終點是移植術后前3個月排斥反應發生情況,分別行單因素和多因素分析,從而確定親屬活體供腎腎移植AR的危險因素。
4 隨訪 AR組采用類固醇激素還是rATG治療取決于生化和臨床反應。以行腎移植時間為起點,隨訪于2013年12月截止。隨訪大多為門診隨診,少部分輔以住院復查。隨訪內容:基本體格檢查、病史詢問、實驗室檢查、AR發病情況。
結 果
1 隨訪情況 AR組隨訪時間為(35.9±13.2)個月,非AR組為(36.3±15.4)個月;兩組差異無統計學意義(P>0.05)。術后3個月內,24例受者發生AR,發生率為7.3%。根據“Banff 2003”分級標準,23例受者AR為I級,經治療后AR逆轉;1例受者AR為Ⅲ級,經治療后無效而行移植腎切除;無受者死亡。
2 各組腎功能比較 AR組供者GFR為(43.3±12.0) ml/ (min·1.73 m2),非AR組供者為(43.5±11.9) ml/(min· 1.73 m2),差異無統計學意義(P=0.94)。非AR組受者移植術后6個月、12個月、24個月和36個月的血肌酐水平低于同時間的AR組受者水平(P<0.05,圖1A)。AR組受者移植術后1年、2年和3年的蛋白尿發生率高于非AR組受者(P<0.05,圖1B)。
3 AR危險因素的單因素分析 兩組受者的年齡、性別比和BMI無統計學差異。兩組受者的移植相關指標,如HLA錯配數、冷缺血時間、熱缺血時間、PRA、供腎動脈數目、供腎摘取術式(開放取腎vs后腹腔鏡下供腎摘取)和免疫抑制方案,差異無統計學意義。兩組供者的人口學特征,包括年齡、性別比和BMI,差異無統計學意義。見表1。
4 供受者年齡與AR的關系 中老年供者的AR發生率為15.2%,高于年輕供者AR發生率(6.0%);兩者差異無統計學意義(P=0.059)。年輕受者的AR發生率為9.5%,正常年齡受者AR發生率為4.3%,兩者差異無統計學意義(P=0.088)。老年供者年輕受者的AR發生率為20.1%,與其他3組相比有統計學差異(P=0.023)。見表2。
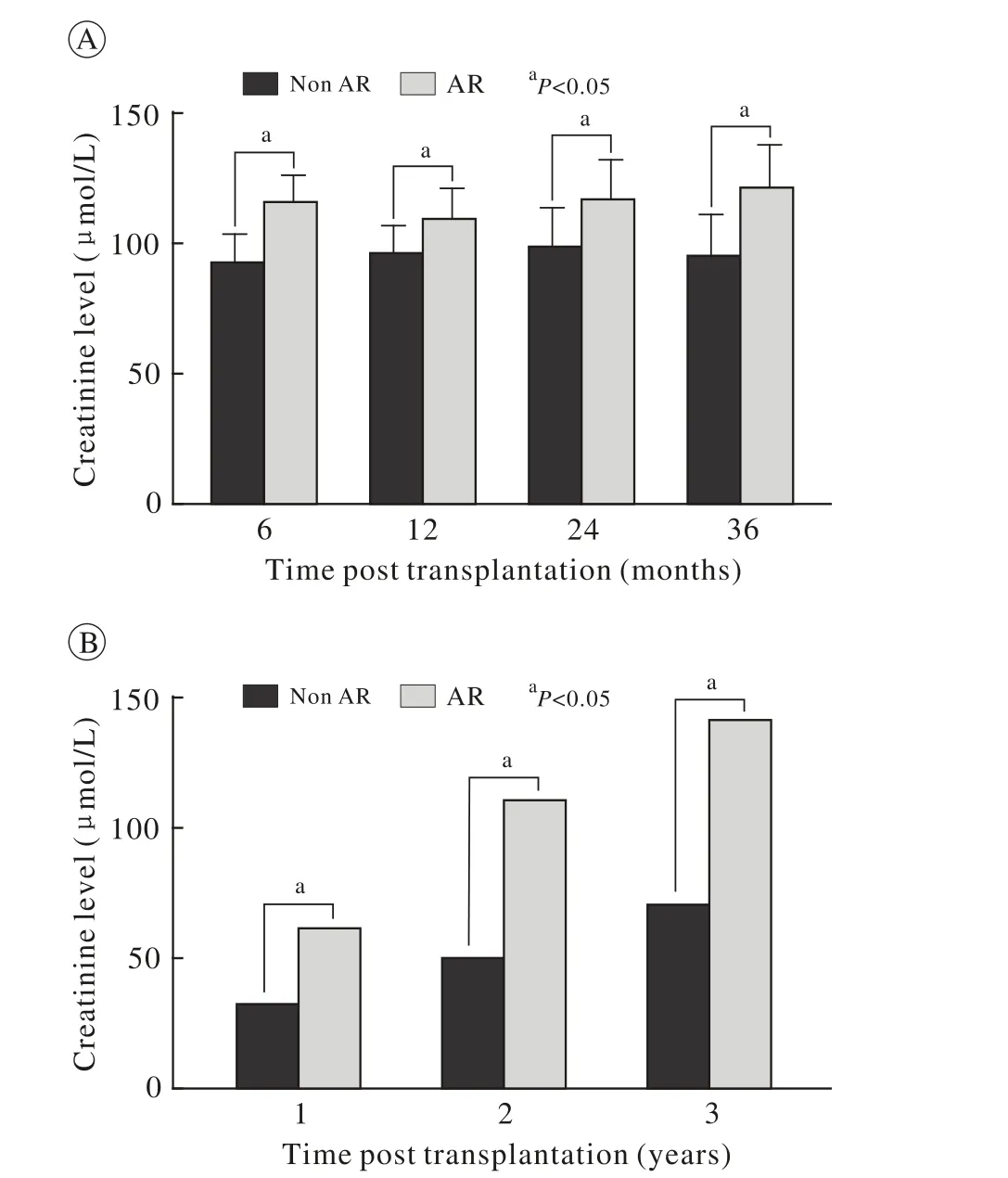
圖 1 AR組和非AR組平均血肌酐(A)和蛋白尿百分比(B)直方圖Fig. 1 Histograms of mean creatinine level (A) and percentage of proteinuria (B) in recipients with AR and those without AR

表1 AR組和非AR組的人口學和臨床特征Tab. 1 Demographics and clinical characteristics of AR and non-AR group

表2 不同年齡組急性排斥反應發生率Tab. 2 Incidence of AR in different age groups (n,%)
5 AR危險因素的多因素分析 表1中與AR相關因素(P<0.1)被納入Cox比例風險模型。多因素分析顯示,供受者年齡分組是AR的獨立危險因素。年輕供者年輕受者組作為對照組,AR發生率最低(2.4%)。老年供者正常受者是AR的獨立危險因素,相對危險度為3.67(95% CI:2.61 ~ 4.58,P=0.002)。與老年供者年輕受者相比,正常供者年輕受者組和老年供者正常受者組的發生AR相對危險度分別為1.12(95% CI:0.64 ~ 2.01)和1.04(95% CI:0.87 ~1.23),差異無統計學意義。見表3。

表3 早期急性排斥反應發生危險的多因素分析Tab. 3 Multivariate analysis of risk factors of early AR episodes
討 論
臨床研究證實,腎移植術后排斥反應導致移植腎功能損害(血肌酐升高、蛋白尿)[7-8]。移植腎功能損害會導致移植腎持續的“自適應”過程,使腎小球處于高灌注、超濾過狀態,長久會導致腎間質和腎小球纖維化,引起節段性或腎小球全球硬化,最終導致移植物丟失[9]。老年供腎功能減退、適應能力差、缺血再灌注損失修復能力減弱、對藥物腎毒性耐受力差,減少急性排斥反應的發生率可明顯降低老年活體供腎移植失敗的風險,提高移植效果。
我們發現,老年供體腎移植AR風險在很大程度上取決于受者年齡。與年輕供者(<50歲)相比,老年供者(>50歲)并不增加移植后排斥風險,表明老年供腎(>50歲)不是急性排斥反應的危險因素。同樣,受者的年齡也不是AR的危險因素:年輕受者排斥反應的發生率并沒有增加。然而,供體和受體年齡的組合是腎移植后急性排斥反應的危險因素。本文發現,接受老年供腎的年輕受者是AR的高危人群。動物研究證明,老年器官移植可引起更強的早期免疫反應[10]。臨床研究證實,老年供體腎的免疫原性更強,可吸引更多的炎性細胞聚集[11-12]。綜上所述,老年供腎是高免疫風險的供體[13-15]。而年輕的受者對于異種抗原可產生一個更有效的免疫應答,因此是免疫高風險受者[16-17]。因此,AR在接受老年供腎的年輕受者中發生風險增加是不足為奇的。
本研究一個重要的臨床啟示是依據供受者年齡的個體化免疫抑制方案可以減少活體供腎移植AR的風險,提高移植效果。在臨床腎移植實踐中,接受老年供腎的年輕受者應被視作“免疫高風險”人群,并給予更強的免疫抑制方案。臨床經驗證實,腎移植術后誘導免疫抑制治療可降低急性排斥反應的風險[18]。因此對于接受老年供腎的年輕受者術后給予“高效免疫誘導方案+低CNI+足量抗增殖劑量”的免疫治療方案。這種個體化方案的優勢在于“高效免疫誘導方案+足量抗增殖劑量”明顯降低腎移植術后早期CNIs暴露水平且不增加急性排斥反應的風險,臨床上達到明顯減輕CNIs對老年供腎的腎毒性、降低排斥風險,提高移植腎效果[19-21]。而對于接受青年供腎的非年輕受者術后給予“較低免疫抑制強度的抑制方案”則有助于降低術后嚴重感染的風險[22]。因此,根據供受者年齡的個體化免疫抑制方案是提高活體供腎移植效果的關鍵[23]。
入選患者的數量相對較少是本研究的主要不足。然而,本研究最重要的特點是樣本間的均質性,且包含與排斥反應相關所有的變量。正因為如此,使本研究剔除了多種危險因素(如種族、不同免疫抑制方案、不同外科技術),導致結果發生偏倚。
總之,接受老年供腎的年輕腎移植受者是活體供腎移植急性排斥反應發生的獨立危險因素,供受者年齡的個體化免疫抑制方案可顯著降低排斥反應發生率,提高腎移植效果。在臨床活體腎移植中,需要更多的前瞻性臨床研究來驗證這種個體化免疫抑制方案的有效性和安全性。
1 Wolfe RA, Roys EC, Merion RM. Trends in organ donation and transplantation in the United States, 1999-2008[J]. Am J Transplant, 2010, 10(4 Pt 2): 961-972.
2 Weber DJ, Wang IW, Gracon AS, et al. Impact of donor age on survival after heart transplantation: an analysis of the United Network for Organ Sharing (UNOS) registry[J]. J Card Surg, 2014, 29(5):723-728.
3 Goh A. Graft survival trends in kidney transplants: an analysis of the UNOS database[J]. Clin Transpl, 2009: 41-54.
4 Tullius SG, Milford E. Kidney allocation and the aging immune response[J]. N Engl J Med, 2011, 364(14): 1369-1370.
5 Martins PN, Tullius SG, Markmann JF. Immunosenescence and immune response in organ transplantation[J]. Int Rev Immunol,2014, 33(3): 162-173.
6 Tullius SG, Tran H, Guleria I, et al. The combination of donor and recipient age is critical in determining host immunoresponsiveness and renal transplant outcome[J]. Ann Surg, 2010, 252(4):662-674.
7 Legendre C, Anglicheau D. Transplantation: proteinuria in kidney transplantation: an ongoing story[J]. Nat Rev Nephrol, 2013, 9(5):251-252.
8 Amer H, Lieske JC, Rule AD, et al. Urine high and low molecular weight proteins one-year post-kidney transplant: relationship to histology and graft survival[J]. Am J Transplant, 2013, 13(3):676-684.
9 Barai S, Gambhir S, Prasad N, et al. Levels of GFR and proteininduced hyperfiltration in kidney donors: a single-center experience in India[J]. Am J Kidney Dis, 2008, 51(3): 407-414.
10 Sidman CL, Luther EA, Marshall JD, et al. Increased expression of major histocompatibility complex antigens on lymphocytes from aged mice[J]. Proc Natl Acad Sci U S A, 1987, 84(21): 7624-7628.
11 Franceschi C, Capri M, Monti D, et al. Inflammaging and antiinflammaging: a systemic perspective on aging and longevity emerged from studies in humans[J]. Mech Ageing Dev, 2007, 128(1):92-105.
12 Agrawal A, Agrawal S, Cao JN, et al. Altered innate immune functioning of dendritic cells in elderly humans: a role of phosphoinositide 3-kinase-signaling pathway[J]. J Immunol,2007, 178(11): 6912-6922.
13 Denecke C, Ge X, Jurisch A, et al. Modified CD4(+) T-cell response in recipients of old cardiac allografts[J]. Transpl Int,2012, 25(3): 328-336.
14 Hricik DE, Poggio ED, Woodside KJ, et al. Effects of cellular sensitization and donor age on acute rejection and graft function after deceased-donor kidney transplantation[J]. Transplantation, 2013,95(10): 1254-1258.
15 Oetting WS, Guan W, Schladt DP, et al. Telomere length of recipients and living kidney donors and chronic graft dysfunction in kidney transplants[J]. Transplantation, 2013, 97(3): 325-329.
16 D?rje C, Midtvedt K, Holdaas H, et al. Early versus late acute antibody-mediated rejection in renal transplant recipients[J]. Transplantation, 2013, 96(1): 79-84.
17 Lebranchu Y, Baan C, Biancone L, et al. Pretransplant identification of acute rejection risk following kidney transplantation[J]. Transpl Int, 2014, 27(2): 129-138.
18 Khanmoradi K, Knorr JP, Feyssa EL, et al. Evaluating safety and efficacy of rabbit antithymocyte globulin induction in elderly kidney transplant recipients[J]. Exp Clin Transplant, 2013, 11(3):222-228.
19 Tsapepas DS, Mohan S, Tanriover B, et al. Impact of small variations in the delivered dose of rabbit antithymocyte induction therapy in kidney transplantation with early corticosteroid withdrawal[J]. Transplantation, 2012, 94(4): 325-330.
20 Br?cker V, Schubert V, Scheffner I, et al. Arteriolar lesions in renal transplant biopsies: prevalence, progression, and clinical significance[J]. Am J Pathol, 2012, 180(5): 1852-1862.
21 Snanoudj R, Royal V, Elie C, et al. Specificity of histological markers of long-term CNI nephrotoxicity in kidney-transplant recipients under low-dose cyclosporine therapy[J]. Am J Transplant, 2011, 11(12):2635-2646.
22 Andrés A, Budde K, Clavien PA, et al. A randomized trial comparing renal function in older kidney transplant patients following delayed versus immediate tacrolimus administration[J]. Transplantation, 2009, 88(9): 1101-1108.
23 Heinbokel T, Elkhal A, Liu G, et al. Immunosenescence and organ transplantation[J]. Transplant Rev (Orlando), 2013, 27(3):65-75.
Relationship between acute rejection in living donor kidney transplantation and age of donors and recipients
WANG Zhen, QIAN Yeyong, LI Kun, BAI Hongwei, LI Gang, FAN Yu, LIU Lupeng, CHANG Jingyuan, SHI Bingyi
No.2 Department of Urology, Institute of Organ Transplantation of PLA, 309th Hospital of PLA, Beijing 100091, China
SHI Bingyi. Email: shibingyi@medmail.com.cn
ObjectiveTo investigate the effects of age on acute rejection (AR) in living donor kidney transplantation (LDKT) recipients.MethodsThis study was performed in 327 donor–recipient pairs of kidney transplantation in our center from January 2006 to December 2013. Donors with age over than 55 years were defined as elder donors, while recipients with age younger than 30 years were defined as young recipients. Clinical baseline data about donors and recipients were recorded and patients were followed up at 1, 3, 6, 12, 24, 36, 48, 60 months after transplantation with medical examination, medical history examination, laboratory examination, AR occurrence examination. The risk factors that might be associated with AR were analyzed using both univariate analysis and Cox proportional hazards regression modeling.ResultsThe follow-up period of AR and without AR group was (35.9±13.2) months and (36.3±15.4) months, respectively. The incidence of AR in recipients within 3 months after transplantation was 7.3% (24/327). The serum creatinine level and the incidence of proteinuria in AR group were higher than without AR group in the same period. Multivariate analysis revealed that young recipient who received older donor graft was an independent risk factor for AR with the relative risk (RR) of 3.67 (95% CI: 2.61- 4.58, P=0.002).ConclusionThe independent risk factor of AR is young recipients who receive older donor graft.
aged (55 years); immunogenicity; acute rejection; kidney transplantation; living donor
R 617
A
2095-5227(2015)10-1025-04 DOI:10.3969/j.issn.2095-5227.2015.10.017
時間:2015-06-15 15:47
http://www.cnki.net/kcms/detail/11.3275.R.20150615.1547.003.html
2015-04-30
王振,男,博士,主治醫師。研究方向:泌尿外科和腎移植。Email: urology_wangzhen@163.com
石炳毅,男,主任醫師,博士生導師。Email: shibingyi @medmail.com.cn