Colorectal adenocarcinoma patients with M1a diseases gain more clinical benefits from palliative primary tumor resection than those with M1b diseases:A propensity score matching analysis
Cheng-Lin Li, De-Rong Tang, Jian Ji, Bao Zang, Chen Chen, Jian-Qiang Zhao
Cheng-Lin Li, De-Rong Tang, Jian Ji, Bao Zang, Chen Chen, Jian-Qiang Zhao, Department of Thoracic Surgery, The Affiliated Huaian No.1 People’s Hospital of Nanjing Medical University, Huaian 223300, Jiangsu Province, China
Abstract
Key words:Colorectal adenocarcinoma;Palliative primary tumor resection;Distant metastasis;Propensity score matching;Surveillance Epidemiology and End Results;Overall survival
INTRODUCTION
Colorectal cancer (CRC) is one of the three most common malignancies with 135430 individuals expected to be diagnosed in 2017 in the United States[1].However,approximately 20% of new CRC patients are diagnosed with distant-stage tumors,resulting in poor long-term outcomes with a 5-year survival rate of 23.2%[2].
Surgical resection is regarded as the only potentially curative treatment option for this disease and could significantly improve the prognosis of patients with metastatic CRC[3].Reeset al[4]reported that the 5-year cancer-specific survival (CSS) rate for metastatic CRC patients undergoing primary and hepatic resection was 36%.Abdallaet al[5]showed that patients receiving surgical resection of primary tumors and liver metastases had a 5-year survival rate of up to 58%.Similarly, curative surgical treatment could increase the 5-year survival rate of 32% to 68% in CRC patients with resectable lung metastasis[6,7].Unfortunately, only one-fifth to one-quarter of metastatic CRC patients can receive curative surgical treatment[8], indicating that metastatic CRC patients are a heterogenous population.
According to the 8thedition of American Joint Committee on Cancer (AJCC) tumornode-metastasis staging system, metastatic CRC are classified into M1a (metastasis confined to one organ or site) and M1b (metastases in more than one organ/site or the peritoneum).Complete resection is impossible for most metastatic CRC patients(especially for those with M1b diseases) even after neoadjuvant chemoradiation.The National Comprehensive Cancer Network clinical practice guidelines[9]do not recommend palliative surgery unless there is a risk of significant acute bleeding,obstruction,perforation,or other severe symptoms based on comprehensive analysis of the literature[10-12].However, accumulating evidence has shown that palliative surgery is associated with more favorable outcomes.For example, a pooled analysis including four randomized trials reported that patients receiving palliative primary tumor removal had prolonged overall survival (OS) compared with those not receiving operation[13].Another population-based retrospective study reviewing 37793 metastatic CRC patients showed that palliative surgery was significantly related to better OS and CSS[14].Finally, a systematic review consisting of 21 studies indicated that there was a survival benefit for palliative surgery in patients with metastatic CRC and criteria for palliative surgery should be extended on the basis of World Health Organization (WHO) performance status (PS) or tumor burden[15].
However, to our best knowledge, no studies have classified stage IV into subsets to assess the role of palliative surgery.Adenocarcinoma is the most common pathological type of CRC, accounting for approximately 90% of cases[16].Thus, we subdivided colorectal adenocarcinoma (CRA) patient populations with stage IV disease on the basis of comorbidities from the Surveillance, Epidemiology, and End Results (SEER)database into stage IVA (M1a diseases) and stage IVB (M1b diseases).Outcomes of palliative surgery were then independently assessed.
選擇我院畢業生的業務信函作為案例不僅接近了學生與跨境電商英語的心理距離,適宜性也非常強。比如,往屆學生寫作上出現的種種問題往往也是在讀生會蹈的覆轍。通過評析往屆學生信函上的錯誤與不足之處,在讀生的寫作水平能得到切實提高。
MATERIALS AND METHODS
Patient source
Patient data, originating between 2010 and 2015, was collected from the SEER database, one of the largest cancer databases in the world[14].The selection criteria were as follows:(1) Patients 18 years old or older;(2) Disease histologically diagnosed as adenocarcinoma;(3) Treated for first primary tumor;(4) Definite M1a or M1b diseases according to the 8thedition of AJCC staging system;(5) No surgery for metastatic sites(including distant lymph nodes);(6) Surgical procedure or no surgical procedure to primary tumor (excluding tumor destruction or no pathologic specimen or unknown whether there was a pathologic specimen);and (7) Active follow-up.Cases with unknown survival time, status, or those coded as 0 mo were excluded.The entire cohort was divided into two groups based on the median age and calculation result of X-tile program (Yale University, 3.6.1, Supplementary Figure 1).After propensity score matching (PSM), 2935 patients with M1a diseases and 2145 patients with M1b diseases were excluded owing to a lack of counterpart propensity scores.In survival analysis for M1a (liver metastasis) and M1a (lung metastasis), 2202 and 267 patients were further excluded, respectively.Follow-up time ranged from 1 to 71 mo.
Statistical analyses
Baseline characteristics of metastatic CRA patients, including sex, year of diagnosis,age, marital status, primary site, surgical information, race, grade, chemotherapy, and radiotherapy, were recorded and analyzed byχ2test.The patient prognosis was assessed using univariate and multivariate Cox regression analyses with hazard ratios and 95% confidence intervals.To minimize potential selection bias, 1:1 PSM without replacement was used to investigate the effect of palliative primary tumor resection on metastatic CRA.After PSM adjustment, Kaplan-Meier method was employed to analyze the OS for M1a and M1b patients.All statistical analyses were conducted using IBM SPSS Statistics 22.0.Pvalues <0.05 were considered statistically significant.
RESULTS
Baseline characteristics
A total of 19680 patients with metastatic CRA were collected from the SEER database,which included 10399 cases of M1a diseases and 9281 cases of M1b diseases (Table 1).The entire cohort consisted of 11107 (56.4%) males and 8573 (43.6%) females with a median age of 63 years (ranging from 18 to 108).Most patients were of White ethnicity(74.8%) and more than half of them had well or moderately differentiated tumors(grade I + II).Next, 15476 (78.6%) cases of primary tumors were located in the colon and 4204 (21.4%) in the rectum.The prevalence of metastatic CRA between 2010 and 2012 was similar to that between 2013 and 2015.However, M1b diseases seemed to account for a larger proportion from 48.4% during 2010-2012 to 51.6% during 2013-2015 while M1a diseases showed the opposite prevalence trend.
Of the entire cohort, 14057 (71.4%) metastatic CRA patients received chemotherapy and 975 (5.0%) received radiotherapy;9360 (47.6%) metastatic CRA patients received palliative primary tumor resection while 10320 (52.4%) did not.The proportion of patients with M1a diseases undergoing surgical procedure was much higher than that of M1b diseases (55.6% for M1a and 38.5% for M1b).

Table 1 Baseline characteristics of metastatic colorectal adenocarcinoma patients
Survival analysis
Univariate and multivariate Cox regression analyses for OS for both M1a and M1b patients were performed (Table 2).The common independent prognostic factors in both M1a and M1b patients included year of diagnosis (2010-2012vs2013-2015), age (<65vs≥ 65), race (whitevsblack), marital status (marriedvsothers), primary site (colonvsrectum), grade (I + IIvsIII + IV), surgery (yesvsno), and chemotherapy (yesvsno/unknown).Radiotherapy (yesvsno) was an independent prognostic factor for M1a patients but not for M1b patients.
After PSM adjustment, we obtained 3732 and 3568 matched patients in the M1a and M1b groups, respectively.Their survival curves were plotted by the Kaplan-Meier method (Figure 1A and D).Patients receiving palliative primary tumor resection had longer survival time than those without surgery (P<0.001).For patients with M1a diseases, palliative resection could increase the median survival time by 9 mo;for patients with M1b diseases, palliative resection can prolong the median survival time by 7 mo (Table 3).Then M1a diseases were further subdivided by metastatic site.Patients with liver metastasis and lung metastasis were included in the further analysis, whereas patients with bone metastasis and brain metastasis were excluded because of small sample size.As shown in Figure 1B and C, patients with lung metastasis could obtain more clinical benefit from palliative resection than those with liver metastasis (15 mo for lung metastasisvs8 mo for liver metastasis, Table 3,P<0.001).
DISCUSSION
Metastatic CRC is a lethal disease with a poor prognosis.While patients with metastatic CRC can obtain clinical benefits from curative surgery, there is still controversy with respect to the role of palliative primary tumor resection.To the best of our knowledge, this is the first population-based study subdividing stage IV into stages IVA (M1a diseases) and IVB (M1b diseases) to evaluate the effect of palliative primary tumor resection.It was determined that patients with M1a diseases could obtain more survival benefits than those with M1b diseases and patients with M1a(lung metastasis) got best long-term outcomes with median OS prolonged by 15 mo compared with those without surgical treatment.These findings provided further evidence to support palliative surgical procedure to metastatic CRA and develop effective individualized treatment strategy.
There were many predictors of OS in patients with unresectable metastatic CRC,including WHO PS, carcinoembryonic antigen level, number of metastatic sites, and palliative surgery[13].Liet al[17]showed that tumor location (right colonvsleft colonvsrectum) was also an independent prognostic factor for metastatic CRC.The results were in line with our findings that patients with rectal cancer were at a lower risk of death than those with colon cancer, possibly owing to higher proportion of lung metastasis in patients with rectal cancer[18].However, no studies focus on the effect of palliative surgery according to the number of metastatic sites or organs (M1a or M1b).Tarantinoet al[14]reported that the survival difference between patients with palliative resection and those without palliative resection was anticipated to decrease due to the development of chemotherapeutic and molecule-targeted drugs.Actually, the significance of survival difference has persisted over time.This may be explained by the heterogeneity of stage IVA (M1a diseases) and stage IVB (M1b diseases).The development of systemic treatment could decrease the survival difference and increase surgery conversion indeed.The proportion of M1b diseases grew from 48.6% during 2010-2012 to 51.6% during 2013-2015 (Table 1,P<0.001) and such patients were less likely to undergo surgical treatment than those with M1a diseases.This may also explain the decreased rate of patients undergoing primary tumor removal observed during 1998-2009 in Tarantino’s study[14].
Liver and lung metastases are the most two common distant metastases from CRC[7], accounting for 50% and 10%-15% of CRC, respectively[19,20].The prognosis of patients with liver or lung metastasis is usually better than those with brain or bone metastasis[21].According to the published literature, median OS was 3-6 mo for patients with brain metastases and 5-7 mo for those with bone metastases[22-28].For patients with unresectable liver metastases who were treated with chemotherapy only, median OS was approximately 20 mo[29].By comparison, patients with unresectable lung metastases, who achieved a complete or partial response to chemotherapy, could achieve a median OS of 27 mo[30].From the perspective of epidemiology, the median time between the diagnosis of CRC and the emergence of liver metastases was shorterthan that for lung metastases (17.2 mo for livervs24.6 mo for lung)[31], which indicated that liver metastases possessed more aggressive malignant behavior to some extent.These survival findings were similar to the present results (22 mo for liver metastasis with palliative surgeryvs33 mo for lung metastasis with palliative surgery).

Table 2 Univariate and multivariate cox regression analyses for overall survival of metastatic colorectal adenocarcinoma patients
There are several limitations to this study that should be noted.PSM can adjust potential confounding variables and decrease selection bias as much as possible,increasing precision by creating a ‘quasi-randomized’ experiment[32].However, wewould like to acknowledge the limitations of our study.First, some significant factors such as surgical complications, life quality, operative tolerance, and laboratory parameters were not included.Second, detailed number of metastases in a single organ was not provided in the SEER database, which hampered further analysis for M1a diseases.Third, further classifications for M1 category in the AJCC staging system were not recorded before 2010, and only patient data between 2010 and 2015 were collected.The conclusions should be validated by more prospective data in the future.

Table 3 Survival time for metastatic colorectal adenocarcinoma patients with or without palliative primary tumor resection
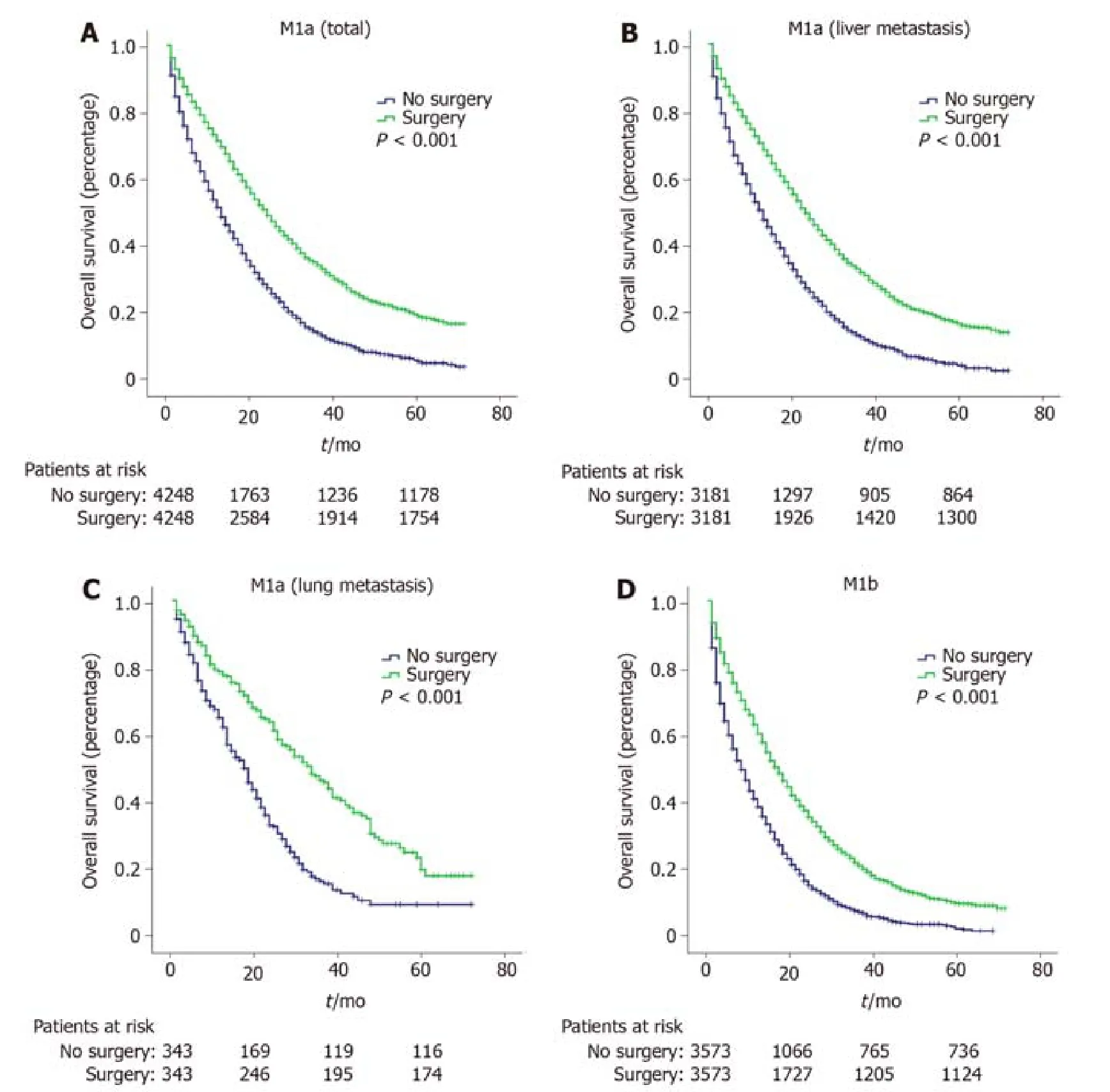
Figure 1 Survival time for metastatic colorectal adenocarcinoma patients with or without palliative primary tumor resection.
ARTICLE HIGHLIGHTS
Research background
The National Comprehensive Cancer Network clinical practice guidelines do not recommend palliative surgery for metastatic colorectal adenocarcinoma (CRA) unless there is a risk of significant acute bleeding, obstruction, perforation, or another severe symptom.
Research motivation
Accumulating evidence has demonstrated that palliative surgery for metastatic CRA patients was associated with more favorable outcomes.However, no studies further classified CRA patients with stage IV into subsets to assess the role of palliative surgery.
Research objectives
The purpose of this study was to investigate the separate role of palliative primary tumor resection for CRA patients with stage IVA (M1a diseases) and stage IVB (M1b diseases).
Research methods
CRA patient records with definite M1a and M1b categories were analyzed by adjusted propensity score matching.Patient prognosis was assessed by univariate and multivariate Cox regression analyses with hazard ratios and 95% confidence intervals.
Research results
Patients with metastatic CRA receiving palliative primary tumor resection had a longer survival time than those who did not (P<0.001).Palliative resection increased the median survival time by 9 mo and by 7 mo for patients with M1a and M1b diseases, respectively.For M1a diseases, patients with lung metastasis had more survival benefit from palliative resection than those with liver metastasis (15 mo for lung metastasisvs8 mo for liver metastasis,P<0.001).
Research conclusions
Palliative primary tumor resection improves survival for all CRA patients but more beneficial for those with M1a diseases than those with M1b diseases.Specifically,patients with M1a (lung metastasis) had the best long-term outcomes after palliative primary tumor resection.
Research perspectives
These findings provided further evidence to support the use of palliative surgical procedures to treat metastatic CRA and develop effective individualized treatment strategies.
 World Journal of Clinical Cases2020年15期
World Journal of Clinical Cases2020年15期
- World Journal of Clinical Cases的其它文章
- Facial and bilateral lower extremity edema due to drug-drug interactions in a patient with hepatitis C virus infection and benign prostate hypertrophy:A case report
- Total laparoscopic segmental gastrectomy for gastrointestinal stromal tumors:A case report
- COVID-19 with asthma:A case report
- Computed tomography, magnetic resonance imaging, and Fdeoxyglucose positron emission computed tomography/computed tomography findings of alveolar soft part sarcoma with calcification in the thigh:A case report
- Acute suppurative oesophagitis with fever and cough:A case report
- Coexistence of ovarian serous papillary cystadenofibroma and type A insulin resistance syndrome in a 14-year-old girl:A case report
