文拉法辛與選擇性五羥色胺再攝取抑制劑對(duì)抑郁癥轉(zhuǎn)換策略療效的Meta分析
何如東陳美玲周歡
·論 著·
文拉法辛與選擇性五羥色胺再攝取抑制劑對(duì)抑郁癥轉(zhuǎn)換策略療效的Meta分析
何如東*陳美玲*周歡*
目的 系統(tǒng)評(píng)價(jià)文拉法辛 (venlafaxine)與選擇性5-羥色胺再攝取抑制劑 (selective serotonin reuptake inhibitor,SSRI)對(duì)抑郁癥轉(zhuǎn)換策略療效的差異。方法 檢索1990~2010年的MEDLINE和中文文獻(xiàn),納入文拉法辛與SSRI對(duì)抑郁癥轉(zhuǎn)換策略治療效果的隨機(jī)對(duì)照試驗(yàn)并進(jìn)行Meta分析。結(jié)果 8個(gè)隨機(jī)對(duì)照試驗(yàn)符合納入標(biāo)準(zhǔn),共5350例抑郁癥患者。Meta分析結(jié)果顯示,文拉法辛的臨床治愈率是52.5%,SSRI的臨床治愈率是43.3%,二者的差異有統(tǒng)計(jì)學(xué)意義(OR=1.38,95%CI:1.20~1.58,P<0.01);文拉法辛的有效率是67.8%,SSRI的有效率是59.6%,二者的差異有統(tǒng)計(jì)學(xué)意義(OR=1.33,95%CI:1.15~1.53,P<0.01)。 結(jié)論 文拉法辛較SSRI對(duì)抑郁癥轉(zhuǎn)換策略有更高的臨床治愈率與有效率。
文拉法辛 SSRI 轉(zhuǎn)換策略 難治性抑郁癥
隨著精神藥理學(xué)的發(fā)展,特別是選擇性5-羥色胺再攝取抑制劑 (selective serotonin reuptake inhibitor,SSRI)的廣泛應(yīng)用,抑郁癥治療已經(jīng)得到了明顯的進(jìn)展,但臨床上仍有40%~50%的抑郁癥患者首次治療療效不佳甚至無(wú)效[1-2]。而某些難治性抑郁癥 (treatment-resistant depression, TRD)經(jīng)歷兩種類型的抗抑郁藥足量足程治療無(wú)效。對(duì)于上述兩類患者實(shí)施轉(zhuǎn)換策略是較優(yōu)的選擇[3]。目前抗抑郁藥有幾大類作用機(jī)制不同的藥物可以選擇,在轉(zhuǎn)換藥物的選擇上,不同作用機(jī)制的藥物在療效上是否存在差異?近年來(lái),5-羥色胺與去甲腎上腺素再攝取抑制劑(serotonin-norepinephrine reuptake inhibitors,SNRI)文拉法辛已在臨床一線廣泛應(yīng)用。有證據(jù)表明文拉法辛在療效上比SSRI更好[4-5]。在轉(zhuǎn)換藥物的選擇上,首選文拉法辛是否會(huì)比SSRI更有優(yōu)勢(shì)?為了探討文拉法辛與SSRI在轉(zhuǎn)換策略療效的差異,本研究對(duì)既往研究的文獻(xiàn)進(jìn)行系統(tǒng)評(píng)價(jià)。
1 資料與方法
1.1 研究文獻(xiàn) 納入標(biāo)準(zhǔn):①隨機(jī)對(duì)照試驗(yàn)(randomized controlled trials,RCT);②研究對(duì)象符合美國(guó)精神障礙診斷與統(tǒng)計(jì)手冊(cè)第4版(DSM-IV)、國(guó)際疾病分類系統(tǒng)(ICD-10)和中國(guó)精神障礙分類與診斷標(biāo)準(zhǔn)第3版(CCMD-3)的抑郁癥診斷標(biāo)準(zhǔn),有明確的排除標(biāo)準(zhǔn);③對(duì)象入組前經(jīng)歷一次或以上足量足程的抗抑郁藥治療無(wú)效后接受轉(zhuǎn)換治療,轉(zhuǎn)換藥物包括文拉法辛與SSRI類藥物;④納入的文獻(xiàn)要有明確的評(píng)定工具、結(jié)局指標(biāo)、藥物不良反應(yīng)統(tǒng)計(jì)與退出原因說(shuō)明。排除標(biāo)準(zhǔn):①非隨機(jī)對(duì)照試驗(yàn);②結(jié)局指標(biāo)數(shù)據(jù)不完整。
1.2 文獻(xiàn)檢索 計(jì)算機(jī)檢索MEDLINE與萬(wàn)方數(shù)據(jù)庫(kù)的核心期刊,檢索年限1990~2010年。英文檢索關(guān)鍵詞:treatment-resistant depression、refractory depression、difficult-to-treat depression、antidepressant、switching、switching strategies、venlafaxine、SSRI;中文檢索關(guān)鍵詞:難治性抑郁癥、轉(zhuǎn)換治療、轉(zhuǎn)換策略、文拉法辛、SSRI。
1.3 文獻(xiàn)質(zhì)量評(píng)估 采用Jadad評(píng)估標(biāo)準(zhǔn):①隨機(jī):描述了具體的隨機(jī)方法且隨機(jī)方法合理2分,只描述隨機(jī)1分;②雙盲:描述了具體的雙盲方法并且方法合理2分,只描述雙盲1分;③退出與失訪:對(duì)退出與失訪的例數(shù)與理由進(jìn)行描述1分,沒描述0分。
1.4 統(tǒng)計(jì)學(xué)處理 采用Revman4.2軟件進(jìn)行檢索文獻(xiàn)的數(shù)據(jù)處理和統(tǒng)計(jì)學(xué)分析,計(jì)數(shù)資料用比值比(odds ratio,OR)與95%可信區(qū)間(CI)表示。采用卡方檢驗(yàn)分析各研究間的異質(zhì)性,如各研究間有統(tǒng)計(jì)學(xué)同質(zhì)性時(shí)(P≥0.05)時(shí),采用固定效應(yīng)模型(fixed effects model)作 Meta分析;如各研究間有統(tǒng)計(jì)學(xué)異質(zhì)性時(shí)(P<0.05)時(shí),采用隨機(jī)效應(yīng)模型(randomized effects model)作Meta分析。
2 結(jié)果
2.1 文獻(xiàn)檢驗(yàn)結(jié)果 初步檢索出25篇文拉法辛與SSRI類藥物對(duì)抑郁癥轉(zhuǎn)換策略療效的文獻(xiàn),有8篇文獻(xiàn)符合納入標(biāo)準(zhǔn)[6-13],中文核心期刊無(wú)相關(guān)文獻(xiàn)。
2.2 納入文獻(xiàn)的特征與方法學(xué)質(zhì)量評(píng)估 8篇文獻(xiàn)共納入5350例抑郁癥患者,總計(jì)接受文拉法辛治療人數(shù)2288例,接受SSRI治療人數(shù)1772例。見表1。
2.3 結(jié)局指標(biāo)的Meta分析 納入文獻(xiàn)中有6個(gè)試驗(yàn)提供臨床治愈率與有效率,1個(gè)試驗(yàn)提供臨床治愈率,1個(gè)試驗(yàn)提供有效率。提取7個(gè)文獻(xiàn)臨床治愈率數(shù)據(jù)進(jìn)行Meta分析,森林圖結(jié)果示各研究間異質(zhì)性檢驗(yàn)無(wú)統(tǒng)計(jì)學(xué)意義(I2=0%,P=0.48),采用固定模型作Meta分析。以臨床治愈率為結(jié)局指標(biāo),文拉法辛組治愈人數(shù)為1115例,治愈率52.5%(1115/2122);SSRI治愈人數(shù)694例,治愈率43.3%(694/1604),差異有統(tǒng)計(jì)學(xué)意義(OR=1.38,95%CI:1.20~1.58,P<0.01)。見圖1。
提取7個(gè)文獻(xiàn)有效率數(shù)據(jù)進(jìn)行Meta分析,森林圖結(jié)果示各研究間異質(zhì)性檢驗(yàn)無(wú)統(tǒng)計(jì)學(xué)意義 (I2=11.6%,P=0.34),采用固定模型作Meta分析。以有效率作為結(jié)局指標(biāo),文拉法辛有效人數(shù)1512例,有效率67.8%(1512/2231);SSRI有效人數(shù)1023例,有效率59.6%(1023/1717),差異有統(tǒng)計(jì)學(xué)意義(OR=1.33,95%CI:1.15~1.53,P<0.01)。見圖2。
需要治療人數(shù) (number needed to treatment,NNT)的計(jì)算:提取文獻(xiàn)的臨床治愈率與有效率的數(shù)據(jù)Meta分析計(jì)算風(fēng)險(xiǎn)差異(RD),NNT=1/RD。以臨床治愈率為結(jié)局指標(biāo),兩組的臨床治愈率差異有統(tǒng)計(jì)學(xué)意義(RD=0.07,95%CI:0.04~0.11,P<0.01),NNT=14(95%CI:9~25)。以有效率為結(jié)局指標(biāo),兩組的有效率差異有統(tǒng)計(jì)學(xué)意義(RD=0.06,95%CI:0.03~0.09,P<0.01),NNT=17(95%CI:11~33)。
退出率的Meta分析:提取8個(gè)文獻(xiàn)的退出率數(shù)據(jù)進(jìn)行Meta分析,森林圖結(jié)果示各研究間異質(zhì)性檢驗(yàn)無(wú)統(tǒng)計(jì)學(xué)意義(I2=3.2%,P=0.40),采用固定模型作Meta分析,以退出率作為結(jié)局指標(biāo),兩類藥的差異無(wú)統(tǒng)計(jì)學(xué)意義 (OR=0.88,95%CI:0.78~1.00,P=0.05)。
3 討論
抗抑郁治療無(wú)效是一個(gè)難題,為此目前提出了一些治療策略與步驟,例如抑郁癥序貫治療(sequenced treatment alternatives to relieve depression,STAR*D),目的是通過轉(zhuǎn)換策略、增效策略、聯(lián)合策略等治療步驟提高患者的療效,特別是臨床治愈率。因?yàn)榕R床治愈較臨床有效有更好的功能恢復(fù)與良好預(yù)后、更少的復(fù)發(fā)和復(fù)燃風(fēng)險(xiǎn)、更少的衛(wèi)生資源使用率、低自殺和酒精藥物依賴風(fēng)險(xiǎn)率、更少的致殘癥狀[14]。

表1 文拉法辛與SSRI對(duì)抑郁癥轉(zhuǎn)換策略療效對(duì)照文獻(xiàn)特征
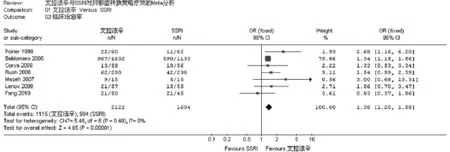
圖1 文拉法辛與SSRI對(duì)抑郁癥轉(zhuǎn)換策略的臨床治愈率的Meta分析
基于安全與耐受性的原因,SSRI類藥物目前已經(jīng)是抗抑郁治療的首選用藥。納入的8個(gè)試驗(yàn)的對(duì)象入組前SSRI使用率超過50%,其中有5個(gè)試驗(yàn)的對(duì)象入組前均經(jīng)歷SSRI治療無(wú)效[8-12]。對(duì)于SSRI治療無(wú)效的患者如采用轉(zhuǎn)換策略會(huì)面臨著同類與異類轉(zhuǎn)換的選擇,因?yàn)閾Q用另一個(gè)SSRI或其它類型的抗抑郁藥都有一定的效果[15-17],沒有明顯的證據(jù)證明哪類抗抑郁藥更有優(yōu)勢(shì)。至今轉(zhuǎn)換策略的對(duì)照研究仍少,所以有必要進(jìn)行系統(tǒng)評(píng)價(jià)。

圖2 文拉法辛與SSRI對(duì)抑郁癥轉(zhuǎn)換策略的有效率的Meta分析
本Meta分析納入的隨機(jī)對(duì)照試驗(yàn)中有5個(gè)試驗(yàn)采用雙盲設(shè)計(jì),方法學(xué)質(zhì)量良好。2個(gè)試驗(yàn)[7-8]雖然未采用盲法設(shè)計(jì),由于樣本量大,在轉(zhuǎn)換策略療效方面的結(jié)果仍有一定代表性。納入分析的試驗(yàn)有相同的結(jié)局指標(biāo),療效評(píng)定工具基本一致。需指出的是納入分析的試驗(yàn)間有一些特征上的差異:Poirier等[6]療程只有4周。Fang等[13]采用固定劑量治療,其中文拉法辛225 mg,帕羅西汀20 mg。Mazeh等[10]研究對(duì)象是老年抑郁癥。Brent等[11]研究對(duì)象是青少年抑郁癥。此外,本分析納入的試驗(yàn)統(tǒng)計(jì)學(xué)的同質(zhì)性好,合并效應(yīng)量的結(jié)果具有良好的證據(jù)的強(qiáng)度,故本研究對(duì)于文拉法辛與SSRI對(duì)轉(zhuǎn)換策略的療效的系統(tǒng)評(píng)價(jià)可信。
本Meta分析以臨床治愈率與有效率為結(jié)局指標(biāo)系統(tǒng)評(píng)價(jià)文拉法辛與SSRI對(duì)抑郁癥轉(zhuǎn)換策略療效的差異。納入分析的試驗(yàn)中,文拉法辛的臨床治愈率為24.8%~60%,有效率為28%~80%;SSRI的臨床治愈率為17.6%~52.1%,有效率為26.4%~71.1%。Meta分析結(jié)果顯示兩種藥物存在差異,文拉法辛較SSRI對(duì)抑郁癥轉(zhuǎn)換策略有更高的臨床治愈率(OR=1.38)與有效率(OR=1.33)。NNT計(jì)算結(jié)果顯示,與SSRI對(duì)照,抑郁癥患者采用文拉法辛治療增加1例得到臨床治愈的獲益需要治療的人數(shù)是14例,采用文拉法辛治療增加1例得到有效的獲益需要治療的人數(shù)是17例。結(jié)果顯示在轉(zhuǎn)換策略中采用文拉法辛治療更能讓抑郁癥患者在治療中獲益。Bauer等[18]納入5個(gè)試驗(yàn)Meta分析文拉法辛與其它類型抗抑郁藥 (主要是SSRI類藥物)對(duì)首次治療無(wú)效與TRD患者的療效差異,結(jié)果示文拉法辛有更高的臨床治愈率(OR=1.35,95%CI:1.20-1.52)與有效率(OR=1.35,95%CI:1.19-1.54)。Papakostas等[19]以相對(duì)危險(xiǎn)度(RR)為合并效應(yīng)量納入3個(gè)試驗(yàn)Meta分析文拉法辛與SSRI對(duì)SSRI治療無(wú)效患者的療效差異,結(jié)果示文拉法辛有更高的臨床治愈率 (RR=1.31,95%CI:1.02-1.67)。這2個(gè)Meta分析的結(jié)果都顯示文拉法辛在轉(zhuǎn)換策略上較SSRI更有優(yōu)勢(shì),本研究結(jié)果與二者一致。
抑郁癥治療決策是基于有效、安全與耐受的原則[20]。文拉法辛是一種5-羥色胺與去甲腎上腺素再攝取抑制劑,其雙重活性的作用機(jī)制對(duì)抑郁癥的治療效果較選擇性5-羥色胺再攝取抑制劑更有優(yōu)勢(shì)[4-5],在轉(zhuǎn)換策略上較SSRI有潛在的優(yōu)勢(shì)[21]。在安全性與耐受性方面,納入的試驗(yàn)統(tǒng)計(jì)文拉法辛與SSRI的副反應(yīng)主要是惡心、嘔吐、口干等消化系統(tǒng)癥狀;頭昏、頭痛等神經(jīng)系統(tǒng)癥狀。Fang等[13]報(bào)告文拉法辛食欲不振與頭昏的發(fā)生率較SSRI高,其它試驗(yàn)無(wú)差異。需指出的是Rush等[8]報(bào)告文拉法辛與SSRI各有2例自殺意念或自殺企圖。Brent等[11]報(bào)告文拉法辛有11例自殺意念或自殺企圖,SSRI有6例。各試驗(yàn)因嚴(yán)重藥物副作用的退出率無(wú)差異,提示文拉法辛是一種具有良好安全性與耐受性的抗抑郁藥。
由于目前轉(zhuǎn)換策略的對(duì)照研究較少,本Meta分析納入的文獻(xiàn)較少。2個(gè)大樣本試驗(yàn)的方法學(xué)設(shè)計(jì)上仍存不足,部分試驗(yàn)樣本量過小,結(jié)果難免偏倚。結(jié)論仍需要大樣本方法學(xué)設(shè)計(jì)合理的試驗(yàn)補(bǔ)充評(píng)價(jià)。
[1]Trivedi MH,Rush AJ,Wisniewski SR,et al.Evaluation of outcomes with citalopram for depression using measurementbased care in STAR*D:implications for clinical practice[J].Am J Psychiatry,2006 163(1):28-40.
[2]Kroenke K,West SL,Swindle R,et al.Similar effectiveness of paroxetine,fluoxetine,and sertraline in primary care:a randomized trial[J].JAMA,2001,286(23):2947-2955.
[3]American Psychiatric Association. Practice guideline for the treatment of patients with major depressive disorder (revision).American Psychiatric Association[J].Am J Psychiatry,2000,157(4 suppl):1-45.
[4]Thase ME,Entsuah AR,Rudolph RL.Remission rates during treatment with venlafaxine or selective serotonin reuptake inhibitors[J].Br J Psychiatry,2001,178(3):234-241.
[5]Nemeroff CB,Entsuah R,Benattia I,et al.Comprehensive analysis of remission(COMPARE)with venlafaxine versus SSRIs[J].Biol psychiatry,2008,63(4):424-434.
[6]Poirier MF,Boyer P.Venlafaxine and paroxetine in treatmentresistant depression.Double-blind,randomised comparison[J].Br J Psychiatry,1999,175(7):12-16.
[7]Baldomero EB,Ubago JG,Cercos CL,et al.Venlafaxine extended release versus conventional antidepressants in the remission of depressive disorders after previous antidepressant failure:ARGOS study[J].Depress Anxiety,2005,22(2):68-76.
[8]Rush AJ,Trivedi MH,Wisniewski SR,et al.Bupropion-SR,sertraline, or venlafaxine-XR after failure of SSRIs for depression[J].N Engl J Med,2006,354(12):1231-1242.
[9]Corya SA,Williamson D,Sanger TM,et al.A randomized,double-blind comparison of olanzapine/fluoxetine combination,olanzapine, fluoxetine, and venlafaxine in treatment-resistant depression[J].Depress Anxiety,2006,23(6):364-372.
[10]Mazeh D,Shahal B,Aviv A,et al.A randomized,singleblind,comparison of venlafaxine with paroxetine in elderly patients suffering from resistant depression[J].Int Clin Psychopharmacol,2007,22(6):371-375.
[11]Brent D,Emslie G,Clarke G,et al.Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression: the TORDIA randomized controlled trial[J].JAMA,2008,299(8):901-913.
[12]Lenox-smith AJ,Jiang Q.Venlafaxine extended release versus citalopram in patients with depression unresponsive to a selective serotonin reuptake inhibitor[J].Int Clin Psychopharmacol,2008,23(3):113-119.
[13]Fang Y,Yuan C,Xu Y,et al.Comparisons of the efficacy and tolerability of extended-release venlafaxine, mirtazapine,and paroxetine in treatment-resistant depression: a double-blind,randomized pilot study in a Chinese population[J].J Clin Psychopharmacol,2010,30(4):357-364.
[14]McClintock SM,Husain MM,Wisniewski SR,et al.Residual symptoms in depressed outpatients who respond by 50%but do not remit to antidepressant medication[J].J Clin Psychopharmacol,2011,31(2):180-186.
[15]Thase ME,Blomgren SL,Birkett MA,et al.Fluoxetine treatment of patients with major depressive disorder who failed initial treatment with sertraline[J].J Clin Psychiatry,1997,58(1):16-21.
[16]Thase ME,Rush AJ,Howland RH,et al.Double-blind switch study of imipramine or sertraline treatment of antidepressant-resistant chronic depression[J].Arch Gen Psychiatry,2002,59(3):233-239.
[17]Reynaert-Dupuis C,Zdanowicz N,Leyman S,et al.Efficacy and tolerance of venlafaxine in depressed patients switched from prior antidepressant treatment[J].Prim Care Psychiatry,2002,8(2):63-68.
[18]Bauer M,Tharmanathan P,Volz HP,et al.The effect of venlafaxine compared with other antidepressants and placebo in the treatment of major depression:a meta-analysis[J].Eur Arch Psychiatry Clin Neurosci,2009,259(3):172-185.
[19]Papakostas GI,F(xiàn)ava M,Thase ME.Treatment of SSRI-resistant depression:a meta-analysis comparing within-versus across-class switches[J].Biol Psychiatry,2008,63(7):699-704.
[20]Schatzberg AF.Safety and tolerability of antidepressants:weighing the impact on treatment decisions[J].J Clin Psychiatry,2007,68(Suppl 8):26-34.
[21]Connolly KR,Thase ME.If at first you don't succeed:a review of the evidence for antidepressant augmentation, combination and switching strategies.Drugs,2011,71(1):43-64.
The efficacy of venlafaxine and selective serotonin reuptake inhibitors in antidepressant switching strategies:a meta-analysis.
HE Rudong,CHEN Meiling,ZHOU Huan.The Chronic Disease Prevention and Treatment Center of Maoming,GuangDong,No 10 Lane 1 Jixing Road,Maoming 525000.China.Tel:0668-2305133.
Objective To systematically review the difference in efficacy between venlafaxine and selective serotonin reuptake inhibitors(SSRI)in antidepressant switching strategies.Methods We conducted a meta-analysis comparing the efficacy between venlafaxine and SSRI in antidepressant switching strategies.The randomized controlled trials (RCT) were identified through searches of MEDLINE and Chinese publications for the years 1990 to 2010.Results Eight RCTs involving 5350 patients with maior depressive met inclusion criteria.Results of meta-analysis showed that the remission rates were 52.5%and 43.3%for venlafaxine and SSRI, respectively.There were statistically significant difference(OR=1.38,95%CI:1.20~1.58,P<0.01)in remission rates between the two treatment groups.The response rates were 67.8%and 59.6%for venlafaxine and SSRI, respectively.There were statistically significant difference(OR=1.33,95%CI:1.15~1.53,P<0.01)in response rates between the two treatment groups.Conclusions Remission and response rates are significantly higher in venlafaxine than in SSRI in antidepressant switching strategies.
Venlafaxine SSRI Switching strategies Treatment-resistant depression
R794.4
A
2011-03-28)
(責(zé)任編輯:曹莉萍)
* 廣東省茂名市慢性病防治中心(茂名 524500)
(E-mail:hurudong@sina.com)