Neuromyelitis optica spectrum disorders and anti-myelin oligodendrocyte glycoprotein positive optic neuropathies
INTRODUCTION
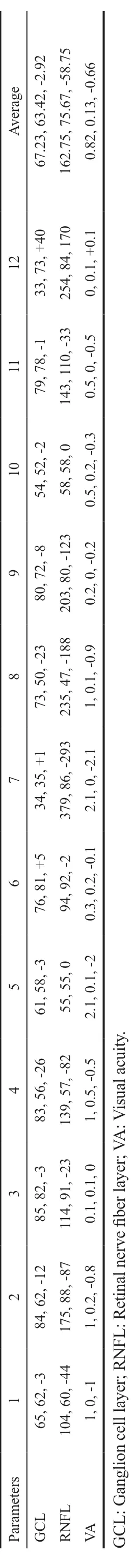
The authors found that presenting and final VA was not be correlated with RNFL or GCL. With regards to GCL, an average reduction of 2.92 and 7.75 μm was seen in the MOG and AQP4 group respectively. These are extremely modest differences and negligible when the standard error of the OCT machine is taken in account. The RNFL analysis showed a reduction of 58.75 μm in the MOG group as opposed to only 10.5 μm in the AQP4 group. However, this is not an indication of worsening disease but is in keeping with the predominance of OHN swelling in the MOG cohort. This swelling resides with time and is in keeping with the observed reduction in RNFL thickness. Therefore, the authors suggest that analysis of the GCL layer is a more accurate representation of nerve damage as opposed to RNFL, especially in the acute phase of the disease. Waiting 3mo to accurately interpret RNFL would be more appropriate
. RNFL may be used to assess subtle swelling of the nerve and to assess change in chronic disease.OCT is unquestionably finding its foothold in the monitoring of optic nerve disease, where it offers an excellent objective numerical interpretation of inner retinal layers. Loss of these unmyelinated axons is postulated to be secondary to an antegrade process
.
Optic Nerve Head Assessment Optic nerve head assessment is a fundamental aspect of every ocular exam and it is crucial when it comes to the assessment of optic neuropathies as the appearance of the nerve can give crucial hints with respect to aetiology of the disease. Similar topographic changes can appear in chronic or late-stage disease
and therefore it is essential that the disc is assessed at presentation with baseline fundal disc photos taken for comparison with its appearance in follow up visits.
Disease Course As previously stated, 2 of the 12 patients(16.67%) in the MOG cohort and 2 of the 4 patients (50%) in AQP4 cohort the had bilateral involvement at presentation.With regards number of relapses, 5 patients in the MOG cohort had a relapsing course (average of 1.6 relapses, range 1-3)while the remining 7 patients had a single attack (monophasic course) at the time of writing. Two of the patients (60%)who had a recurrent course had sequential progression to the contralateral eye. In the AQP4 group, 2 of the 4 patients(50%) had bilateral involvement at presentation. Three of the 4 patients (75%) had a recurrent course (average of 3 relapses,range 1-7) and 1 of these patients had sequential progression with multiple relapses. The remaining one patient had a monophasic course.
ON seen in MOG positive cases tend to have atypical findings.The 80% patients of those with MOG positive ON tend to have moderate to severe disc oedema
. Patients tend to have recurrent and bilateral attacks of ON
. These patients tend to be highly steroid responsive and can prove to be steroid dependant
.
2)將電熔套管從包裝袋中取出,并檢查確認配件內壁是干凈的。如有需要,可使用酒精擦拭紙擦拭電熔套管內壁,在開始焊接工藝前,確保清潔后的電熔套管內壁是完全干燥。
In contrast to typical ON, high dose intravenous glucocorticoids are recommended are at initial presentation in MOG and anti-Aquaporin 4 (AQP4) positive cases of ON
. Guidelines for treatment have proved difficult to establish due to the low number of patients and therefore the absence of randomised controlled clinical trials.
To describe all cases of anti-MOG antibody positive and AQP4 antibody positive ON that have presented to a specialist ophthalmology quaternary referral centre. This will consist of demographic data, clinical characteristics, ancillary tests [optical coherence tomography (OCT), perimetry and neuroimaging] and treatment/outcome.
SUBJECTS AND METHODS
Ethical Approval This study was a retrospective review and was conducted in accordance with the Declaration of Helsinki and the Irish Data Protection Act. The protocol of the study adhered to the tenets of the Declaration of Helsinki. This study adheres to the legal requirements of the General Data Protection Regulation (GDPR, articles 6 and 9).
新中式建筑以傳統文化理念的基礎,將我國傳統文化的元素通過現代藝術形式來表達出來,不但符合我國民眾切實的生活所需,又不落后于當前國內外主流審美理念,屬于一種具備獨特藝術方式并運用現代審美觀念來塑造的具有我國東方風貌的藝術形態。嶺南建筑多輕巧趣致,建筑與環境自然融合。本項目吸取兩者特點,力求塑造出融合時尚不失古典的嶺南新中式建筑風格。
Visual Field Testing Table 5 depicts the visual fields findings associated with each patient in both cohorts and the change in each. Of the MOG cohort, 5 of the 12 patients (41.67%) had generalised visual field depression or an enlarged blind spot(Figure 3). Five of the 12 (41.67%) fields demonstrated an improvement, 5 fields were unchanged from the baseline and 2 (16.67%) demonstrating deterioration in the follow up period. One field in the AQP4 (25%) group showed an improvement from baseline to final while the others remained unchanged.
A cross-sectional single-centre retrospective case series consisting of 16 patients including 12 anti-MOG positive patients, and 4 anti-AQP4 positive patients. Inclusion criteria consisted of all patients who had a positive anti-MOG or positive anti-AQP4 blood result for investigation of a unilateral or bilateral ON who attended the Royal Victoria Eye and Ear Hospital, Dublin, Ireland. Exclusion criteria consisted of patients with negative blood markers for the autoantibodies.There was no exclusion based on age or pre-existing comorbidity.At the initial and each follow up consultation the following parameters were recorded; visual acuity (VA) in logarithm of the minimum angle of resolution (logMAR), colour vision(Ishihara pseudoisochromatic testing), presence/absence of a relative afferent pupillary defect (RAPD), slit lamp biomicroscopy with optic nerve assessment, kinetic visual fields (Octopus Visual Field, Haag-Streit, Switzerland), OCT(Cirrus 5000, Carl Zeiss, Meditec, Dublin, CA, USA) analysis of the macula, ganglion cell layer (GCL) and the retinal nerve fibre layer (RNFL). Each of the patients had magnetic resonance imaging (MRI) scanning of the brain and optic nerves with gadolinium contrast. Colour vision was assessed using 14 of the 38 Ishihara plates and graded as mild (10-14/14), moderate (6-10/14) or severe (0-5/14) depending on number of plates correctly identified as outlined in parentheses.RAPD was assessed for its presence or absence and graded from 0 to 3 in terms of increasing severity
. Red desaturation was assessed using a red hat pin on a white background and participants were asked to compare colour intensity between each eye
.
3k 1H NMR(CDCl3) δ:9.48(d,J=5.1,1 H),8.46-8.44(m,1 H),8.05(d,J=5.1,1 H),7.94-7.87(m,2 H),7.75-7.42(m,4 H),7.40-7.38(m,2 H).
理解是描述對象的特征和由來,闡述此對象與相關對象之間的區別和聯系,是分析問題和解決問題的基礎,是創建數學思維的前提,是學習數學的根基,是為生活生產服務的源泉。理解是學生學習相關課程內容的背景,既有利于幫助學生理解相關內容,也促進其將所學知識運用于解決問題的過程中,無疑有利于提高學生的應用數學的意識和能力。
Statistical Analysis Data was collated and analysed using the statistical package STATA (StataCorp. 2013. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP).A statistically significant result was defined as
<0.05. Best corrected VA was recorded in the patient’s medical notes in Snellen format in metres which was subsequently converted to the logMAR for the purpose of statistical analysis. A VA of count fingers (CF), hand motion (HM), perception of light(PL) and no perception of light (NPL) were denoted 2.1, 2.4,2.7, and 3.0 on the logMAR scale, respectively.
RESULTS
Baseline Characteristics A total of 16 patients were include in the study. This consisted of 12 (75%) anti-MOG positive ON patients and 4 (25%) anti-AQP4 positive patients. These 16 patients comprised all recorded cases of antibody positive ON that had attended the Royal Victoria Ear and Ear Hospital.Clinical characteristics of the anti-MOG cohort are seen in Table 1 and the anti-AQP4 cohort are seen in Table 2. The average length of the follow up was 16.5mo (range 2 to 41mo)and 47mo (range 2 to 131mo) for the MOG and AQP4 groups,respectively. Female to male ratio was 7:5 in the MOG group and 1:1 in the AQP4 group. Average age of onset in the MOG group was 29.2y with a range of 10 to 61y, while in the AQP4 group the average age was 42y (range 18-55y). Presenting complaint was blurring of vision in 10 of 12 of the MOG group (83.33%). The remaining 2 patients had pain as their presenting symptom (16.67%). In the AQP4 group, 3 out of the 4 patients (75%) experienced a decrease in vision while the remaining one patient had horizontal diplopia. Pain was a feature of all but one of the anti-MOG cohort (91.67%), either retrobulbar (27.27%) or more commonly on eye movement(72.73%). Interestingly, all the patients in the AQP4 cohort(100%) reported an absence of pain.
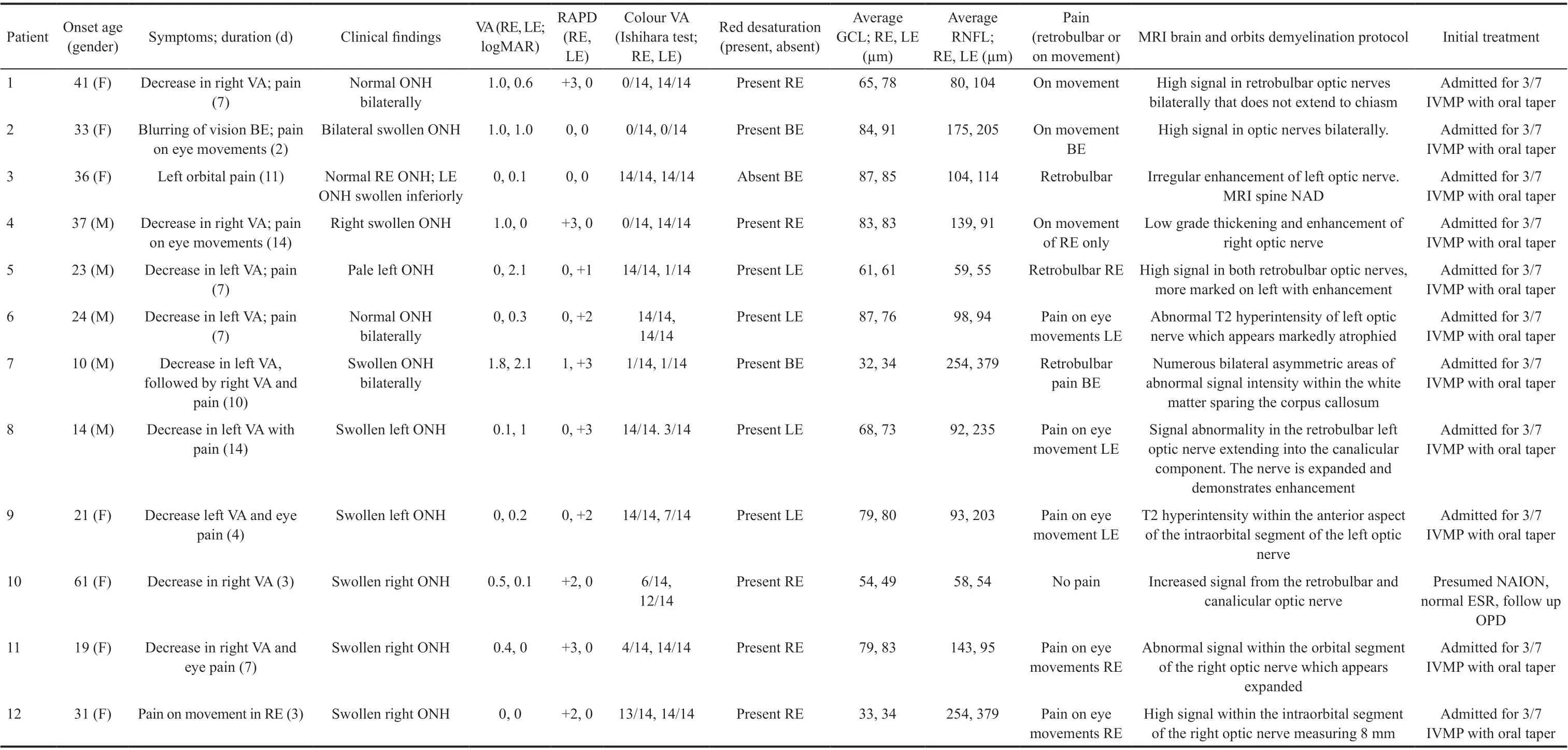
Ocular Findings With regards the affected eye in the MOG group, 5 were right eyes, 5 were left eyes and 2 of the patients had bilateral involvement giving us a total of 14 eyes available for analysis. There were 6 affected eyes in the AQP4 group comprising of 2 left eyes and 2 bilateral. The 11 of 14(78.57%) eyes in the MOG group had visible swollen optic nerve heads (ONH), 2 (14.29%) had normal appearing ONH and the remaining 1 (7.14%) had a pale ONH on presentation.In the AQP4 group, 3 out of the 6 (50%) eyes had either normal or pale appearing ONH and none had a swollen ONH.The presence or absence of an RAPD was also assessed at presentation to the ophthalmic emergency department. Of the MOG group, 11 of the 14 eyes (78.57%) had a RAPD. The presence of an RAPD in the AQP4 group was less with only 2 of the 6 (33.33%) eyes displaying one. The presence of a colour vision defect was also assessed. This was categorised as mild, moderate, or severe as outlined in the methods section.Of the 14 eyes in the MOG cohort, 12 (85.71%) had a colour vision defect. Of these, 9 (75%) were severe, 2 (16.67%)were moderate and 1 (8.33%) was mild. In the AQP4 group,a colour deficiency was observed in 4 of the 6 eyes (66.67%),all 4 being severe in nature. The presence of red desaturation was also assessed in a binary fashion. It was present in all but one eye in the MOG group (92.86%). Only 5 eyes in the AQP4 group were examinable as one eye was NPL, and 3 of the 5 eyes (60%) had this subjective finding.
Visual Acuity and Optical Coherence Tomography Findings Tables 3 and 4 outline initial and final VA in logMAR units, initial and final average GCL and RNFL thickness and the respective change in each for both groups.Only the records for the involved eye were taken for analysis and if both eyes were affected then the data for the more affected eye was utilised. The average presenting logMAR VA in the MOG group was 0.82 (range 0-2.1) while in the AQP4 group it was 1.475 (range 0-3). At last review, the average improvement in VA in the MOG group was -0.66 (range -2.1 to +0.1) and in the AQP4 group was -0.05 (range -0.3 to +0.1).With regards GCL analysis (Figure 1), a modest decrease in thickness was seen in both groups with an average reduction of 2.92 and 7.75 μm in the MOG and AQP4 respectively. The retinal nerve fibre thickness analysis (Figure 2) displayed a greater reduction in thickness, especially in the MOG cohort with an average reduction of 58.75 μm in this group as opposed to only 10.5 μm in the AQP4 group. We examined the correlation between GCL thickness and VA at presentation and as a determinant of final visual outcome in the MOG group. There was no statistically significant correlation(Pearson correlation) between GCL thickness and presenting and final VA [
(10)=0.081,
=0.08 and
(10)=0.089,
=0.34respectively]. The same statistical analysis was performed for the correlation between RNFL and VA and similar outcomes were observed [
(10)=0.04,
=0.22 and
(10)=0.09,
=0.04].In the AQP4 group, moderate correlation was observed between GCL thickness and presenting VA [
(2)=0.61,
=0.42], but this result was not statistically significant. No correlation was seen for initial RNFL thickness and final visual outcome in this group either [
(2)=0.19,
=0.38].



本文首先采用毫秒激光進行打孔實驗,利用高速攝影術捕捉打孔過程,得到氣化和熔融物的產生及熔融的噴濺情況,研究熔融物的噴濺軌跡和速率。然后依據實驗建立模型,利用數值模擬技術模擬研究激光打孔過程熔融物的噴濺情況。最后將兩者結果進行比較,證明數值模型的正確性,得到噴濺過程的基本規律。
Visual Acuity and Optical Coherence Tomography Findings Reduction in VA is a hallmark feature in optic nerve disease and the main reason why these patients attend the ophthalmic emergency department as their primary referral source. 81.25%of all eyes (13/16) had a reduction in their VA at presentation.The average presenting logMAR VA in the MOG group was 0.82 as opposed to the AQP4 group whose average VA was 0.655 units worse at 1.475. The average VA in the AQP4 group is compounded by the fact that 1 patient (25%) had a perfect presenting VA of 0 logMAR units. Interestingly, even though the AQP4 group had the greater scope for improvement in vision, it was the MOG group that achieved this (improvement of 0.66 units for the MOG group as opposed to just 0.05 units for the AQP4). If we define long term visual disability as 0.3 logMAR or greater (threshold for driving), all but one of the eyes in the MOG group achieved this (92.86%) as opposed to just 1 eye (25%) in the AQP4 group. These findings are in keeping with what is in the literature where anti-AQP4 positive patients tend to have more severe visual disability
.



Treatment and Maintenance Therapy All patients were treated as inpatients for 3 to 5d of 500 mg twice daily dosing of intravenous methylprednisolone at presentation. Current immunosuppressant therapy, if any, is outlined in Table 6. In the MOG group, azathioprine was the maintenance medication of choice with 5 of the 12 (41.67%) patients receiving it.Two patients were on methotrexate (16.67%), 1 was taking mycophenolate mofetil (8.33%) and 3 of the remaining 4(33.33%; 1 of which was pregnant) were on no maintenance therapy. The final patient was placed on rituximab, underwent plasma exchange and intravenous immunoglobulins (IVIG)and maintenance low dose steroid. In the AQP4 group, two of the patients (50%) were on low dose prednisolone and of the other two, one was taking azathioprine and the other methotrexate to control disease relapse.
As the name of the disease suggest, NMO is defined by both a myelitis and an ON
. The disease has a predilection for both the optic nerves and the spinal cord, and the lesions commonly spare the brain in the early stages
. Patients who have an ON associated with NMO tend to have an acute profound vision loss associated with disc swelling
. However, they may also develop optic nerve atrophy and cavitation akin to glaucomatous optic nerve change in severe cases
. The cavitation is postulated to be secondary to a demyelination associated necrosis of the optic nerve head. The episodes of ON may be recurrent and simultaneously bilateral
causing progressive optic atrophy with cumulative inflammatory damage.



DISCUSSION
Antibody positive optic neuropathies are uncommon. The limited number of seropositive patients available for analysis in our quaternary centre cohort is indicative of this. The female predominance usually seen with these diseases was evident in our sample with an overall female to male ratio of 9:7.
Radiological Findings All but one of the patients in the anti-MOG cohort had sparing of brain involvement (91.67%).All had optic nerve abnormalities observed on MRI imaging(Figure 4). Two (16.67%) of the patients had enhancement in the affected nerve and in the contralateral clinically unaffected nerve. In the AQP4 group, 2 (50%) of the patients had optic nerve enhancement on MRI, one had no evidence of optic neuritis and the final patient had evidence of chiasmitis (Figure 5;Signal abnormality on T2 weighted imaging and uptake with gadolinium).
膠……
 International Journal of Ophthalmology
2022年7期
International Journal of Ophthalmology
2022年7期
- International Journal of Ophthalmology的其它文章
- Relative peripheral refraction and its role in myopia onset in teenage students
- Incidence and risk factors for vitreous loss in residents performing manual small-incision cataract surgery
- Comparison of minimally invasive glaucoma surgery with trabecular micro-bypass stent and microhook ab interno trabeculotomy performed in conjunction with cataract surgery
- A new bleb-independent surgery namely penetrating canaloplasty for corticosteroid-induced glaucoma: a prospective case series
- Dynamic changes of inducible nitric oxide synthase expression in rat’s retina and its role on blood-retinal barrier injury after acute high intraocular pressure
- Characteristic of red eye related diseases of Han and Uygur population in Urumchi compared with Shanghai,China
