Changes in pulsatile ocular blood flow in normal tension glaucoma patients
Tarannum Shakeel
?
Changes in pulsatile ocular blood flow in normal tension glaucoma patients
Tarannum Shakeel
Department of Ophthalmology, SGRRIM&HS, Patel Nagar, Dehradun 248001, India
方法:前瞻性病例對照研究。彩色多普勒超聲成像(CDI)用于測量正常眼壓性青光眼患者的眼部血流參數-收縮期峰值流速(Vmax),舒張末期血流速度(Vd),最大速度的時間平均值(TAmax),搏動指數(PI),眼動脈(OA)阻力指數(RI)與收縮期/舒張期比值(S/D),視網膜中央動脈(CRA)和睫狀后短動脈(SPCA),并對比正常人數值。比較兩組采用非配對t檢驗,P≤0.05時有顯著意義。
結果:當與正常人組P值分別為0.605,0.254,0.348對比時,正常眼壓性青光眼組中眼動脈,視網膜中央動脈和睫狀后短動脈的收縮期峰值流速降低。當與正常人組P值分別為0.000,0.014,0.138對比時,正常眼壓性青光眼組中三項的舒張末期血流速度降低。當眼動脈P值分別為0.000,0.045,視網膜中央動脈P值為0.000和0.006,睫狀后短動脈P值0.024和0.024時,搏動指數和阻力指數增加。當正常人組眼動脈,視網膜中央動脈和睫狀后短動脈P值分別為0.047,0.041和0.189時,正常眼壓性青光眼組收縮期/舒張期比值增加。
結論:研究得出彩色多普勒超聲成像是測量青光眼血管組成部分的有效途徑。比較正常眼壓性青光眼組和正常人組時發現眼部血管血流速度下降,血管阻力指數增加。
?AIM: To evaluate changes in pulsatile ocular blood flow in normal tension glaucoma (NTG) patients.
?METHODS: In this prospective case control study color Doppler imaging (CDI) was used to determine ocular blood flow parameters - peak systolic velocity(Vmax), end diastolic velocity (Vd), time average mean of maximum velocity (TAmax), pulsatility index (PI), resistive index (RI) and systolic/diastolic ratio (S/D) in ophthalmic artery (OA), central retinal artery (CRA) and short posterior ciliary artery (SPCA) in NTG patients and a comparision was made with the normal subjects. Unpaired Student’s t-test was used to compare the two groups andP≤0.05 was considered significant.
?RESULTS: Vmaxin OA, CRA and SPCA in the NTG group was decreased when compared to normals withPvalues 0.605, 0.254 and 0.348 respectively. Vdin the NTG group was also decreased in all the three vessels when compared to the normal subjects withPvalues 0.000, 0.014 and 0.138 in OA, CRA, and SPCA respectively. The PI and RI were increased in all the vessels in the NTG group withPvalues 0.000 and 0.045 for the OA, 0.000 and 0.006 for the CRA and 0.002 and 0.024 for the SPCA. S/D ratio was increased in the NTG group as compared to normals withPvalues 0.047, 0.041 and 0.189 in OA, CRA and SPCA respectively.
?CONCLUSION: This study concludes that CDI may provide an effective way of measuring part of the vascular component of glaucoma. We found decreased blood flow velocity and increased resistive indices in the ocular vasculature in the NTG group as compared to normal subjects.
Color Doppler imaging; normal tension glaucoma; ophthalmic artery; central retinal artery; short posterior ciliary artery; peak systolic velocity; end diastolic velocity; pulsatility index; resistive index
INTRODUCTION
Despite its high prevalence, glaucoma remains a disease of unknown etiology and inadequate treatment. Although elevated intraocular pressure (IOP) is the primary risk factor, the very existence of normal tension glaucoma (NTG) indicate that other factors might also be involved in the pathogenesis of glaucoma. A vascular theory of glaucoma has long been considered[1-2].Many vascular related diseases have been reported to be associated with normal tension glaucoma including diabetes[3],hypertension[4],migraine[5]and peripheral vasospasm[6], suggesting that circulatory disturbances may be an associated factor.
Color Doppler imaging (CDI) allows non-invasive assessment of retrobulbar circulation.It is an established method for investigation of ocular and orbital blood flow characterstics and its results are relatively reproducible[7]. Recent studies performed with CDI have shown altered retrobulbar haemodynamics in glaucoma patients[8-9].
In the present study we have used CDI with spectral analysis for measuringpeak systolic velocity (Vmax), end diastolic velocity (Vd), pulsatility index (PI), resistive index (RI) and systolic/diastolic (S/D) ratio in ophthalmic artery (OA), central retinal artery (CRA) and short posterior ciliary artery (SPCA) in NTG patients. These indices have been compared with those of normal subjects.
榆陽煤礦摒棄傳統垮落法開采形式,在2307工作面首次采用高流動性風積砂似膏體充填材料,成功地進行了風積砂似膏體充填采煤的工業化試驗,為西北地區保水開采技術提供參考和借鑒[1~3]。
SUBJECTS AND METHODS
In a prospective, noninterventional, case-control single centre study, we enrolled 42 NTG patients (84 eyes) and 36 normal subjects (72 eyes). An ethical clearance was taken from the institutional review board. A written and informed consent was taken from all participants and they were made aware of the scientific nature of the study. None of the participants recieved stipend for the participation nor were they charged for the investigations done. Inclusion criteria for normal subjects was best corrected Snellen visual acuity of 20/20, normal anterior segment on slit lamp biomicroscopy, normal fundus on indirect ophthalmoscopy, intraocular pressure (IOP) <20 mm Hg and normal visual fields. Any volunteer with hazy media, relatives of glaucoma patients, those with any fundus pathology, systemic disease or on systemic drugs were excluded from the study. Inclusion criteria for NTG patients was IOP <20 mm Hg(Goldmann applanation tonometer) as confirmed on diurnal inpatient phasing, characterstic optic disc changes, characteristic visual field loss ( Humphrey automated perimetry) and open angles on gonioscopy (Goldmann three mirror gonioscope). History of diabetes mellitus, systemic hypertension, hypotension and shock, myocardial infarction, myopia, retinal vein occlusion, migraine and dyspnoea was also taken.
After detailed history and clinical examination,the subjects were taken for CDI. CDI allows non-invasive examination of blood flow velocity in OA, CRA and SPCA, by providing simultaneous Doppler and B- Scan ultrasound images on a monitor.
A logic 500 Pro-series (GE company) machine with 5-9 MHZ linear multifrequency probe was used for B mode and Color Doppler imaging . All the CDI examinations were performed by a single experienced sonographer, who was unaware of the patient’s clinical status. The color Doppler images were analyzed separately by the radiologist and the ophthalmologist.
Table 1Age distribution of normal subjects and NTG patients

GroupNo.ofpatientsMeanage±SD(a)Agerange(a)PNormals3639.16±18.4213-75NTG4250.8±18.3118-800.209
NTG: Normal tension glaucoma.
Table 2Gender distribution of normal subjects and NTG patients

GroupM(%)F(%)PNormals23(63.88%)13(36.12%)NTG21(50%)21(50%)0.613
NTG: Normal tension glaucoma.
Following measurements were made in OA, CRA and SPCA. PI was calculated by Gosing’s formula (Vmax-Vd/TAmax). RI was calculated by Pourcelot’s formula (Vmax-Vd/Vmax). The Shapiro -Wilks Test was used to determine whether the ocular blood flow values among normal subjects confirms to a normal distribution. The unpaired student’s t- test was used to compare whether the differences between the normal and glaucoma subjects were statistically significant. Significance was set atP≤0.05. Simple linear regression analysis was used to examine the association between CDI measurements and age.
RESULTS
We chose 42 NTG patients and 36 normal subjects. The mean age of normal subjects was 39.16± 18.42y and mean age of NTG patients was 50.80±18.31y. The difference in age was not statistically significant (P= 0.209)(Table 1).
The gender distribution varied widely in the two groups. However the difference was not statistically significant (Table 2).
None of the control subjects had any significant cardiovascular, respiratory or neurological history. In the NTG group 3 patients (7.14%) were controlled diabetics and 3 patients (7.14%) gave history of attacks of migraine
The comparision of blood flow parameters of the NTG group and normal subjects is shown in Table 3.
Table 3Blood flow parameters in normal subjects and NTG patients
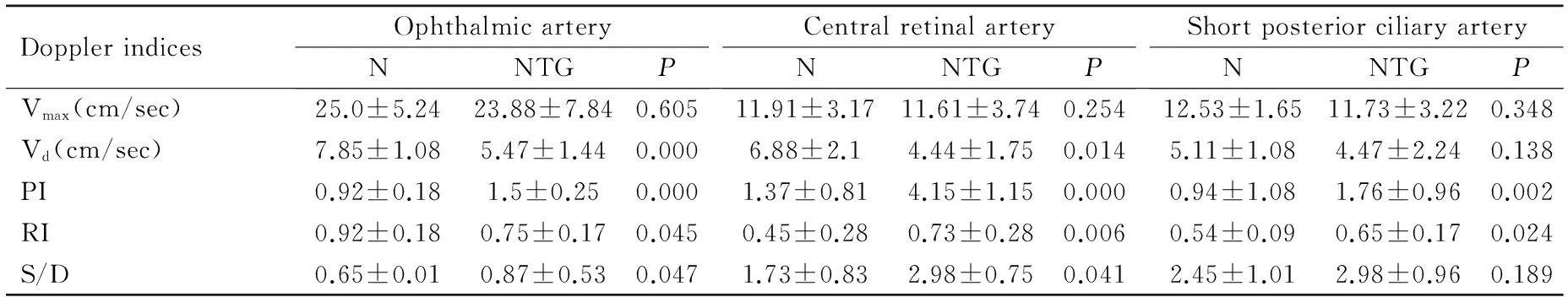
DopplerindicesOphthalmicarteryNNTGPCentralretinalarteryNNTGPShortposteriorciliaryarteryNNTGPVmax(cm/sec)25.0±5.2423.88±7.840.60511.91±3.1711.61±3.740.25412.53±1.6511.73±3.220.348Vd(cm/sec)7.85±1.085.47±1.440.0006.88±2.14.44±1.750.0145.11±1.084.47±2.240.138PI0.92±0.181.5±0.250.0001.37±0.814.15±1.150.0000.94±1.081.76±0.960.002RI0.92±0.180.75±0.170.0450.45±0.280.73±0.280.0060.54±0.090.65±0.170.024S/D0.65±0.010.87±0.530.0471.73±0.832.98±0.750.0412.45±1.012.98±0.960.189
Vmax: Peak systolic velocity; Vd: End diastolic velocity; PI: Pulsatility index; RI: Resistive index; S/D: Systolic/diastolic; NTG: Normal tension glaucoma.
DISCUSSION
The exact pathogenesis of glaucoma remains unknown. Two main theories of glaucomatous damage have been considered. A) mechanical theory; B) vascular theory. According to the mechanical theory, increased IOP causes stretching of the laminar beams and damage to the retinal ganglion cell axons. The vascular theory considers glaucomatous optic neuropathy as a consequence of insufficient blood supply due to either increased IOP or other risk factors reducing ocular blood flow[10].
The notion that glaucoma could have a vascular basis derives from certain circumstantial lines of evidence. The existence of NTG implies that mechanical theories of pressure induced axonal transport defects are incomplete. The association of NTG with other vasospastic diseases such as migraine again indicates that the cause may be of primary vascular nature[11]. It has also been shown that patients with glaucoma have an abnormal increase in plasma endothelin-1 (ET-1) after the body cools. It is possible that at least in some patients, increased levels of ET-1 in response to vasospastic stimuli may be involved in the pathogenesis of glaucomatous damage[12].
With the use of Doppler ultrasound of the orbit, a non invasive examination of retrobulbar circulation is possible . Several studies using CDI have revealed altered orbital hemodynamics in patients with glaucoma[13-14]. In the NTG group as shown in Table 3, Vmaxwas not significantly altered in all the three vessels when compared to normal subjects. Vdwas significantly reduced in OA and CRA. PI and RI were significantly increased in all the three vessels when compared to normal subjects and S/D ratio was increased significantly in OA and CRA but not in SPCA. The results were not consistent in SPCA. This could be because of the technical difficulties for imaging this particular area of vasculature due to thinner caliber and more tortuous configuration of ciliary arteries. It is difficult to follow their course and accurately angle the ultrasound beam within these vessels. The resistive index being angle dependent, is considered the most reliable parameter in these vessels. Our results are comparative with the previous studies[15-17]. In our study since there was no difference in Vmax, so it appears that major contribution to the increased vascular resistance (RI), was reduced end diastolic velocity.
The interpretation of the changes in blood velocity and RI is difficult. The vascular bed of optic nerve head (ONH) consists almost entirely of capillaries. Capillaries are known to represent the point of highest vascular resistance within the circulation. This increased resistance is supported by our results in which Vd, PI and RI attained greater and more significant difference than Vmaxbetween the glaucoma and normal groups.
Measurement of retrobulbar hemodynamics can be affected by systemic factors such as age[18], blood pressure[4], and prevalence of systemic diseases like diabetes mellitus[3]and migraine[5]. Our study design took these important points into consideration.
Several studies support the idea that circulatory abnormalities represent risk factors for glaucoma[6]. Reduced blood flow in patients with glaucoma does not automatically indicate damage. It remains to be established whether such alterations are present primarily and thus pathogenically active, or whether they occur secondarily. The fact that ocular blood flow improves on carotid revascularization surgery[19]and the association of normal tension glaucoma with systemic vascular diseases[3-6]makes it unlikely that these alterations are only secondary to glaucomatous damage.
In Doppler ultrasonography, the interpretation of the measured parameters is difficult. CDI measures blood velocity and not blood flow, which is calculated by the product of blood velocity and cross sectional area of the vessel measured. Poiseulle’s law states that volume flow is proportional to the fourth power of the radius of the vessel. Currently it is impossible to determine accurately the diameter of orbital vessels in vivo with this technique. Despite this limitation, we believe that flow velocities, PI and RI may give us some clues to the status of ocular circulation and may be of diagnostic and therapeutic value in various groups of glaucoma.
From this study we conclude that CDI provides an effective way to measure blood velocities in the orbit. We found decreased blood velocity and increased resistive index in the ocular vasculature of NTG patients. These changes could be a cause or consequence of glaucomatous optic atrophy. CDI may provide a means of measuring part of the vascular component in glaucoma in greater detail. This study suggests that in the diagnosis of glaucoma, it is necessary to know not only the IOP, but also the ocular blood flow velocities. Further studies are required to know the cause of reduction of ocular blood flow in glaucoma as well as effect of treatment on ocular blood flow.
1 Yanagi M, Kawasaki R, Wang JJ, Wong TY, Crowston J, Kiuchi Y. Vascular risk factors in glaucoma: a review.ClinExperimentOphthalmol2011;39(3):252-258
2 Mroczkowska S, Benavente-Perez A, Negi A, Sung V, Patel SR, Gherghel D. Primary open-angle glaucoma vs normal-tension glaucoma: the vascular perspective.JAMAOphthalmol2013;131(1):36-43
3 Jeganathan VS, Wang JJ, Wong TY. Ocular associations of diabetes other than diabetic retinopathy.DiabetesCare2008;31(9):1905-1912
4 Zhao D, Cho J, Kim MH, Guallar E. The association of blood pressure and primary open-angle glaucoma: a meta-analysis.AmJOphthalmol2014;158(3): 615-627
5 Demircan S, AtaM, Ark Yüksel S, Ulusoy MD, YuvacI, Arifoglu HB, Bakan B, Zararsz G. The impact of migraine on posterior ocular structures.JOphthalmol2015;2015:1-8
6 Moore D, Harris A, Wudunn D, Kheradiya N, Siesky B. Dysfunctional regulation of ocular blood flow: A risk factor for glaucoma?ClinOphthalmol2008;2(4):849-861
7 Stalmans I, Siesky B, Zeyen T, Fieuws S, Harris A. Reproducibility of color Doppler imaging.GraefesArchClinExpOphthalmol2009;247(11):1531-1538
8 Meng N, Zhang P, Huang H, Ma J, Zhang Y, Li H, Qu Y. Color Doppler imaging analysis of retrobulbar blood flow velocities in primary open-angle glaucomatous eyes: a meta-analysis.PLoSOne2013;8(5):e62723
9 Garh?fer G, Fuchsj?ger-Mayrl G, Vass C, Pemp B, Hommer A, Schmetterer L. Retrobulbar blood flow velocities in open angle glaucoma and their association with mean arterial blood pressure.InvestOphthalmolVisSci2010;51(12):6652-6657
10 Cherecheanu AP, Garhofer G, Schmidl D, Werkmeister R, Schmetterer L. Ocular perfusion pressure and ocular blood flow in glaucoma.CurrOpinPharmacol2013;13(1):36-42
11 Douglas R A .Normal-tension glaucoma (Low-tension glaucoma).IndianJOphthalmol2011;59(Suppl 1):S97-S101
12 Henry E, Newby DE,Webb DJ, Hadoke PW, O’Brein CJ. Altered endothelin-1 vasoreactivity in patients with untreated normal-pressure glaucoma.InvestOphthalmolVisSci2006; 47(6):2528-2532
13 Jimenez-Aragon F, Garcia-Martin E, Larrosa-Lopez R, Artigas-Martín JM, Seral-Moral P, Pablo LE. Role of color Doppler imaging in early diagnosis and prediction of progression in glaucoma.BiomedResInt 2013;2013:871689
14 Sharma NC, Bangiya D. Comparative study of ocular blood flow parameters by color Doppler imaging in healthy and glaucomatous eye.IndianJRadiolImaging2006;16:679-682
15 Kuerten D, Fuest M, Koch EC, Koutsonas A, Plange N.Retrobulbar Hemodynamics and Visual Field Progression in Normal Tension Glaucoma: A Long-Term Follow-Up Study.BiomedResInt2015;2015:158097
16 Galassi F, Giambene B, Varriale R.Systemic vascular dysregulation and retrobulbar hemodynamics in normal-tension glaucoma.InvestOphthalmolVisSci2011;52:4467-4471
17 Flammer J, Konieczka K, FlammerAJ. The role of ocular blood flow in the pathogenesis of glaucomatous damage.USOphthalmicReview2011;4(2):84-87
18 Boehm AG, Koeller AU, Pillunat LE. The effect of age on optic nerve head blood flow.InvestOphthalmolVisSci2005;46:1291-1295
19 Kawaguchi S, Iida J, Uchiyama Y. Ocular Circulation and Chronic Ocular Ischemic Syndrome before and after Carotid Artery Revascularization Surgery.JOphthalmol2012;2012:350475
正常眼壓性青光眼患者眼部血流的波動性變化
Tarannum Shakeel
248001印度德拉敦Patel Nagar SGRRIMHS眼科)
Tarannum Shakeel. 印度德拉敦Patel Nagar SGRRIMHS眼科. tarannumshakeel9@gmail.com
目的:評價正常眼壓性青光眼(NTG)患者眼部血流的波動性變化。……