下頜髁突矢狀骨折髓內髓外雙重內固定術的臨床應用
陳傳俊陳曉陽陳靜
1.皖南醫學院口腔醫學院,蕪湖 241002;2.安徽醫科大學第三附屬醫院口腔頜面外科,合肥 230061;3.安徽濟民腫瘤醫院口腔科,合肥 230011
·臨床研究·
下頜髁突矢狀骨折髓內髓外雙重內固定術的臨床應用
陳傳俊1陳曉陽2陳靜3
1.皖南醫學院口腔醫學院,蕪湖 241002;
2.安徽醫科大學第三附屬醫院口腔頜面外科,合肥 230061;
3.安徽濟民腫瘤醫院口腔科,合肥 230011
目的 探討髓內及髓外雙重內固定在下頜髁突矢狀骨折開放復位內固定中的應用價值。方法 采用髓內髓外雙重內固定術治療18例24側髁突矢狀骨折,固定方法:單一螺釘或克氏針行髓內固定,配合一塊鈦板行髓外固定,伴發他處骨折者同期行精確復位固定。術后通過拍攝CT和全景X線片評價鈦板固定情況、骨折段復位精準度及穩固性,通過臨床檢查評價咬合關系、開口度、開口型。結果 術后X線全景片或CT檢查顯示,24側髁突矢狀骨折段均未發現術后旋轉移位,對位良好;鈦板和螺釘無扭曲、折斷和松脫。術后咬合關系、開口度、開口型恢復良好。結論 髓內髓外雙重內固定具有抗骨折段旋轉作用,髓內螺釘和髓外鈦板在空間上互不干擾,是下頜骨髁突矢狀骨折固定的良好方法。
髁突矢狀骨折; 堅強內固定; 髓內固定; 髓外固定
頜面部外傷患者發生下頜髁突矢狀骨折(sagittal fracture of the mandibular condyle,SFMC)時,下頜髁突內側的骨折段常因翼外肌的牽拉而發生向前、內、下方的移位,早期多表現為髁突高度降低,后期常發生顳下頜關節強直,尤其是在伴發下頜骨前份骨折且沒有精準復位的狀態下更容易發生關節強直[1-4]。對于發生了骨折段移位的SFMC,除兒童以外,目前國內外在治療方案的選擇上逐漸趨于統一,即采用手術開放復位內固定進行治療;但是就移位骨折段的固定方法而言,則存在多種方法并存的局面:單個微型鈦板固定[5]、骨折段取出回植雙微型鈦板或單板固定[6-7]、單個長皮質釘固定等[8-9]。上述固定方法常因翼外肌的牽引作用而發生一些術后并發癥,如單個長皮質釘固定可發生骨折段旋轉,單個微型鈦板固定可發生鈦板扭曲甚至折斷,骨折段取出后再回植有導致骨吸收甚至骨壞死的可能。為解決現有固定方法存在的缺陷,本文使用髓內和髓外雙重內固定方法治療SFMC,取得了良好的效果,現報告如下。
1 材料和方法
1.1 患者資料
本組病例來自2002—2015年累積的18例SFMC患者(共24側),其中12例為單側SFMC,6例為雙側SFMC,伴發下頜骨他處骨折4例。男14例,女4例,年齡18~80歲。致傷原因:8例為轎車駕駛車禍傷,4例為摩托車駕駛事故傷,3例為騎自行車事故傷,2例為運動性損傷,1例為斗毆致傷。所有的患者均為單側或雙側SFMC伴骨折段移位,且經CT或全景X線片確診。受傷至手術時間為5~16 d,平均7.8 d。
1.2 外科復位方法
術前于上下牙槽突安放支抗釘實施頜間彈性牽引。全身麻醉下以耳屏前的拐杖型切口入路,分離達關節囊,T形切開髁突頸部的關節囊附著從而暴露髁突殘端,由于髁突殘端的阻擋使得術者的視野和器械難以抵達移向前下內方的骨折段,從而增加了骨折段復位的難度,故筆者使用提骨鉤勾住下頜乙狀切跡用力向足向牽拉,以加大關節間隙及周圍的操作空間(圖1),再輔以神經拉鉤或牙周膜剝離子等纖細的器械輕輕夾持或勾住移位的骨折段使之復位。固定分兩個步驟進行。1)髓內固定:平行于髁突橫軸,在骨折段復位的狀態下自髁突外極向內極方向鉆孔,穿經髁突殘端和骨折段,以等同于髁突內外極之間距離長度的皮質螺釘旋入或克氏針插入(圖2左)。2)髓外固定:用0.6 mm的四孔微型鈦板橫跨骨折線安放于皮質表面,與髓內固定螺釘或克氏針呈十字交叉(不平行)并固定(圖2右)。最后將移位或撕裂的關節盤復位縫合,分層關閉創口。伴發下頜他處骨折者同期行精確復位固定。次日實施頜間牽引并持續2周,囑患者進軟食2周。術后隨訪,隨訪時間為10~25個月,平均為16個月。
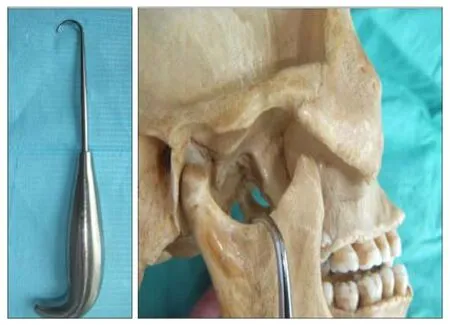
圖 1 使用提骨鉤(左)足向牽拉以擴大關節間隙和手術野(右)Fig 1 A lift bone hook used (left) to grapple the sigmoid notch with caudal traction to widen the joint space (right)
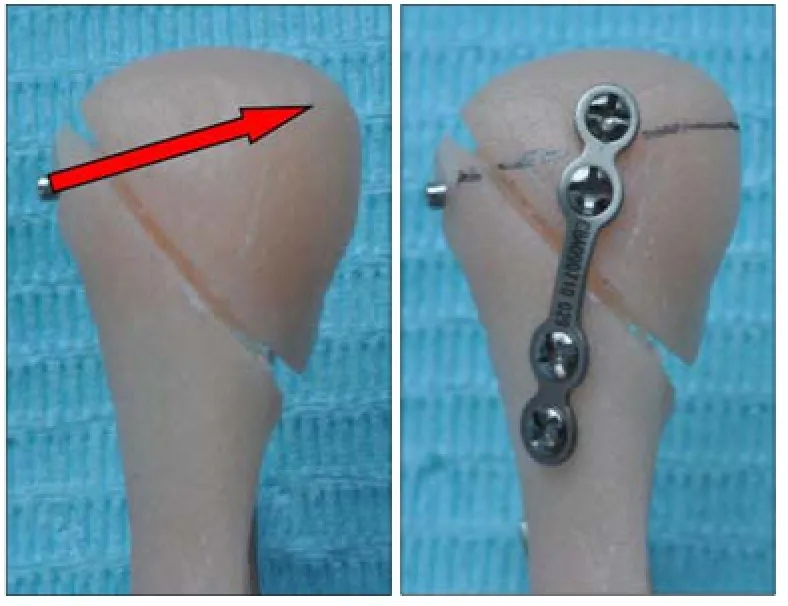
圖 2 髓內髓外雙重內固定Fig 2 Extramedullary fixation combined with intramedullary fixa- tion
1.3 效果評價
術后拍攝CT和全景X線片來評價鈦板固定情況、骨折段復位精準度及穩固性,通過臨床檢查評價患者咬合關系的恢復情況,并檢查患者的開口度和開口型。
2 結果
在24側SFMC中,有2例患者出現暫時性面神經損傷,主要表現為額皺變淺,半年后均恢復正常;其余無術中和術后并發癥。術后X線全景片或CT檢查顯示:骨折段對位良好,無旋轉移位情況發生,髁突形態正常(圖3);無鈦板及螺釘松脫、扭曲或折斷。術后咬合關系恢復良好,開口度及開口型恢復正常。
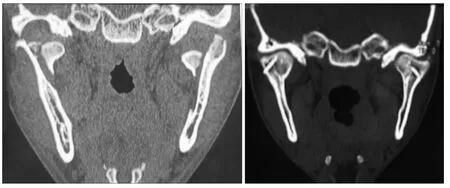
圖 3 1例患者的術前(左)及術后(右)CTFig 3 Preoperative (left) and postoperative (right) CT scan of a patient
3 討論
有關SFMC的內固定方式方法有諸多報道。有學者[5-6]將前內下移位的內側骨折段解剖分離并剝離翼外肌附著后取出,在體外鉆孔并安放內固定鈦合金板,然后將骨折段連同鈦合金板復位回植固定。這種外科處理方法有值得商榷的地方,因為骨折段一旦失去肌肉附著,血液循環即被中斷,骨折段有發生吸收甚至壞死的可能性[7-8]。有學者[8-9]曾推薦利用單一長螺釘固定SFMC骨折段,但筆者在使用單一長螺釘固定這一方法時曾遇見意外情況,即骨折段固定術后在翼外肌的強力牽引下發生旋轉移位,長螺釘猶如穿插于冰糖葫蘆的中軸,成了骨折段移位的旋轉軸。Meng等[10]和Xin等[11]提出可以使用兩個長螺釘固定,以避免骨折段旋轉。也有學者[6]使用兩個微型鈦板固定SFMC骨折段,也是為了避免骨折段的旋轉移位。這些方法較好地解決了骨折段旋轉移位的問題,但從解剖上看,顳下頜關節是小關節,髁突本身是較小的指狀突起,發生SFMC時,有時骨折線靠近髁突內極,其內側移位的骨折段則是一微小的骨塊,當使用兩個螺釘髓內固定或是使用兩個鈦板髓外固定時,一方面微小的骨折段安放鈦板或螺釘常顯得空間不足,另一方面反復多個鉆孔有導致骨折段破碎的可能。筆者也曾使用兩個長螺釘固定SFMC骨折段,在操作過程中常發生骨折段破碎的現象。綜上所述,SFMC現有的固定方式均存在一定的缺陷,本文所采用的髓內和髓外雙重內固定有以下優點。1)抗旋轉作用。髓內髓外聯合雙重固定,特別是固定裝置的十字交叉安放,具有抗旋轉作用,避免了單一長螺釘髓內固定出現術后骨折段旋轉移位的可能性。2)固定件分配空間合理,髓內髓外雙重固定合理地分配了固定件占用的空間,互不干擾,特別適合那些內側移位的小骨折段固定。
SFMC內固定方式目前尚不統一,其治療方案的選擇也是從爭議走向趨同的過程。由于SFMC容易導致顳下頜關節強直,故其治療方案的選擇備受關注[4,9,12-15]。近年來的公開資料越來越多地傾向于對成人SFMC選擇外科開放復位內固定,兒童的SFMC選擇保守治療方案[16-18]。He等[13-14]通過回顧性調查分析發現,SFMC伴發下頜他處骨折可因下頜弓外展而擴大,髁突外極或髁突的殘端向外上移位而抵觸顴弓發生粘連,形成關節強直。Duan等[4]通過分析CT及MRI資料顯示,關節盤的受損或移位與SFMC的創傷性關節強直高度相關,這是因為骨折段或髁突外極殘端與顳骨關節面間失去正常阻隔結構而直接相抵,從而誘發關節強直。Meng等[19]于2009年提出翼外肌牽張成骨假說,解釋翼外肌在創傷性顳下頜關節強直發生中的作用。該假說認為,翼外肌的動力牽拉使得骨折段和髁突殘端間的間隙漸進性成骨,大量的成骨和周邊結構的融合導致關節強直,其骨生成機制和牽張成骨類似。這一假說已被動物模型所證實[20-21]。綜上所述,伴隨著對創傷性顳下頜關節強直發生機制的理解深化,SFMC治療方案的選擇也在發生變化,外科精準復位內固定術逐漸成為被廣泛認同的方案。
[1] Long X, Li X, Cheng Y, et al. Preservation of disc for treatment of traumatic temporomandibular joint ankylosis[J]. J Oral Maxillofac Surg, 2005, 63(7):897-902.
[2] 王霄, 張益, 李江明. 髁突矢狀骨折繼發顳下頜關節強直動物模型的建立[J]. 北京大學學報(醫學版), 2011, 43(6): 903-907.
Wang X, Zhang Y, Li JM. Experimental establishment of animal model of temporomandibular joint ankylosis secondary to condylar sagittal fracture[J]. J Peking Univ (Health Sci), 2011, 43(6):903-907.
[3] Arakeri G, Brennan PA. The role of concomitant mandibular fractures in disc displacement and development of TMJ ankylosis secondary to sagittal fractures of the mandibular condyle[J]. Int J Oral Maxillofac Surg, 2011, 40(11):1333-1335.
[4] Duan DH, Zhang Y. A clinical investigation on disc displacement in sagittal fracture of the mandibular condyle and its association with TMJ ankylosis development[J]. Int J Oral Maxillofac Surg, 2011, 40(2):134-138.
[5] 景捷, 趙洪偉, 孫剛, 等. 脫位性髁突矢狀骨折手術治療的近期療效觀察[J]. 華西口腔醫學雜志, 2007, 25(1):58-60.
Jing J, Zhao HW, Sun G, et al. Surgical treatment of dislocation sagittal fracture of the mandibular condyle[J]. West Chin J Stomatol, 2007, 25(1):58-60.
[6] Jing J, Han Y, Song Y, et al. Surgical treatment on displaced and dislocated sagittal fractures of the mandibular condyle [J]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2011, 111(6):693-699.
[7] Pereira MD, Marques A, Ishizuka M, et al. Surgical treatment of the fractured and dislocated condylar process of the mandible[J]. J Craniomaxillofac Surg, 1995, 23(6):369-376.
[8] Vesnaver A. Open reduction and internal fixation of intraarticular fractures of the mandibular condyle: our first experiences[J]. J Oral Maxillofac Surg, 2008, 66(10):2123-2129.
[9] Luo S, Li B, Long X, et al. Surgical treatment of sagittal fracture of mandibular condyle using long-screw osteosynthesis[J]. J Oral Maxillofac Surg, 2011, 69(7):1988-1994.
[10] Meng FW, Liu YP, Hu KJ, et al. Use of a temporary screw for alignment and fixation of sagittal mandibular condylar fractures with lateral screws[J]. Int J Oral Maxillofac Surg, 2010, 39(6):548-553.
[11] Xin P, Jiang B, Dai J, et al. Finite element analysis of type B condylar head fractures and osteosynthesis using two positional screws[J]. J Craniomaxillofac Surg, 2014, 42(5):482-488.
[12] Liu CK, Jing CX, Li W, et al. Observational study of surgical treatment of sagittal fractures of mandibular condyle [J]. J Craniofac Surg, 2015, 26(4):e359-e364.
[13] He D, Cai Y, Yang C. Analysis of temporomandibular joint ankylosis caused by condylar fracture in adults[J]. J Oral Maxillofac Surg, 2014, 72(4):763.e1-763.e9.
[14] He D, Ellis E 3rd, Zhang Y. Etiology of temporomandibular joint ankylosis secondary to condylar fractures: the role of concomitant mandibular fractures[J]. J Oral Maxillofac Surg, 2008, 66(1):77-84.
[15] Ferretti C, Bryant R, Becker P, et al. Temporomandibular joint morphology following post-traumatic ankylosis in 26 patients[J]. Int J Oral Maxillofac Surg, 2005, 34(4):376-381.
[16] Baker AW, McMahon J, Moos KF. Current consensus on the management of fractures of the mandibular condyle. A method by questionnaire[J]. Int J Oral Maxillofac Surg, 1998, 27(4):258-266.
[17] Vesnaver A, Ah?an U, Rozman J. Evaluation of surgical treatment in mandibular condyle fractures[J]. J Craniomaxillofac Surg, 2012, 40(8):647-653.
[18] Liu Y, Bai N, Song G, et al. Open versus closed treatment of unilateral moderately displaced mandibular condylar fractures: a meta-analysis of randomized controlled trials[J]. Oral Surg Oral Med Oral Pathol Oral Radiol, 2013, 116(2): 169-173.
[19] Meng FW, Zhao JL, Hu KJ, et al. A new hypothesis of mechanisms of traumatic ankylosis of temporomandibular joint[J]. Med Hypotheses, 2009, 73(1):92-93.
[20] Liu CK, Liu P, Meng FW, et al. The role of the lateral pterygoid muscle in the sagittal fracture of mandibular condyle (SFMC) healing process[J]. Br J Oral Maxillofac Surg, 2012, 50(4):356-360.
[21] Wu D, Yang XJ, Cheng P, et al. The lateral pterygoid muscle affects reconstruction of the condyle in the sagittal fracture healing process: a histological study[J]. Int J Oral Maxillofac Surg, 2015, 44(8):1010-1015.
(本文編輯 吳愛華)
Extramedullary fixation combined with intramedullary fixation in the surgical reduction of sagittal mandibular condylar fractures
Chen Chuanjun1, Chen Xiaoyang2, Chen Jing3.
(1. Stomatological School, Wannan Medical College, Wuhu 241002, China; 2. Dept. of Oral and Maxillofacial Surgery, The Third Affiliated Hospital of Anhui Medical University, Hefei 230061, China; 3. Dept. of Stomatology, Anhui Jimin Tumor Hospital, Hefei 230011, China)
Supported by: National Natural Science Foundation of China (815500037). Correspondence: Chen Chuanjun, E-mail: ccj6318 @sina.com.
Objective This study aimed to evaluate the clinical effect of extramedullary fixation combined with intramedullary fixation during the surgical reduction of sagittal mandibular condylar fractures. Methods Twenty-four sagittal fractures of the mandibular condyle in18 patients were fixed by two appliances: intramedullary with one long-screw osteosynthesis or Kirschner wire and extramedullary with one micro-plate. The radiologically-recorded post-operative stability-associated complications included the screw/micro-plate loosening, micro-plate twisting, micro-plate fractures, and fragment rotation. The occluding relations, the maximalinter-incisal distances upon mouth opening, and the mandibular deflection upon mouth opening were evaluated based on follow-up clinical examination. Results Postoperative panoramic X-ray and CT scans showed good repositioning of the fragment, with no redislocation or rotation, no screw/plate loosening, and no plate-twisting or fracture. Clinical examination showed that all patients regained normal mandibular movements, ideal occlusion, and normal maximal inter-incisal distances upon mouth opening. Conclusion Extramedullary fixation combined with intramedullary fixation is highly recommended for sagittal condylar fractures because of the anti-rotation effect of the fragment and the reasonable placement of the fixation appliances.
sagittal condylar fracture; rigid internal fixation; intramedullary fixation; extramedullary fixation
R 782.4
A [doi] 10.7518/hxkq.2016.05.008
2016-05-23;
2016-07-24
國家自然科學基金(815500037)
陳傳俊,教授,博士,E-mail:ccj6318@sina.com
陳傳俊,教授,博士,E-mail:ccj6318@sina.com

