阿爾茲海默病睡眠障礙的機制與治療進展
孫文靜, 賀 斌, 尹 又
第二軍醫大學長征醫院神經內科,上海 200003
?
·綜述·
阿爾茲海默病睡眠障礙的機制與治療進展
孫文靜, 賀斌, 尹又*
第二軍醫大學長征醫院神經內科,上海200003
阿爾茲海默病(Alzheimer's disease, AD)是一種與年齡高度相關的、以進行性認知功能障礙和記憶力損害為主的中樞神經系統變性疾病,又稱為老年性癡呆。調查顯示,40%以上的AD患者合并不同程度的睡眠問題(睡眠結構改變、晝夜節律紊亂或睡眠呼吸障礙),可導致患者認知與行為能力加速惡化、神經-內分泌系統功能失調、情緒易怒和低落,甚至導致死亡。由于目前AD的一線治療藥物療效欠佳,且近10余年幾乎所有的AD新藥研發無明顯陽性結果,故如何有效改善AD伴隨癥狀亦成為臨床延緩AD進展的治療重點之一。近5年針對睡眠與AD的關系及相關藥物、非藥物治療等研究日益受到重視。本文就目前對于AD患者睡眠障礙的發病機制、治療現狀作一綜述。
睡眠障礙;阿爾茲海默病;機制;治療
阿爾茲海默病(Alzheime's disease,AD)是最常見的癡呆類型。40%~80%的AD患者伴有不同程度的睡眠障礙,輕度AD即出現睡眠時間及結構紊亂[1]。目前,AD相關睡眠障礙的診斷主要依據Yesavage等[2]制定的標準。AD相關睡眠障礙中,尤以睡眠-覺醒節律紊亂、日落綜合征等給患者及其家屬的生活帶來的身心及經濟負擔更為沉重[3]。
1 AD藥物研發進展
近10余年針對不同靶點的AD藥物的研發均進展緩慢,且療效評估中未涉及AD睡眠障礙的改善報道(表1)[4-6]。
2 AD睡眠障礙的可能發病機制
AD睡眠障礙的可能發病機制包括生物節律中樞的紊亂、松果體區褪黑素(melatonine,MT)及其受體的改變、授時因子(zeitgeber)的變化以及基因因素等,其中睡眠/覺醒節律紊亂是其核心假說[7]。
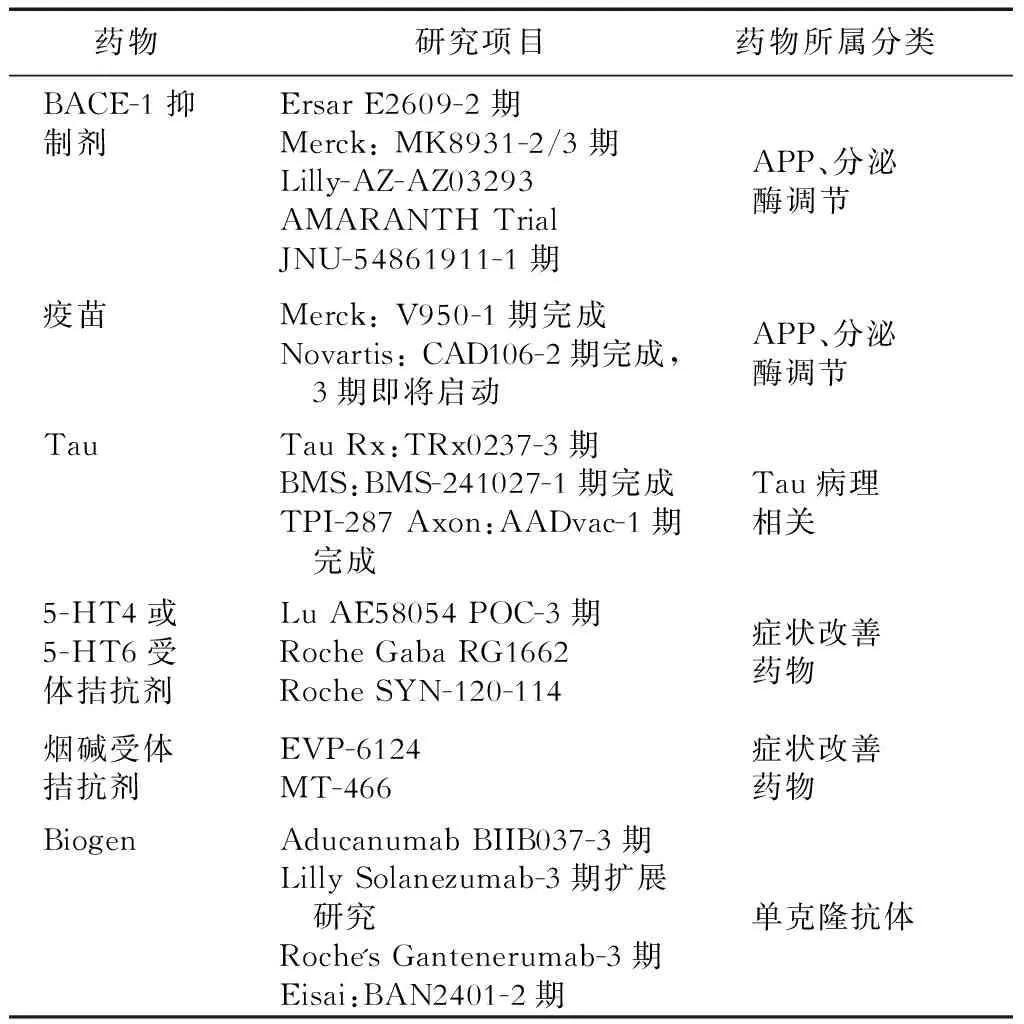
表1 近10年AD睡眠障礙新藥研發報告(1期、2期)
2.1生物節律中樞紊亂作為生物節律的起始點,AD患者的視交叉上核神經元數目明顯減少,并出現神經纖維纏結和β淀粉樣蛋白沉積。
2.2褪黑素及其受體改變褪黑素由松果體分泌后通過其受體MT1(占主要部分)和MT2調控晝夜節律。AD患者腦脊液中褪黑素水平僅占同齡健康人的1/5,MT1的表達也明顯降低,晚期神經元的數量明顯減少。
2.3授時因子變化光照是最強的授時因子,而AD患者常不愿外出,且伴有視網膜和視神經病變、視野缺損等[8],導致光照作用減弱。2.4基因因素基因可能決定AD個體睡眠障礙的嚴重程度。轉基因鼠睡眠調節紊亂較野生型鼠更早,進一步證實AD患者睡眠障礙與基因密切相關[5]。
3 AD睡眠障礙的藥物治療
目前,目前約有10余項較大規模的AD睡眠障礙相關臨床藥物研究,涉及膽堿酯酶抑制劑、褪黑素、抗精神病藥及非藥物療法等,其中涉及681例患者的6項隨機對照試驗(RCT)研究中僅有一半陽性結果(表2)。
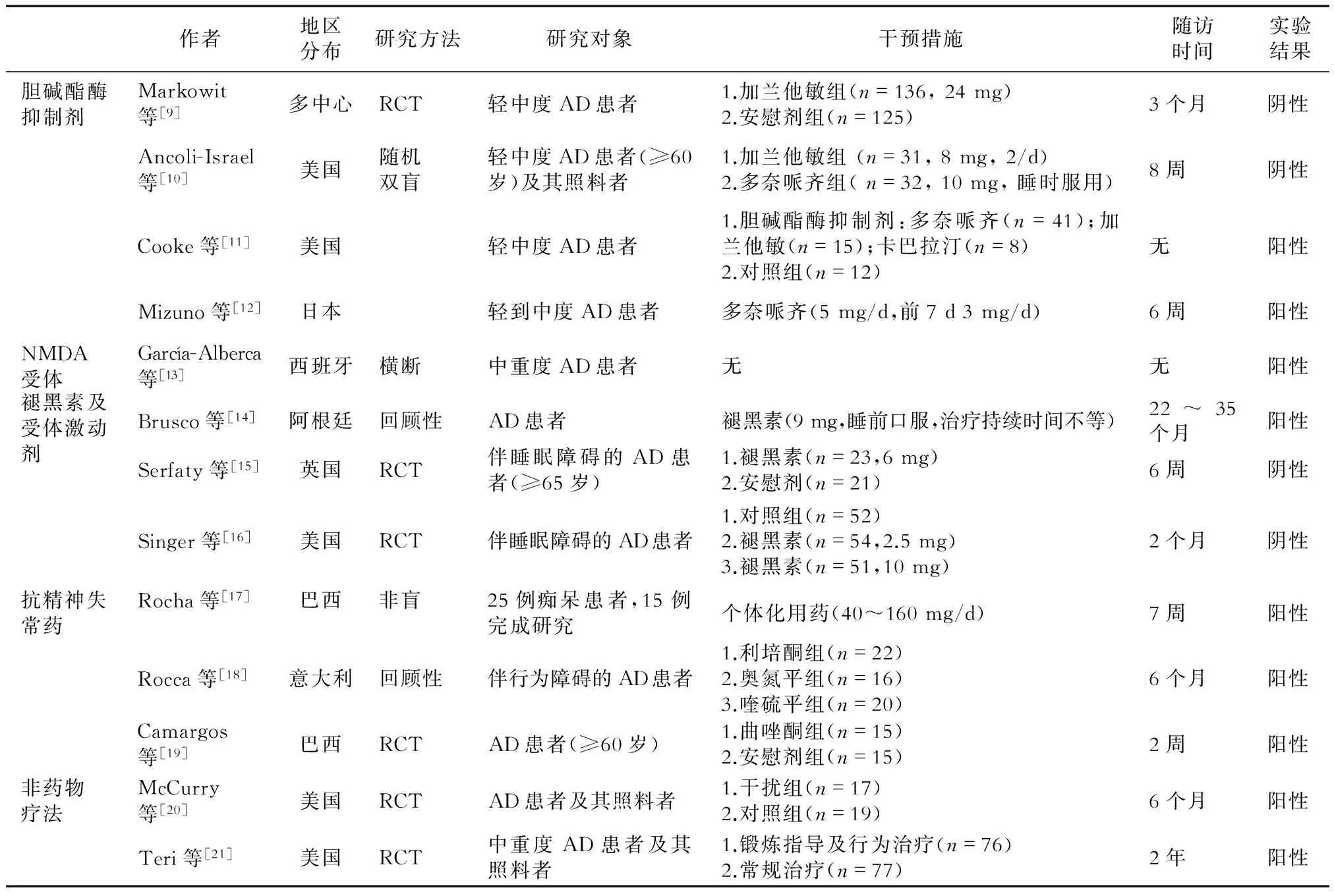
表2 AD睡眠障礙的大規模臨床研究
3.1改善認知癥狀的藥物
3.1.1膽堿酯酶抑制劑基底前腦作為膽堿能傳導通路的發源地,可能存在膽堿能/腺苷/睡眠-覺醒的控通路。兩項對加蘭他敏的臨床試驗研究均為陰性結果[9-10]。Cooke等[11]對分別服用加蘭他敏、重酒石酸卡巴拉汀和多奈哌齊的AD患者的睡眠結構進行觀察,發現AD患者快速動眼睡眠時間均增加,而非快速動眼時間1期減少,2期增加;多奈哌齊組比加蘭他敏組1期睡眠減少,較安慰劑組2期睡眠增加,表明多奈哌齊對患者睡眠有一定益處。 Mizuno等[12]也證實,5 mg多奈哌齊能增加患者的快速動眼睡眠時間百分比,提高睡眠效率,減少睡眠片段化。
3.1.2NMDA受體激動劑美金剛胺是第1個被證實對AD(尤其是中、重度AD)患者有顯著療效的藥物。美金剛胺可以阻止過量谷氨酸等的傳遞而達到保護神經元的作用。García-Alberca等[13]研究表明,AD患者使用美金剛后睡眠紊亂量表(神經精神、神經心理及功能狀態)評分均下降。
3.2褪黑素及其受體激動劑
3.2.1褪黑素AD睡眠障礙的主要因素是褪黑素合成和分泌減少,導致正常生物節律紊亂。一項包含14例參與者的回顧性研究[14]發現,每日口服9 mg褪黑素能明顯改善睡眠質量。但另一項對比研究[15]中,AD睡眠障礙每日口服6 mg褪黑素7周后,睡眠參數無變化,分別服用2.5 mg、5 mg和10 mg褪黑素8周后亦睡眠無顯著改善[16]。
3.2.2褪黑素受體激動劑AD患者體內不僅褪黑素水平下降[22],其受體表達也明顯下降,導致患者生理節律紊亂加重。瑞美替昂是已經被美國食品和藥品管理局(FDA)認證的治療失眠的藥物。瑞美替昂對MT1及MT2均有激動作用,但目前對其療效的觀察時間未超過35 d[23]。
3.3抗精神失常藥


4 非藥物治療
4.1光照光照主要通過視網膜下丘腦束引起視交叉上核神經細胞膜去極化,增強神經元發放率,并阻止年齡相關的精氨酸加壓素(AVP)表達,從而改善老年人的睡眠、神經內分泌、體溫及睡眠-覺醒節律。AD患者上述正常節律常較健康老年人破壞更為嚴重,對光照治療反應良好。McCurry等[20]證實,AD睡眠障礙患者可以進行光照等治療。
4.2其他方法研究[21]顯示,增加體育鍛煉不僅對老年人的睡眠-覺醒節律有明顯的改善作用,而且可以提高老年人的身心健康及生活熱情,但此研究沒有進行睡眠相關參數的評估。此外,踱步似乎能改善AD患者睡眠-覺醒周期的同步化[29]。通過經皮電刺激激活AD患者背部胸1~胸5脊髓神經元也可以改善睡眠節律[30]。有研究[31]初步表明,針灸可以通過增加夜間褪黑素的分泌而減少失眠及焦慮。也有研究[32]通過直接干預體溫(如熱水澡)來提高老年人的睡眠質量。
AD患者睡眠障礙的發生率高、危害大,盡管不斷對其病因、發病機制進行探索,但仍未找到較好的治療方法。目前常用的藥物各有利弊,應針對AD睡眠障礙表現的差異選擇藥物。膽堿酯酶抑制劑中的多奈哌齊在改善認知功能的同時有助于調節睡眠,有望成為該類AD患者的基礎治療藥物;褪黑素可提高患者的睡眠及認知能力,但治療周期較長;患者對小劑量(40 mg)齊拉西酮的耐受性良好,且照料者的負擔較輕,但類帕金森表現等不良反應常見;小劑量非典型抗精神病藥對伴有行為障礙或夜間睡眠-覺醒紊亂的AD患者更優;曲唑酮是目前最受肯定的AD睡眠障礙輔助藥物,其能改善AD患者的睡眠質量和睡眠結構,且無認知損傷等不良反應。總之,AD睡眠障礙的治療正逐漸受到關注,其作為AD輔助治療的意義日益凸顯,但治療方案尚缺乏大樣本、前瞻性以及對照研究的支持。
[1]Petit D, Gagnon JF, Fantini ML, et al. Sleep and quantitative EEG in neurodegenerative disorders[J].J Psychosom Res,2004,56(5):487-496.
[2]Yesavage JA, Friedman L, Ancoli-Israel S, et al. Development of diagnostic criteria for defining sleep disturbance in Alzheimer's disease[J].J Geriatr Psychiatry Neurol,2003,16(3):131-139.
[3]Ostrowski M, Mietkiewicz MC. Night of the Alzheimer's patient: the nightmare of the caregiver via the caregivers'guides[J].Geriatr Psychol Neuropsychiatr Vieil,2015,13(2):179-186.
[4]Castello MA, Jeppson JD, Soriano S. Moving beyond anti-amyloid therapy for the prevention and treatment of Alzheimer's disease[J].BMC Neurol,2014,14:169.
[5]De Strooper B. Lessons from a failed γ-secretase Alzheimer trial[J].Cell, 2014,159(4):721-726.
[6]尹又, 黃流清, 李澎, 等. 帕金森病患者睡眠障礙的研究進展[J].中華行為醫學與腦科學雜志,2014,23(1):91-93.
[7]Wu YH, Swaab DF. Disturbance and strategies for reactivation of the circadian rhythm system in aging and Alzheimer's disease[J].Sleep Med,2007,8(6):623-636.
[8]Valenti DA. Alzheimer's disease: visual system review[J].Optometry,2010,81(1):12-21.
[9]Markowitz JS, Gutterman EM, Lilienfeld S, et al. Sleep-related outcomes in persons with mild to moderate Alzheimer disease in a placebo-controlled trial of galantamine[J]. Sleep,2003,26(5):602-606.
[10]Ancoli-Israel S, Amatniek J, Ascher S, et al. Effects of galantamine versus donepezil on sleep in patients with mild to moderate Alzheimer disease and their caregivers: a double-blind, head-to-head, randomized pilot study[J].Alzheimer Dis Assoc Disord,2005,19(4):240-245.
[11]Cooke JR, Loredo JS, Liu L, et al. Acetylcholinesterase inhibitors and sleep architecture in patients with Alzheimer's disease[J].Drugs Aging,2006,23(6):503-511.
[12]Mizuno S, Kameda A, Inagaki T, et al. Effects of donepezil on Alzheimer's disease: the relationship between cognitive function and rapid eye movement sleep[J].Psychiatry Clin Neurosci,2004,58(6):660-665.
[13]García-Alberca JM, Lara JP, Cruz B, et al. Sleep disturbances in Alzheimer's disease are associated with neuropsychiatric symptoms and antidementia treatment[J].J Nerv Ment Dis,2013,201(3):251-257.
[14]Brusco LI, Fainstein I, Márquez M, et al. Effect of melatonin in selected populations of sleep-disturbed patients[J].Biol Signals Recept,1999,8(1-2):126-131.
[15]Serfaty M, Kennell-Webb S, Warner J, et al. Double blind randomised placebo controlled trial of low dose melatonin for sleep disorders in dementia[J].Int J Geriatr Psychiatry,2002,17(12):1120-1127.
[16]Singer C, Tractenberg RE, Kaye J, et al. A multicenter, placebo-controlled trial of melatonin for sleep disturbance in Alzheimer's disease[J].Sleep,2003,26(7):893-901.
[17]Rocha FL, Hara C, Ramos MG, et al. An exploratory open-label trial of ziprasidone for the treatment of behavioral and psychological symptoms of dementia[J].Dement Geriatr Cogn Disord,2006,22(5-6):445-448.
[18]Rocca P, Marino F, Montemagni C,et al.Risperidone, olanzapine and quetiapine in the treatment of behavioral and psychological symptoms in patients with Alzheimer's disease: preliminary findings from a naturalistic, retrospective study[J]. Psychiatry Clin Neurosci,2007, 61(6):622-629.
[19]Camargos EF, Pandolfi MB, Freitas MP, et al. Trazodone for the treatment of sleep disorders in dementia: an open-label, observational and review study[J]. Arq Neuropsiquiatr, 2011,69(1):44-49.
[20]McCurry SM, Gibbons LE, Logsdon RG, et al. Nighttime insomnia treatment and education for Alzheimer's disease: a randomized, controlled trial[J].J Am Geriatr Soc,2005,53(5):793-802.
[21]Teri L, Gibbons LE, McCurry SM, et al. Exercise plus behavioral management in patients with Alzheimer disease: a randomized controlled trial[J].JAMA,2003,290(15):2015-2022.
[22]Moraes W, Poyares D, Sukys-Claudino L, et al. Donepezil improves obstructive sleep apnea in Alzheimer disease: a double-blind, placebo-controlled study[J].Chest, 2008,133(3):677-683.
[23]Wurtman R. Ramelteon: a novel treatment for the treatment of insomnia[J]. Expert Rev Neurother,2006,6(7):957-964.
[24]Yin Y, Liu Y, Zhuang J, et al. Low-dose atypical antipsychotic risperidone improves the 5-year outcome in Alzheimer's disease patients with sleep disturbances[J]. Pharmacology,2015,96(3-4):155-162.
[25]Camargos EF, Louzada LL, Quintas JL,et al. Trazodone improves sleep parameters in Alzheimer disease patients: a randomized, double-blind, and placebo-controlled study[J].Am J Geriatr Psychiatry,2014,22(12):1565-1574.
[26]Grippe TC, Gon?alves BS, Louzada LL, et al. Circadian rhythm in Alzheimer disease after trazodone use[J].Chronobiol Int,2015,32(9):1311-1314.
[27]Raji MA, Brady SR. Mirtazapine for treatment of depression and comorbidities in Alzheimer disease[J].Ann Pharmacother,2001,35(9):1024-1027.
[28]Defrancesco M, Marksteiner J, Fleischhacker WW, et al. Use of Benzodiazepines in Alzheimer's Disease: A Systematic Review of Literature[J].Int J Neuropsychopharmacol, 2015,18(10):pyv055.
[29]Werth E, Savaskan E, Knoblauch V, et al. Decline in long-term circadian rest-activity cycle organization in a patient with dementia[J].J Geriatr Psychiatry Neurol,2002,15(1):55-59.
[30]Clancy JA, Mary DA, Witte KK, et al. Non-invasive vagus nerve stimulation in healthy humans reduces sympathetic nerve activity[J].Brain Stimul,2014,7(6):871-877.
[31]Spence DW, Kayumov L, Chen A, et al. Acupuncture increases nocturnal melatonin secretion and reduces insomnia and anxiety: a preliminary report[J].J Neuropsychiatry Clin Neurosci,2004,16(1):19-28.
[32]Van Someren EJ. More than a marker: interaction between the circadian regulation of temperature and sleep, age-related changes, and treatment possibilities[J].Chronobiol Int,2000,17(3):313-354.
[本文編輯]廖曉瑜,姬靜芳
Mechanism and treatment of sleep disorders in Alzheimer’s disease
SUN Wen-jing, HE Bin, YIN You*
Department of Neurology, Changzheng Hospital, Second Military Medical University, Shanghai 200003, China
Alzheimer's disease (AD) is a neurodegenerative disease highly correlated with age and characterized by progressive impairment in memory and cognition, also known as senile dementia. Survey shows more than 40% of AD patients with varying degrees of sleep problems (sleep structure changes, circadian rhythm disorder, sleep apnea and so on), which can lead to accelerated cognitive and behavioral deterioration, the nerve-endocrine system dysfunction, emotional irritability and depression, and even death. Due to the poor efficacy of first-line treatment drugs, and no significant positive results were achieved in AD drug development over the past ten years, how to effectively improve the associated symptoms of AD has become one of the therapeutic targets for delaying the progression of AD. In the past 5 years, research on the relationship between sleep and AD, related drugs and non-drug therapy has attracted increasing attention. In this paper, a review of the pathogenesis and clinical treatment of sleep disorders in patients with AD will be presented.
sleep disorders; Alzheimer's disease; pathogenesis; treatment
2016-01-28[接受日期]2016-07-25
國家自然科學基金(30900473,81371459,81171252), 國家科技部重大專項(2011ZXJ09202-015),國家科技支撐計劃項目(2015BAI13B01),上海市科學技術委員會重點項目(11411950203),上海市自然科學基金(15ZR1414600). Supported by National Natural Science Foundation of China(30900473,81371459,81171252), National Ministry of Science and Technology Major Project(2011ZXJ09202-015), National Key Technology Research and Development Program of Ministry of Science and Technology of China (2015BAI13B01), Medical Key Project of Shanghai Municipal Science and Technology Commission(11411950203)and Natural Science Foundation of Shanghai(15ZR1414600).
孫文靜,碩士生. E-mail:sunwj1121@163.com
Corresponding author). Tel: 021-64041990, E-mail:yinyou179@163.com
10.12025/j.issn.1008-6358.2016.20160098
R 749.1+6
A

