Effectiveness and postoperative rehabilitation of one-stage combined anterior-posterior surgery for severe thoracolumbar fractures with spinal cord injury
lNTRODUCTlON
因此,產(chǎn)生了由物流服務(wù)集成商、物流服務(wù)提供商構(gòu)成的兩級物流服務(wù)供應(yīng)鏈,用于滿足零售商面向客戶的個性化、多樣化的物流服務(wù)需求。由此形成了兩級產(chǎn)品供應(yīng)鏈與兩級物流服務(wù)供應(yīng)鏈的聯(lián)動與融合,本文將重點研究兩者聯(lián)動的利益協(xié)調(diào)問題。
Thoracolumbar fractures refer to fractures at the thoracolumbar spine, which are mainly featured by local thoracic spinal pain and swelling and muscle tension on both sides of the fracture. Patients with thoracolumbar fractures may have difficulty in standing and turning over. Some may even suffer from movement disorder and significant impairment of daily life activities. The incidence of thoracolumbar fractures is relatively high, and is a common trauma at the Department of Orthopedics. The diagnosis of this disorder has become easier and faster in China due to the continuous improvement in medical technology[1,2]. Thoracolumbar fractures are generally combined with spinal cord injury to varying degrees, which may cause deterioration of the patients' condition and increase the difficulty of clinical treatment. The reasons for this are as follows: The fractured blocks and the intervertebral disc tissues protrude into the spinal canal, resulting in spinal cord contusion and compression. Therefore, fracture reduction, spinal compression, and spinal fixation and fusion at the affected segments are crucial steps in surgery[3]. China has witnessed a rapid development of medical science in recent years, and the diagnosis of thoracolumbar fractures is more rapid, while the selection of an appropriate treatment has become a primary concern[4]. At present, anterior or combined anterior-posterior surgery is preferred for severe thoracolumbar fractures. In this study, the application value, advantages, and disadvantages of these two surgical approaches were compared by reviewing the data of patients with thoracolumbar fractures treated at our hospital.
MATERlALS AND METHODS
Patients
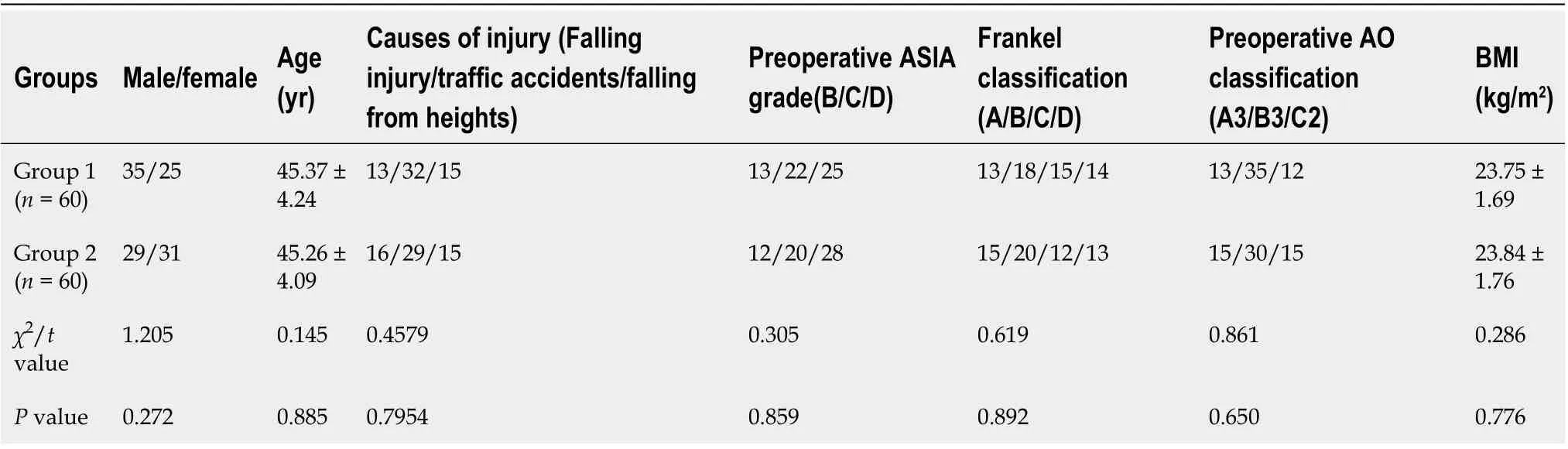
The present study was approved by the hospital ethics committee. One hundred and twenty patients with severe thoracolumbar fractures and spinal cord injury treated at our hospital from February 2020 to February 2021 were randomly enrolled. The random sampling method was used to divide the patients into two groups, namely, group 1 and group 2, with 60 patients in each group. Informed consent was obtained from all patients. The two groups were not different significantly in terms of the basic information (> 0.05) (Table 1).
周橋似乎意識到了作為管理者的不足,他去書店買了一大堆關(guān)于管理和人際關(guān)系的書籍,有些放在辦公室,有些放在床頭,閑來就看看。
One-stage combined anterior-posterior surgery can effectively improve the function of affected vertebrae and the life quality of patients with severe thoracolumbar fractures and spinal cord injury.This surgical approach is worthy of promotion in clinical use.
(1) Cognitive impairment to varying degrees; (2) recent history of acute and chronic infections; (3) hearing impairment or incapable of communication; (4) pathological fractures caused by tumors, infections, or osteoporosis; (5) severe spinal degenerative diseases; and (6) history of drug dependence or drug allergy.
Methods
Patients in group 2 received anterior decompression plus bone grafting with internal fixation. General anesthesia was performed in the lateral position. A lateral-anterior extra-pleuroperitoneal approach was adopted to expose the affected vertebrae and the adjacent vertebrae. The ribs were resected selectively to prepare the bone graft. The lateral portion of the pedicle of the affected vertebral body was resected to expose the dural sac and nerve root sleeve fully. The posterior 3/4 portion of the vertebral body was resected, along with the superior and inferior intervertebral discs and the endplate cartilage.Decompression was performed to the medial margin of the contralateral pedicle. Extra care was taken not to injure the spinal cord. Further inspection was conducted to confirm that the compression was completely removed and the deformity was corrected. Next, an autologous tricortical iliac bone graft of an appropriate length was inserted between the superior and inferior vertebral bodies. The titanium plate was mounted and immobilized. The residual fractured blocks were placed into the iliac bone and the lateral gaps. Thorough hemostasis was performed, followed by washing with normal saline. The incision was sutured layer by layer.
本項目2014年11月底進場,1號交通洞作為地下泵站及其附屬洞室群的主要施工通道,其施工進度直接影響到地下泵站及其附屬洞室的施工進度。此時不是遷墳時節(jié),由于遷墳、征地、移動果林附著的3路線纜等地面附著物較為困難,在增加大量投資的同時也需要耗費大量的時間,短期內(nèi)1號交通洞無法施工,對此將1號交通洞進口段由設(shè)計的明挖改為洞挖施工。
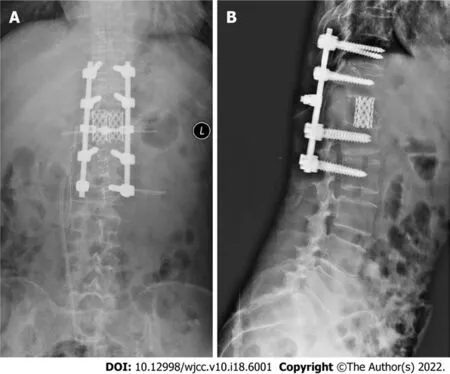
Patients in group 1 received surgerythe combined anterior-posterior approach: The same steps were followed for anterior decompression as in group 2. The incision was maintained at a length of 10-12 cm as no anterior fixation would be performed. Grafting with large iliac bone blocks was performed for the fusion. If the harvested iliac bone blocks were thin, the fusion was performed using a titanium mesh cage. Posterior fixation was performedthe intermuscular space. Therefore, no damage would be caused to the posterior complex structure (Figure 1). The GSS-Ⅱ rod-screw system and Depuy pedicle screw system were used. It was unnecessary to perform canal decompression. Lateral fenestration of the vertebral body was performed if the superior and inferior intervertebral discs of the affected vertebra were not damaged, which was followed by intravertebral bone grafting. A closed thoracic drainage tube was indwelled for all patients receiving thoracotomy. The drainage tube was removed after confirming that there was no effusion or pneumatosis in the thoracic cavity. Costal bone was introduced for patients who received fusion using large iliac bone blocks. The fractured blocks harvested by spinal decompression were regrafted.
The early interventions after surgery were the same in both groups. Patients with nerve injury were treated with hormones and mannitol 4-5 d after surgery and with antibiotics 5-7 d after surgery. Fluid replacement was given to maintain electrolyte and acid-base balance. The indication for blood transfusion was assessed based on intraoperative blood loss and postoperative routine blood tests.Patients with osteoporosis received anti-osteoporosis treatment within 1 mo after surgery, and only then were they allowed to get out of bed. The time to ambulation was prolonged to 1.5 mo after surgery for those with severe osteoporosis. In addition, these patients were required to wear waist braces within the first 3 mo of ambulation.
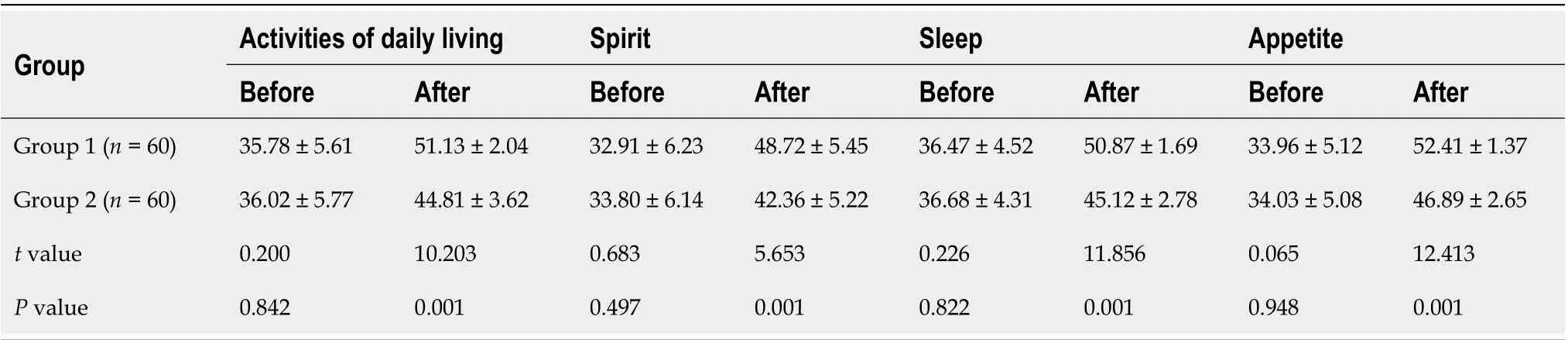
Blood loss was greater and the operation time was longer in group 1 than in group 2, with significant difference. Incision length, intraoperative X-rays, and length of hospital stay were not significantly different between the two groups. Preoperative function of the affected vertebrae was not significantly different between the two groups. In each group, the patients showed significant improvement after surgery. The anterior vertebral height ratio and the posterior vertebral height ratio in group 1 after surgery were significantly higher than those in group 2. The Cobb angle after surgery was significantly lower in group 1 than in group 2. The canal-occupying ratio of the affected vertebrae was not significantly different between the two groups. Before surgery, there was no significant difference in the quality of life scores between the two groups. The above indicators were significantly improved after surgery compared with before surgery in each group. In addition, these indicators were markedly better in group 1 than in group 2 after surgery.
Observation indicators
The observation indicators were blood loss, incision length, operation time, intraoperative X-rays, length of hospital stay, anterior vertebral height ratio, posterior vertebral height ratio, Cobb angle, and canaloccupying ratio of the affected vertebra.
Quality of life (QOL) was scored in the two groups before treatment and at 2 mo after surgery. The total score of each item ranged from 0 to 60: scores < 20, extremely poor; 20-50, fair; and 51-60, good[5].
Statistical analysis
其中,k值越小時,所計算出的距離越適合運用在高維空間中,并由此提出了分數(shù)距離度量,即利用k<1的距離來衡量高維空間中數(shù)據(jù)間的距離。當k=2時,式(7)代表歐氏距離。
RESULTS
Comparison of surgical indicators
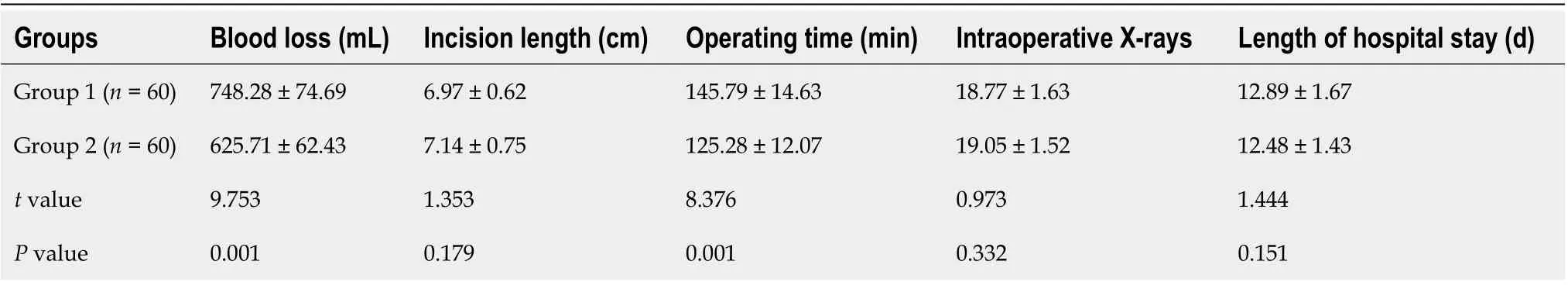
Blood loss was greater and the operation time was longer in group 1 than in group 2, with significant difference (< 0.05). Incision length, intraoperative X-rays, and length of hospital stay were not significantly different between the two groups (> 0.05) (Table 2).
Comparison of the function of the affected vertebrae
However, our study also has some limitations. First, this was a single-center study with limited number of patients enrolled, and the novel surgical approach is still expected to be attempted in more centers. Second, the follow-up was short in our study, and the long-term efficacy of the novel surgical approach remains to be further documented.
Comparison of the QOL scores between the two groups
Before surgery, there was no significant difference in the QOL scores between the two groups (> 0.05).The above indicators in each group were significantly improved after surgery compared with before surgery. In addition, these indicators were much better in group 1 than in group 2 after surgery (<0.05) (Table 4).
DlSCUSSlON
Severe spinal fractures caused by high-energy trauma have become increasingly common in recent years. Spinal fractures, damaged spine structure, spinal dislocation, and space occupation by a large number of fractured blocks in the spinal canal may cause spinal cord compression and nerve injury[6,7]. At present, the clinical treatment for such a disorder aims to achieve sufficient spinal decompression,restore the support and immobilize the vertebrae, and hence promote bone union and recovery of nerve function. However, the conventional posterior approach may fail to achieve these goals[8,9].
公路工程施工管理過程中的常見問題及解決措施分析……………………………………………… 李軍,汪常輝(7-230)
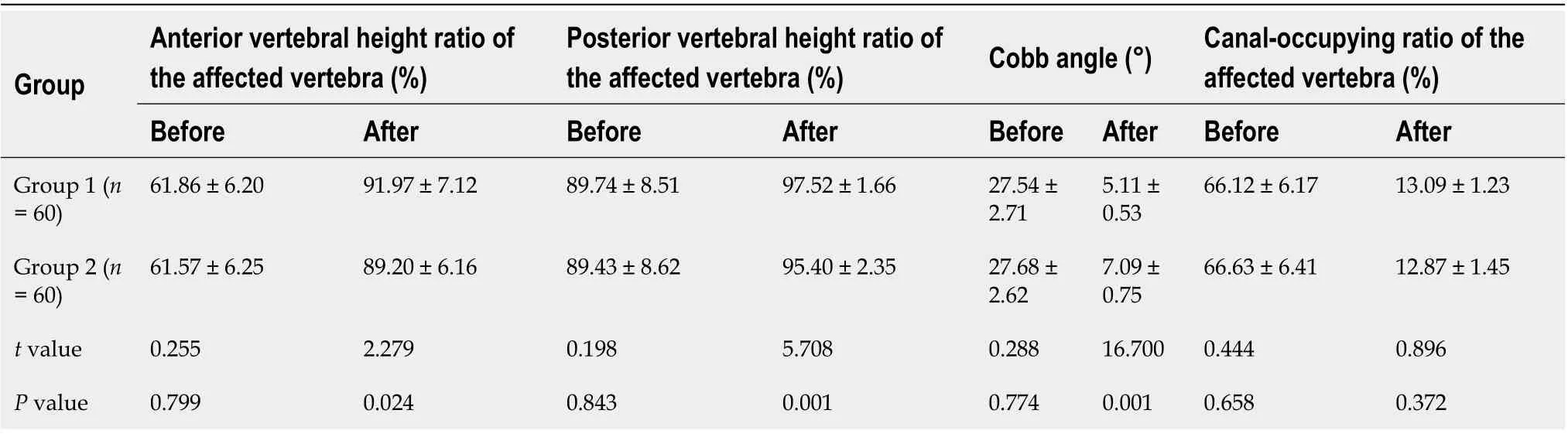
Surgical treatment for thoracolumbar fractures is usually intended to reconstruct the normal spinal structure and spinal stability, relieve compression, prevent late-stage thoracolumbar deformity and secondary nerve injury, and offer mechanical protection for recovery of nerve function[10,11]. Posterior spinal surgery is an invasive surgery, and the surgical indications of patients should be carefully assessed to prevent complications and ensure surgical success[12,13]. Given these facts, posterior open spinal surgery is generally intended to treat thoracolumbar fractures with spinal instability. Spinal instability is a disorder where the spine does not maintain normal anatomy when resisting loads. As a result, the nerve roots may have a secondary injury or mechanical injury, which further changes the spine structure and induces fracture malunion[14,15]. Certain rules should be followed during surgery,and the surgical approach is selected depending on the position of spinal compression. In addition, a pedicle screw-rod internal fixation system is used to improve surgical outcomes[16,17]. The present study showed that blood loss was greater and the operation time was longer in group 1 than in group 2(< 0.05). Incision length, intraoperative X-rays, and length of hospital stay were not significantly different between the two groups (> 0.05). In each group, the patients' condition was significantly improved after surgery compared with before surgery. The anterior vertebral height ratio and the posterior vertebral height ratio in group 1 after surgery were significantly higher than those in group 2.The Cobb angle after surgery was significantly lower in group 1 than in group 2 (< 0.05). However,the canal-occupying ratio of the affected vertebra was not significantly different between the two groups(> 0.05). Each group of patients achieved significant improvement after surgery. All of the relevant indicators in group 1 were significantly higher than those in group 2 after surgery (< 0.05). The reasons for these results might be due to the larger incision, greater blood loss, longer operation time,and difficulty in vertebral exposure. Anterior spinal surgery has the following advantages compared with the posterior approach: More thorough spinal decompression, lower risk of fixation loosening and disruption, removal of the fixation system after artificial joint fusion is unnecessary, and less likelihood of vertebral deformity, paralysis and sequelae after surgery[18,19]. The following defects have been reported for posterior spinal surgery: Degeneration and stenosis of the affected vertebrae and the superior adjacent intervertebral disc; multiple micromovements of the pedicle screws under excessive loading, which further causes loosening before bony fusion[20,21]; postoperative cutting of the screws within the cancellous bone, leading to reduction loss in those for whom osteoporosis is not confirmed before surgery; and fatigue fracture of the pedicle screws and implants due to overload[9]. Despite the above defects, posterior spinal surgery also has the following advantages. It is easier to perform surgerythis approach; only the superior and inferior adjacent segments of the affected vertebrae are immobilized with pedicle screws. In this way, the number of segments to be immobilized is reduced,while the motor function of the spine is preserved maximally[17]. This approach allows for posterior laminectomy with direct decompression. In addition, a well-designed implant enables sufficient stretching of the anterior and posterior longitudinal ligaments of the fibrous ring under the physiological curvature through three-dimensional adjustment. The implant can effectively achieve the reduction of fractured blocks in the vertebral canal in burst fractures through traction. Hence, indirect decompression is achieved without further damaging the stability of the bony structure[16]. The posterior approach not only allows bone grafting for fusion, but also fusion of the anterior affected bonethe pedicle. The combined anterior-posterior surgery integrates the advantages of both the anterior and posterior approaches. The combined approach can directly manage the displacement of a posterior column fracture and offer pre-support to assist in anterior reduction. The adjacent segments can be temporarily stabilized. In addition, the cage for anterior bone fusion can be conveniently placed by pressurizing and tightening. Moreover, excessive tilting or subsidence of the titanium mesh cage can be prevented. Therefore, the normal physiological loading state before the injury can be best reproduced[22]. Our study showed that the combined anterior-posterior surgery outperformed the posterior spinal surgery in promoting the functional recovery of the affected vertebrae and improved the patients’ QOL.The combined approach effectively restored the height of the affected vertebrae and corrected kyphosis.The combined approach also allows for sufficient anterior decompression, and the simple anterior approach does not enable temporary fixation, auxiliary reduction, and three-column fixation according to Denis' three-column concept. Therefore, the latter is usually associated with an unfavorable microenvironment for callus regeneration.
There were no significant differences in the preoperative function of the affected vertebrae between the two groups (> 0.05). Significant improvement was achieved in both groups after surgery. The anterior vertebral height ratio and the posterior vertebral height ratio in group 1 after surgery were significantly higher than those in group 2. The Cobb angle after surgery was significantly lower in group 1 than in group 2 (< 0.05). The canal-occupying ratio of the affected vertebrae was not significantly different between the two groups (> 0.05) (Table 3).
CONCLUSlON
(1) No conscious disturbance; (2) complete medical records; (3) thoracolumbar fractures confirmed by computed tomography (CT) or X-rays, combined with nerve injury; (4) fractured blocks occupying over 50% of the spinal canal; (5) patients tolerant to surgery; and (6) the degree of vertebral compression greater than 50%.
ARTlCLE HlGHLlGHTS
Research methods
One hundred and twenty patients with severe thoracolumbar fractures and spinal cord injury treated at our hospital from February 2020 to February 2021 were randomly enrolled, which were randomly divided into group 1 (one-stage combined anterior-posterior surgery) and group 2 (one-stage anteriorapproach surgery). Blood loss, incision length, operation time, intraoperative X-rays, length of hospital stay, anterior vertebral height ratio, posterior vertebral height ratio, Cobb angle, canal-occupying ratio of the affected vertebra, and quality of life scores were compared between the two groups.
由于干旱指數(shù)的周期變換很復雜,變化周期不固定,且在同一時段中又包含各種時間尺度的周期變化,表現(xiàn)出多時間尺度的特征,因此本文利用小波變換分析方法來研究干旱指數(shù)在不同尺度(周期)隨時間的演變情況。
Research results
矗立在湖畔一處山崖峭壁上的布萊德城堡,為湖景增添了許多夢幻色彩。這座中世紀的城堡是斯洛文尼亞最大、最古老的城堡之一。古典建筑和湖光山色和諧地融為一體,在季節(jié)和光影的變化中,默默地向世人展現(xiàn)著自己多姿多彩的風貌。
(一)梁廷燦《歷代名人生卒年表》謂金門詔“生于康熙十二年癸丑”。陶容、于士雄《歷代名人生卒年表補》則對梁表進一步補充,著錄生年一致,卒年則說據(jù)《光緒江都續(xù)志》“年八十卒”,著錄為“乾隆十六年辛未”(北京圖書館出版社2002年版,第504頁)。如果按“生于康熙十二年”而“年八十卒”推算,則金門詔卒年按虛歲當為乾隆十七年。另外,查核《光緒江都續(xù)志》并未載金門詔生卒年月,“年八十卒”不知何據(jù)。
Research conclusions
One-stage combined anterior-posterior surgery effectively improves the function of the affected vertebrae and the life quality of patients with severe thoracolumbar fractures and spinal cord injury.
All statistical analyses were performed using SPSS 22.0 software. Measurements were expressed as mean ± SD and analyzed by the-test. Counts were expressed as(%) and analyzed by thetest.<0.05 indicated a significant difference.
本文的主要貢獻在于將IMU固定在腳部,采用SVM分類器識別單步運動速度,當行人在1.5 m/s~4 m/s內(nèi)運動時,我們認為單步運動速度識別誤差將小于0.25 m/s。本文提出的方法存在一定的誤差。但是由于同一人員運動狀態(tài)改變時步長會發(fā)生顯著變化,且已證明運動速度與運動步長之間有強相關(guān)關(guān)系。本文提出的方法存在一定誤差,但是利用本文提出的方法,針對存在速度劇烈變化的運動過程,可以根據(jù)識別的單步運動狀態(tài)改變行人的運動步長,相對于用戶輸入步長固定值,將有助于提高SHSs的追蹤精度。
Research perspectives
One-stage combined anterior-posterior surgery is worthy of popularization in clinical use.
FOOTNOTES
Conceptualization: Zhang B contributed the conceptualization of the study; An Y, Wang JC,Song QP and Jiang YZ collected the data; An Y and Wang JC Formal analyzed the data; Wang JC, Song QP and Jiang YZ wrote the manuscript; Wang JC, Song QP and Zhang B reviewed and edited the manuscript.
The study was reviewed and approved by the Ethics Committee of Beijing Jishuitan Hospital (Approval No. 202110-05).
All study participants, or their legal guardian, provided informed written consent prior to study enrollment.
The authors declare that they have no conflicts of interest concerning this article. No benefits in any form have been or will be received from any commercial party related directly or indirectly to the subject of this study.
No additional data are available.
The authors have read the STROBE Statement - checklist of items, and the manuscript was prepared and revised according to the STROBE Statement - checklist of items.
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
China
Bo Zhang 0000-0002-6320-7258; Jin-Chao Wang 0000-0003-0423-750X; Yu-Zhen Jiang 0000-0003-2248-7211; Qing-Peng Song 0000-0002-2146-6913; Yan An 0000-0003-4919-2106.
袁安將吳耕抱在懷里,李離掐著他的人中穴,上官星雨將玉玦取下來,代替火把舉在手里。吳耕醒過來,張著嘴,蠕動著嘴唇,卻說不出話。看到三人著急的神色,他又伸手指向自己的雙耳。在鋪天蓋地的花雨里,在他想起跟父親一起重返他們的吳家垴桃花源之后,他到底想到了什么樣的幻象,讓他激動如斯,無法說,也無法聽?
Wang JL
A
Wang JL
 World Journal of Clinical Cases2022年18期
World Journal of Clinical Cases2022年18期
- World Journal of Clinical Cases的其它文章
- Stem cells as an option for the treatment of COVID-19
- Development of clustered regularly interspaced short palindromic repeats/CRISPR-associated technology for potential clinical applications
- Prostate sclerosing adenopathy: A clinicopathological and immunohistochemical study of twelve patients
- Construction and validation of a novel prediction system for detection of overall survival in lung cancer patients
- Identification of potential key molecules and signaling pathways for psoriasis based on weighted gene coexpression network analysis
- Coinfection of Streptococcus suis and Nocardia asiatica in the human central nervous system: A case report
