多囊卵巢綜合征患者血清炎癥因子及性激素水平的變化及二甲地黃湯的作用
林群 徐麗霞 陳青華 石明晴

[摘要] 目的 探討多囊卵巢綜合征(PCOS)患者血清炎癥因子及性激素水平的變化及二甲地黃湯的作用。方法? 選取2018年1月~2020年6月浙江省麗水市中醫(yī)院婦產(chǎn)科門(mén)診治療的PCOS患者40例作為試驗(yàn)組。試驗(yàn)組患者予以二甲地黃湯治療,1劑/d,連用3個(gè)月經(jīng)周期。觀察試驗(yàn)組治療前后血清炎癥因子[超敏C反應(yīng)蛋白(hs-CRP)和腫瘤壞死因子-α(TNF-α)]及性激素[促卵泡生成素(FSH)、雌激素(E2)和促黃體生成素(LH)]水平的變化。另選擇同期筆者醫(yī)院體檢中心的健康體檢者30例作為對(duì)照組,對(duì)照組僅在納入時(shí)測(cè)定血清hs-CRP、TNF-α、LH、FSH和E2水平。 結(jié)果? 試驗(yàn)組血清hs-CRP和TNF-α水平顯著高于對(duì)照組,差異有統(tǒng)計(jì)學(xué)意義(P<0.01);試驗(yàn)組血清LH水平明顯高于對(duì)照組,血清FSH和E2水平明顯低于對(duì)照組,差異有統(tǒng)計(jì)學(xué)意義(P<0.05)。治療3個(gè)月經(jīng)周期后,試驗(yàn)組血清hs-CRP和TNF-α水平較治療前明顯下降,差異有統(tǒng)計(jì)學(xué)意義(P<0.01);試驗(yàn)組血清LH水平較前明顯下降,血清FSH和E2水平較前明顯上升,差異有統(tǒng)計(jì)學(xué)意義(P<0.05)。 結(jié)論 PCOS患者存在血清炎癥因子水平異常和性激素紊亂。二甲地黃湯治療PCOS患者不僅可降低血清炎癥因子水平,控制炎癥反應(yīng),而且可糾正內(nèi)分泌紊亂,調(diào)節(jié)性激素水平。
[關(guān)鍵詞] 多囊卵巢綜合征;炎癥因子;性激素;二甲地黃湯
[中圖分類號(hào)] R711.7? ? ? ? ? [文獻(xiàn)標(biāo)識(shí)碼] B? ? ? ? ? [文章編號(hào)] 1673-9701(2022)16-0124-04
Changes of serum inflammatory factors and sex hormones in patients with polycystic ovary syndrome and the effect of dijiadihuang decoction
LIN Qun1 XU Lixia1 CHEN Qinghua1 SHI Mingqing2
1. Department of Laboratory, Lishui Hospital of Traditional Chinese Medicine in Zhejiang Province,Lishui 323000,China;2.Department of Obstetrics and Gynecology, Lishui Hospital of Traditional Chinese Medicine in Zhejiang Province,Lishui 323000,China
[Abstract] Objective To explore the changes of serum inflammatory factors and sex hormone levels in patients with polycystic ovary syndrome(PCOS) and the effect of Dijiadihuang Decoction. Methods A total of 40 PCOS patients treated in the Obstetrics and Gynecology Department of Lishui Traditional Chinese Medicine Hospital from January 2018 to June 2020 were selected as the experimental group. The patients in experimental group were treated with Erjiadihuang Decoction, 1 dose/d, for 3 consecutive menstrual cycles. The changes of serum inflammatory factors [hypersensitive C-reactive protein (hs-CRP) and tumor necrosis factor-α (TNF-α)] and sex hormones [follicle stimulating hormone (FSH), estrogen (E2) and luteinizing hormone [LH] in experimental group before and after treatment] levels. In the same period, 30 healthy subjects from the physical examination center of our hospital were selected as the control group, the serum hs-CRP, TNF-α, LH, FSH and E2 levels were examined including in the study. Results The serum hs-CRP and TNF-α levels of patients in experimental group were significantly higher than those in control group, and the difference was statistically significant between two groups(P<0.01);the serum LH level of patients in experimental group was significantly higher than that in control group, and the serum FSH and E2 levels of patients in were significantly lower than that in control group, the difference was statistically significant between two groups(P<0.05). After treatment for 3 menstrual cycles, the levels of serum hs-CRP and TNF-α in experimental group were significantly lower than before treatment, the difference was statistically significant before and after treatment(P<0.01); the levels of serum LH in experimental group were significantly lower than before, and the levels of serum FSH and E2 were significantly higher than before, and the difference was statistically significant before and after treatment(P<0.05).? Conslusion? Patients with PCOS have abnormal levels of serum inflammatory factors and disorders of sex hormones. Erjiadihuang Decoction in the treatment of PCOS patients can not only reduce the level of serum inflammatory factors and control the inflammatory response, but also correct endocrine disorders and regulate the level of sex hormones.
[Key words] Polycystic ovary syndrome; Inflammatory factors; Sex hormones; Dimethyl Dihuang Decoction
多囊卵巢綜合征(polycystic ovarian syndrome,PCOS)是婦產(chǎn)科常見(jiàn)病,育齡婦女多發(fā),發(fā)病率占育齡婦女的6%~13%,主要表現(xiàn)為內(nèi)分泌和代謝功能異常,可引起高雄激素血癥、月經(jīng)紊亂,導(dǎo)致不孕[1,2]。PCOS的發(fā)病機(jī)制至今國(guó)內(nèi)外尚未研究清楚,近年來(lái)研究發(fā)現(xiàn)慢性炎癥反應(yīng)及性激素紊亂引起的胰島素抵抗在PCOS發(fā)病中起著極其重要的作用[3,4]。近年來(lái)研究發(fā)現(xiàn)中醫(yī)中藥在PCOS的治療上發(fā)現(xiàn)具有獨(dú)特之處,可通過(guò)改善內(nèi)分泌紊亂,促進(jìn)卵泡發(fā)育,治療PCOS效果較好,但有關(guān)中醫(yī)中藥對(duì)PCOS患者血清炎癥因子及性激素水平的影響國(guó)內(nèi)外報(bào)道較少[5,6]。本研究分析PCOS患者血清炎癥因子及性激素水平的變化及二甲地黃湯的干預(yù)作用,現(xiàn)報(bào)道如下。
1 資料與方法
1.1 一般資料
選取2018年1月~2020年6月浙江省麗水市中醫(yī)院婦產(chǎn)科門(mén)診治療的PCOS患者40例作為試驗(yàn)組。納入標(biāo)準(zhǔn)[7]:①符合2012年制定的PCOS的診斷標(biāo)準(zhǔn)[8];②育齡婦女。排除標(biāo)準(zhǔn)[9]:①合并其他原因引起不孕者;②合并其他生殖系統(tǒng)疾病者。試驗(yàn)組年齡21~40歲,平均(28.81±4.36)歲;體重41~82 kg,平均(51.22±4.81)kg。另選擇同期浙江省麗水市中醫(yī)院體檢中心的健康體檢者30例作為對(duì)照組,年齡23~38歲,平均(28.45±4.51)歲;體重42~80 kg,平均(51.92±3.78)kg。兩組年齡和體重等比較,差異無(wú)統(tǒng)計(jì)學(xué)意義(P>0.05),具有可比性。本方案通過(guò)筆者醫(yī)院醫(yī)學(xué)倫理委員會(huì)批準(zhǔn),納入患者均簽署知情同意書(shū)。
1.2 方法
試驗(yàn)組予以二甲地黃湯治療,藥物組成:炙龜版和炙鱉甲各20 g,生地黃、山藥、山茱萸、麥冬、茯苓、丹皮和蓮子心各6 g,1劑/d,水煎取汁約200 ml分早晚2次口服,連用3個(gè)月經(jīng)周期。觀察試驗(yàn)組治療前后血清炎癥因子[超敏C-反應(yīng)蛋白(hypersensitive3 C-reactive protein, hs-CRP)和腫瘤壞死因子-α(tumor necrosis factor-α, TNF-α)]及性激素[促卵泡生成素(follicular hormone,F(xiàn)SH)、雌激素(estrogen 2,E2)和促黃體生成素(luteinizing hormone,LH)]水平的變化,對(duì)照組僅在納入時(shí)測(cè)定血清指標(biāo)1次。
1.3 觀察指標(biāo)
1.3.1 標(biāo)本采集? 抽取空腹靜脈血3~5 ml,3000 r/min離心10 min分離出血清,置于-70℃的冰箱內(nèi)保存。
1.3.2 血清炎癥因子及性激素水平測(cè)定? 采用乳膠增強(qiáng)免疫散射比濁法測(cè)定血清hs-CRP水平,試劑盒由深圳邁瑞生物醫(yī)療電子有限公司提供;采用酶聯(lián)免疫吸附法測(cè)定血清TNF-α水平,試劑盒由北京中杉金橋生物技術(shù)有限公司提供;采用電化學(xué)發(fā)光測(cè)定血清FSH、E2和LH水平,試劑盒由羅氏診斷產(chǎn)品有限公司提供。
1.4 統(tǒng)計(jì)學(xué)方法
采用SPSS 22.0統(tǒng)計(jì)學(xué)軟件進(jìn)行數(shù)據(jù)分析,計(jì)量資料以均數(shù)±標(biāo)準(zhǔn)差(x±s)表示,采用t檢驗(yàn)。計(jì)數(shù)資料以[n(%)]表示,采用χ2檢驗(yàn),P<0.05為差異有統(tǒng)計(jì)學(xué)意義。
2 結(jié)果
2.1 兩組治療前后血清炎癥因子水平比較
試驗(yàn)組血清hs-CRP和TNF-α水平顯著高于對(duì)照組(P<0.01),治療3個(gè)月經(jīng)周期后,試驗(yàn)組血清hs-CRP和TNF-α水平較治療前明顯下降(P<0.01)。見(jiàn)表1。
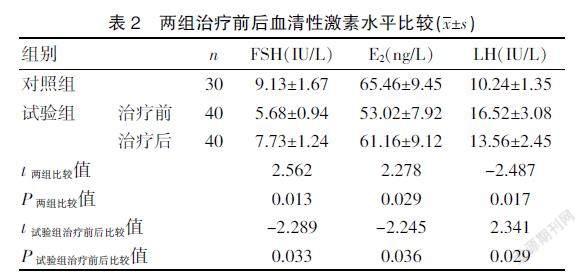
2.2 兩組治療前后血清性激素水平比較
試驗(yàn)組血清LH水平明顯高于對(duì)照組,血清FSH和E2水平明顯低于對(duì)照組(P<0.05);治療3個(gè)月經(jīng)周期后,試驗(yàn)組血清LH水平較前明顯下降,血清FSH和E2水平較前明顯上升(P<0.05)。見(jiàn)表2。
3 討論
PCOS是臨床常見(jiàn)的內(nèi)分泌和代謝紊亂的綜合征,以育齡期女性多見(jiàn),患者出現(xiàn)內(nèi)分泌紊亂和代謝異常的情況,臨床表現(xiàn)為卵泡發(fā)育異常和排卵功能喪失,患者體內(nèi)的雄性激素異常升高,出現(xiàn)月經(jīng)失調(diào)紊亂、閉經(jīng)和不孕等情況,對(duì)患者的生活質(zhì)量影響較大[10]。隨著社會(huì)環(huán)境的不斷變化,PCOS的發(fā)病率近年來(lái)有逐年上升的趨勢(shì),導(dǎo)致育齡期婦女月經(jīng)紊亂和不孕,不僅影響患者身心健康,而且給其家庭、社會(huì)和婚姻等帶來(lái)極大的傷害,需積極干預(yù)治療[11]。
PCOS的病理機(jī)制較復(fù)雜,其中炎癥反應(yīng)異常及下丘腦-垂體-卵巢軸功能紊亂障礙是其主要影響因素[12,13]。研究發(fā)現(xiàn)PCOS患者存在慢性亞臨床炎癥反應(yīng)狀態(tài),炎癥可能導(dǎo)致下丘腦-垂體-性腺軸功能發(fā)生障礙及卵泡發(fā)育異常的整個(gè)過(guò)程,分泌多種炎癥相關(guān)細(xì)胞因子及免疫調(diào)節(jié)分子,參與調(diào)節(jié)卵巢多種功能,如卵泡形成、排卵及黃體形成及撤退過(guò)程[14~16]。本研究顯示,試驗(yàn)組血清hs-CRP和TNF-α水平顯著高于對(duì)照組。提示PCOS患者存在血清炎癥因子水平異常升高,體內(nèi)存在慢性亞臨床炎癥反應(yīng)狀態(tài)。研究亦發(fā)現(xiàn)PCOS患者存在下丘腦-垂體-卵巢軸功能紊亂,使得下丘腦促性腺激素釋放激素分泌脈沖頻率增加,增加垂體對(duì)促性腺激素釋放激素的敏感度,使垂體分泌LH的頻率及幅度增加,LH分泌增加會(huì)降低FSH和E2的合成和分泌[17~19]。本研究發(fā)現(xiàn)血清LH水平明顯高于對(duì)照組,血清FSH和E2水平明顯低于對(duì)照組,提示PCOS患者存在血清性激素紊亂,表現(xiàn)為血清LH水平明顯上升,血清FSH和E2水平明顯下降。
PCOS是一個(gè)影響內(nèi)分泌、代謝、生殖、性腺等多系統(tǒng)的復(fù)雜疾病,中醫(yī)學(xué)上無(wú)此病名,結(jié)合臨床實(shí)踐認(rèn)為其主要病理病機(jī)多為腎氣不足、沖任失資、臟腑功能失常,中醫(yī)對(duì)本病的治療是站在整體調(diào)理的高度,以腎虛為立足點(diǎn),兼健脾化痰、祛濕理氣、化瘀等[20~22]。二甲地黃湯方中炙龜版、炙鱉甲滋陰潛陽(yáng)散結(jié),生地黃壯水滋陰;山藥補(bǔ)腎健脾;山茱萸補(bǔ)益肝腎,益精潛陽(yáng);茯苓益氣健脾利水;丹皮清熱涼血;麥冬清心潤(rùn)肺;蓮子心清心安神。本研究顯示,治療3個(gè)月經(jīng)周期后,試驗(yàn)組患者血清hs-CRP和TNF-α水平較前明顯下降,且試驗(yàn)組血清LH水平較前明顯下降,血清FSH和E2水平較前明顯上升。提示二甲地黃湯治療PCOS患者不僅可降低血清炎癥因子水平,控制炎癥反應(yīng),而且可糾正內(nèi)分泌紊亂,調(diào)節(jié)性激素水平。
綜上所述,PCOS患者存在血清炎癥因子水平異常和性激素紊亂。二甲地黃湯治療PCOS患者不僅可降低血清炎癥因子水平,控制炎癥反應(yīng),而且可糾正內(nèi)分泌紊亂,調(diào)節(jié)性激素水平。
[參考文獻(xiàn)]
[1]? ?Korkmazg GG,Altinoglu E,Civelek S,et al. The association of oxidative stress markers with conventional risk factors in the metabolic syndrome[J].Metabolism,2018,62(6):828-835.
[2]? ?Huang G, Coviello A. Clinical update on screening diagnosis and management of metabolic disorders and cardiovascular risk factors associated with polycystic ovary syndrome[J].Curr Opin Endocrinol Diabetes Obes,2018,19(6):512-519.
[3]? ?Cutler DA,Pride SM,Cheung AP. Low intakes of dietary fiber and magnesium are associated with insulin resistance and hyperandrogenism in polycystic ovary syndrome: A cohort study[J].Food Sci Nutr,2019,7(4):1426-1437.
[4]? ?黨菲. 控制胰島素抵抗改善多囊卵巢綜合征患者性激素與血脂代謝的效果[J].中國(guó)婦幼保健,2018,33(19):4388-4392.
[5]? ?李蔚,郝霞,丁慧. 影響多囊卵巢綜合征不孕癥患者受孕結(jié)局的中醫(yī)體質(zhì)、中醫(yī)證候相關(guān)因素分析[J].中華中醫(yī)藥學(xué)刊,2020,31(5):248-251.
[6]? ?楊藝嬌,楊玲,倪曉容. 多囊卵巢綜合征中醫(yī)證型與體質(zhì)分布及血清炎癥因子的相關(guān)性研究[J].河北中醫(yī),2020, 42(10):1465-1470.
[7]? ?Ozelci R, Dilbaz S, Dilbaz B, et al. Gonadotropin releasing hormone antagonist use in controlled ovarian stimulation and intrauterine insemination cycles in women with polycystic ovary syndrome[J].Taiwan J Obstet Gynecol,2019, 58(2):234-238.
[8]? ?中華醫(yī)學(xué)會(huì)婦產(chǎn)科學(xué)分會(huì)內(nèi)分泌學(xué)組及指南專家組. 多囊卵巢綜合征中國(guó)診療指南[J].中華婦產(chǎn)科雜志,2018,53(1): 2-6.
[9]? ?Patel R,Shah G. Evaluation of ovarian and metabolic effects of GnRH modulators in two rat models of polycystic ovary syndrome[J].Mol Reprod Dev,2018,85(10):778-789.
[10]? Kalhori Z,Mehranjani MS,Azadbakht M,et al. L-Carnitine im-proves endocrine function and folliculogenesis by reducing inflammation,polycystic ovaryoxidative stress and apoptosis in mice following induction of syndrome[J].Reprod Fertil Dev,2019,31(2):282-293.
[11]? Escobar-Morreale HF, Luque-Ram rez M, Gonz lez F. Circulating inflammatory markers in polycystic ovary syndrome: A systematic review and metaanalysis[J].Fertil Steril,2011,95(3): 1048-1058.
[12]? 談美華,章麗盈.多囊卵巢綜合征所致不孕患者性激素及代謝指標(biāo)檢測(cè)分析[J].中國(guó)婦幼保健,2020,35(2):302-304.
[13]? Deepika ML,Reddy KR,Yashwanth A,et al. TNF -α haplotype association with polycystic ovary syndrome-a South Indian study[J].J Assist Reprod Genet,2018,30(11):1493-1503.
[14]? 劉震忠.雷洛昔芬聯(lián)合坤泰膠囊治療對(duì)多囊卵巢綜合征不孕婦女性激素水平及妊娠結(jié)局的影響[J].中國(guó)婦幼保健,2018,33(12):2774-2777.
[15]? Yilmaz N,Inal HA,Gorkem U,et al. Follicular fluid total antioxidant capacity levels in PCOS[J].J Obstet Gynaecol,2016,36(5): 654-655.
[16]? 師帥,劉鴻.達(dá)英-35與優(yōu)思明對(duì)肥胖型多囊卵巢綜合征患者脂代謝 性激素水平及妊娠結(jié)局的影響[J].中國(guó)婦幼保健,2018,33(10):2217-2221.
[17]? Kim CH, Ahn JW, You RM, et al. Pioglitazone treatment decreases follicular fluid levels of tumor necrosis factor-αand interleukin-6 inpatients with polycystic ovary syndrome[J].Clin Exp Reprod Med,2011,38(2):98-102.
[18]? 陳瓊娣.多囊卵巢綜合征患者血清AMH與性激素水平的相關(guān)性研究[J].云南醫(yī)藥,2021,42(1):47-48.
[19]? Sakumoto R,Vermehren M,Kenngott RA,et al. Localization of gene and protein expressions of tumor necrosis factor-{alpha} and tumor necrosis factor receptor types I and II in the bovine corpus luteum during the estrous cycle[J].J Anim Sci,2011,89(10):3040-3047.
[20]? 周貴鳳,林色奇.從多囊卵巢綜合征的古代病名探究中醫(yī)病因病機(jī)[J].江西中醫(yī)藥大學(xué)學(xué)報(bào),2021,33(1):5-7.
[21]? 馮玉,高月平.江蘇地區(qū)多囊卵巢綜合征中醫(yī)證型分布規(guī)律及與飲食失宜相關(guān)性的臨床研究[J].中國(guó)中藥雜志,2014,39(10):1937-1940.
[22]? 吳緒祥.中藥聯(lián)合克羅米芬治療多囊卵巢綜合征不孕癥臨床觀察[J].湖北中醫(yī)學(xué)院學(xué)報(bào),2010,12(2):15-16.
(收稿日期:2021-03-19)
- 中國(guó)現(xiàn)代醫(yī)生的其它文章
- 混合痔治療現(xiàn)狀分析
- 環(huán)狀RNA在骨關(guān)節(jié)炎調(diào)控的研究進(jìn)展
- 食管癌根治術(shù)后出院患者營(yíng)養(yǎng)延續(xù)性護(hù)理的現(xiàn)況與建議
- 止咳平喘十二味合劑治療痰熱郁肺型咳嗽變異性哮喘的臨床療效評(píng)價(jià)及作用機(jī)制研究
- 玉屏風(fēng)加減聯(lián)合西藥治療過(guò)敏性結(jié)膜炎的療效及安全性meta分析
- 中西醫(yī)結(jié)合多模式止痛方案改善肩關(guān)節(jié)鏡術(shù)后腫脹、疼痛的有效性分析

