Etiology, pathogenesis, and diagnosis of neovascular glaucoma
INTRODUCTION
Neovascular glaucoma (NVG) is a potentially blinding,intractable and aggressive secondary angle-closure glaucoma that is defined by intraocular neovascularization(NV) of the iris and/or anterior chamber angle with increased intraocular pressure (IOP), which leads to devastating visual consequences that complicate a number of systemic and ocular disorders
. Changes in the optic disc are nonspecific, and glaucomatous optic neuropathy is not required for diagnosis of the disease. NVG is a secondary inflammatory glaucoma that is characterized by increasing inflammation of the anterior segment of the eye, which is most frequently caused by deep retinal ischemia (ischemic and proliferative retinopathy
) that is encountered in various ischemic retinopathies, primarily proliferative diabetic retinopathy, the ischemic form of central retinal vein occlusion (CRVO), and ocular ischemic syndrome(OIS); however, some cases are associated with other ocular and extraocular entities
. NVG is a progressive disease with the potential for evolution even after medical or surgical normalization of the increased IOP. This disease is generally secondary to an advanced underlying systemic condition that exists among the various etiologies of NVG. Therefore, retinal ischemia and proliferative diabetic retinopathy-associated microangiopathy are generally elements of advanced systemic microangiopathy and tissue ischemia. CRVO is also frequently associated with systemic hypertension, arteriosclerosis, and hypercoagulability.
10月22日中國復(fù)合肥零售價格指數(shù) (CCRI) 為 2499.54點,環(huán)比上漲28.24點,漲幅為1.14%;同比上漲211.78點,漲幅為9.26%;比基期上漲52.83點,漲幅為2.16%。
The term NVG emphasizes the essential particularities of this glaucoma, namely, the formation of new vessels and not the intraocular hemorrhage that is not always present. Most known cases of rubeosis iridis are characterized by chronic and diffuse involvement of the posterior segment of the eyeball,with preceding ischemic retinal disease in most cases. The lower the ophthalmic blood pressure is, the more important the alterations of the iris. The iris displays an extreme and rapid sensitivity to an extended or even transitory state of retinal ischemia. Angiographic alterations of the iris vessels frequently accompany ischemia and necrosis of the inner retina. The essential role of iris and trabecular NV justifies the terms rubeotic and NVG. NVG does not invariably follow the development of iris NV. Once NV is detected, patients should be carefully followed with repeated biomicroscopic and gonioscopic examinations before pupil dilation. The present review discusses some aspects of the etiology, pathogenesis,and diagnosis of NVG.
PIIE: 全球全要素生產(chǎn)率增速有望反彈。近日,美智庫彼得森國際經(jīng)濟(jì)研究所(PIIE)發(fā)文稱,1995—2007年,全球全要素生產(chǎn)率年增長率為1.4%;2007—2016年大幅下降至0.4%。隨著近期經(jīng)濟(jì)活動不斷改善,全球全要素生產(chǎn)率增長率有望反彈。
ETIOLOGY
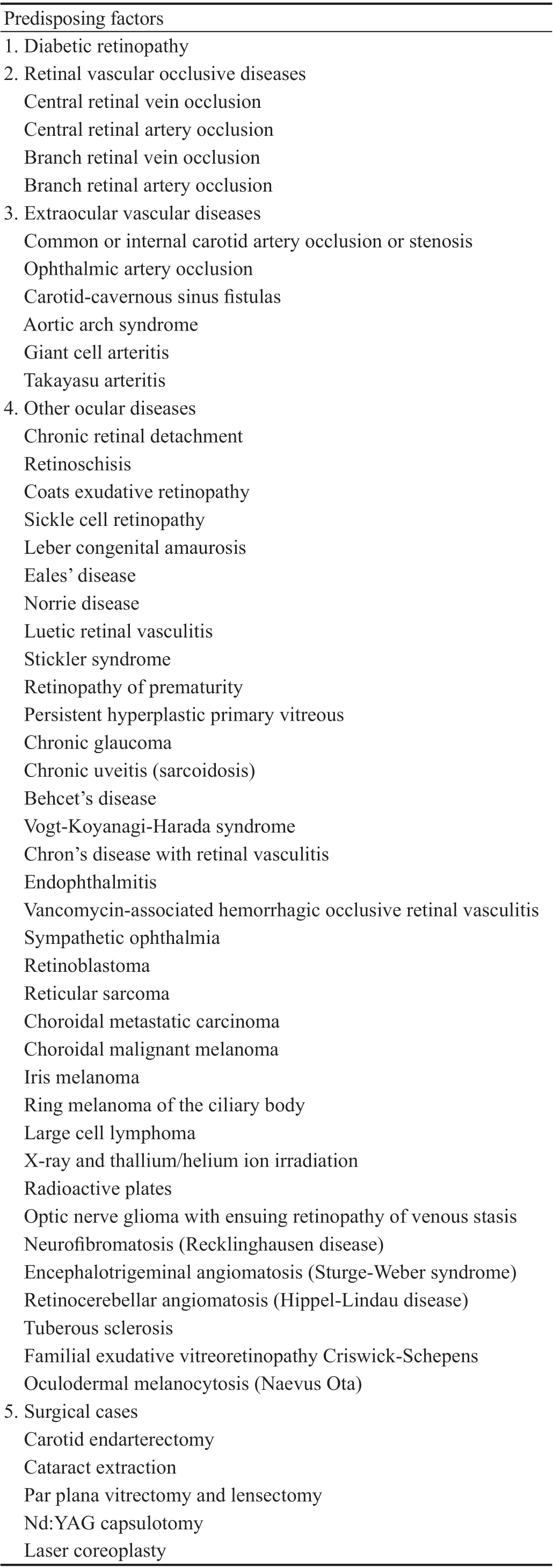
NVG may occur in patients with many ocular and systemic diseases, most frequently including diabetic retinopathy,ischemic CRVO, and OIS. Most of these diseases are associated with widespread retinal ischemia in the form of extensive capillary nonperfusion. Retinal diseases and other ocular and extraocular diseases that may lead to rubeosis iridis and NVG are listed in Table 1
.
Diabetes is the most common cause of NVG, which is an advanced manifestation of diabetic retinopathy that generally occurs in association with proliferative diabetic retinopathy. The rate of iris NV reaches 65% in these eyes, and the rate of NVG reaches 5%-8%
.The appearance of rubeosis iridis and NVG are directly linked to the duration of diabetes. NVG rarely occurs in adults with diabetes with a disease duration of less than 15y. The development of rubeosis iridis in an eye with nonproliferative diabetic retinopathy without significant retinal ischemia suggests the coexistence of other conditions,such as carotid artery disease and OIS. The average age of patients with diabetes presenting with NVG is significantly lower than that of patients with CRVO-emergent NVG. The period between retinal involvement and the occurrence of changes to the anterior segment of the eyeball is longer in patients with diabetes than in patients with CRVO. Ocular NV and NVG associated with diabetic retinopathy are not as aggressive or severe in development as those conditions appearing in patients with ischemic CRVO
. The risk of NVG is significantly increased following vitrectomy and lensectomy in patients with diabetic retinopathy due to the better access of vasoproliferative mediators to the anterior segment of the eyeball. Iris NV and NVG are common complications after vitrectomy in patients with diabetes. If cataracts are extracted concomitantly with vitrectomy, the rate of postoperative complications is much higher.
At this stage, contraction of the fibrovascular membrane covering the iris and trabeculum results in radial traction with gradual synechial closure of the anterior chamber angle and the formation of extensive irreversible peripheral anterior synechiae along the trabecular meshwork (goniosynechiae), causing secondary angle-closure glaucoma
. The IOP is very high (40-60 mm Hg) and is accompanied by ocular pain, corneal edema, and the Tyndall effect. Blood leakage from the incompetent and abnormal new blood vessels may cause hyphema
.
The iris stroma is flattened, and the pupil becomes fixed and semidilated. At the level of the pupil, radial traction on the anterior surface of the iris results in pupillary distortion and an ensuing eversion of the posterior iris surface over the pupillary margin, called uveal ectropion. This condition is almost always accompanied by closure of the angle on the same meridian. Finally, complete angle closure occurs with large iridocorneal adhesions such that the iris is almost in contact with the peripheral cornea at the level of the Schwalbe line, which leaves no angle structures visible. This final stage of glaucoma produces a completely closed zipper appearance of the camerular angle with coalescing peripheral anterior synechiae. An endothelial layer is also present in some cases, which continues with the corneal endothelium and creates a pseudocamerular angle.Modifications of the optic disc are nonspecific. Differential diagnosis includes advanced stages of primary open angle and angle-closure glaucoma and malignant glaucoma.
NVG occurs in patients with ischemic CRVO and more rarely in patients with ischemic hemi-CRVO,in patients with retinal vein occlusion in multiple branches simultaneously and involving wide retinal areas, and in patients with venous occlusion on a background of nonproliferative diabetic retinopathy
.
We are grateful for financial supports from the National Natural Science Foundation of China (51775288).
OIS encompasses a spectrum of clinical findings that result from chronic ocular hypoperfusion. Severe carotid artery occlusive diseases primarily cause OIS, which is the third most frequent cause of NVG, accounting for 13% of cases
. Atherosclerosis of the carotid vascular system is the major cause of OIS and may be its initial manifestation. In most cases of carotid artery occlusive disease (stenosis and occlusion of the common or internal carotid arteries), a significant collateral circulation develops between the internal and external carotid arterial systems or between the two internal carotid arteries to prevent the critical degree of retinal ischemia required for the occurrence of NV. Patients who develop OIS show decreased blood flow in the retrobulbar vessels and a reversal of blood flow in the ophthalmic artery
. The degree of stenosis, the presence or absence of collateral vessels, and the chronicity of carotid artery occlusive disease are involved in the pathogenesis of OIS. OIS should be suspected when iris NV is observed in eyes without a history of ischemic CRVO or in the eyes of patients without diabetes. Iris NV may lead to increased IOP and NVG. Some eyes may initially appear normal or even present with ocular hypotony despite the presence of fibrovascular tissue closing the angle because of ischemia of the ciliary body and the ensuing reduction in its perfusion with low aqueous humor production. This low IOP in eyes with well-established NVG (even when the chamber angle is significantly obstructed by goniosynechiae) should suggest occlusive disease of the carotid artery. After surgical re-establishment of ocular blood flow and increased perfusion of the internal carotid artery and ciliary body, the IOP increases dramatically and worsens the NVG. Other extraocular vascular diseases, namely, ophthalmic artery occlusion, carotid-cavernous fistula, aortic arch syndrome, giant cell arteritis, and Takayasu arteritis, may also lead to a decrease in the ocular blood supply and result in ischemia of the anterior and posterior segments of the eyeball with the development of iris NV and NVG.
Branch retinal artery occlusion is a rare cause of iris NV.
Central retinal artery occlusion (CRAO) is an uncommon cause of NVG. Unlike retinal anoxia from CRAO, retinal hypoxia from CRVO triggers the neovascular stimulus required for the development of NVG, which may explain the rarity of NVG in arterial compared to venous occlusion. The existence of creeping capillaropathy in patients with CRVO explains why NVG occurs more frequently in patients with CRVO than in patients with arterial occlusion. The chronically hypoxic retina in individuals with ischemic CRVO induces the production and secretion of vasoproliferative factors, such as vascular endothelial growth factor (VEGF), but the infarcted or necrotic retina resulting from CRAO does not have this capability.The estimated incidence of NVG following CRAO ranges from 2% to 17%
. The low incidence of NVG in CRAO may be because retinal ischemia is generally so complete that insufficient viable retinal tissue is available to produce the stimulating agent for NV. However, the severe ischemia induced by arterial occlusion does not result in anoxia of the entire retina because it involves only the inner retina and leaves viable cells in the inner nuclear layer of the retina, which respond to the neovascular stimulus, and the choriocapillaris continues to oxygenate the outer retina. Patients with NVG due to arterial occlusion are generally older, with advanced carotid changes and diffuse arteriosclerosis, which are key risk factors for the emergence of arterial occlusion and ocular NV.The delay in the occurrence of NVG after CRAO is shorter(5-9wk) than that after CRVO (12-24wk). Repermeabilization is the rule in arterial occlusion, and the capillary bed retains some competence. The changes are different in individuals with CRVO. Although the extent of venous occlusion is accentuated and arterial perfusion becomes insufficient, a permanent alteration of the capillary bed walls may occur,which explains the irreversible creation of the large territories of exclusion. Notably, the effect of panretinal photocoagulation(PRP) is very different from the effects of arterial occlusion.Specifically, destruction of the entire retina is observed in patients treated with PRP, especially PRP of the outer retina,followed by degeneration of the most internal layers. PRP produces the conversion of ischemic but viable retinal tissue that produces angiogenic factors into avascular, nonviable retinal tissue that no longer produces these factors.
在語言交際中,同樣會出現(xiàn)語言之間的結(jié)構(gòu)相互適應(yīng)與選擇,其屬于語言順應(yīng)論范疇。語言使用是語言發(fā)揮功能作用的過程,語言使用者需根據(jù)不同語言環(huán)境來選擇語言交際手段,以達(dá)到預(yù)期交際意圖。翻譯同語言交際一樣,也是一個文化選擇的過程。選擇源語材料之后,譯者就需要分析文本,找準(zhǔn)文化立場,選擇恰當(dāng)?shù)姆g方法,運用合適的翻譯策略。在翻譯過程中,這種選擇與順應(yīng)的過程是一種動態(tài)的順應(yīng),這與權(quán)變思想已然相通。經(jīng)權(quán)相濟(jì)是一種辯證、靈活的思維模式,也是一種有效的調(diào)節(jié)機制。
The rate of iris NV with NVG reaches 10%
in the nonischemic form of CRVO. Eyes with nonischemic CRVO may develop NV and NVG in association with diabetic retinopathy or OIS. NVG appears 8-15wk after CRVO and is called 90-day glaucoma because the average latency period is 3mo
. It may occur in the very first month or at any other time interval after CRVO appears. Before starting CRVO treatment, clinicians must determine whether the occlusion is ischemic in nature.Ischemic-type CRVO is defined by a nonperfused retinal area larger than 10 disc diameters on fluorescein angiography.Notably, fluorescein angiography provides no information at all or sometimes provides misleading information on retinalcapillary nonperfusion in at least one-third of eyes during the early, acute phase of CRVO. For these eyes, in which marked and extensive intraretinal hemorrhages prevent a clear angiographic evaluation of retinal capillary nonperfusion zones, the diagnosis of the ischemic type is based on the presence of at least 4 of the 5 following criteria: best-corrected visual acuity (BCVA) ≤20/400 Snellen equivalent; ability to see ≤V/4e isopter with the Goldmann perimeter; presence of the relative afferent pupillary defect in patients with a normal fellow eye; extensive ocular fundus changes (a more striking number of hemorrhages, venous tortuosity, cotton wool spots(>5), and disc and macular edema); and reduction in the IOP of the occluded eye of ≥4 mm Hg compared to that of the fellow eye
. The cumulative risk of NVG development in patients with ischemic CRVO reaches a maximum of 40%-45%
after several years, and 80% of cases occur in the first 7-8mo
.The risk of the conversion of a nonischemic to an ischemic form is 30%
, and this risk increases in proportional to the extent of intraretinal hemorrhages.
2) NVG is a potentially devastating consequence of fibrovascular proliferation of the eye with ensuing obstruction of the trabecular meshwork.
PATHOGENESIS
VEGF and its isoform VEGF A are important and likely predominant factors involved in the pathogenesis of intraocular NV and NVG. VEGF is an inflammatory, angiogenic,permeable glycoprotein that is produced by many cells,including vascular endothelial cells, retinal capillary pericytes,retinal pigment epithelial cells, Müller cells, astrocytes, and retinal ganglion cells. The nonpigmented ciliary epithelium is also an important site of VEGF synthesis. The VEGF level is normally in equilibrium with that of pigment epitheliumderived growth factor (PEDF), an antiangiogenic factor. When the equilibrium between VEGF and PEDF is shifted in favor of VEGF, VEGF binds to
its receptors on the surface of vessel endothelial cells, which has a mitogenic effect on inducing angiogenesis
the activation, proliferation, and migration of endothelial cells, the induction of inflammation,and increases in vascular permeability. VEGF is a key molecule involved in ocular NV.
The prerubeotic stage is characterized by a normal IOP and clinical findings of underlying conditions that may cause retinal ischemia, such as diabetic retinopathy,ischemic CRVO, or OIS
. In the presence of a causal factor,the likelihood of the occurrence of iris NV and its development toward NVG must be estimated. The identification of patients at risk in this stage is of the utmost importance because it is the best time to intervene and prevent the occurrence of NVG
.
Diabetic disease generally exists for many years before the occurrence of rubeosis iridis, and proliferative diabetic retinopathy is already present at the time of its diagnosis in most cases. Iris NV appears less frequently in eyes with nonproliferative diabetic retinopathy, and the possible contribution of predisposing factors such as obstructive disease of the carotid arteries to the emergence of iris NV should be determined. The risk of iris NV and NVG increases in patients with diabetic retinopathy if retinal areas of capillary or arteriolar nonperfusion are present or if the patient has undergone vitrectomy or lensectomy in the past. New vessels on the iris and angle are not detectable in the prerubeosis stage.Long before the clinical detection of iris NV, the seemingly normal iris vessels allow leakage of fluorescein through vascular wall defects to highlight the rupture of the ocular blood barrier, which is not normally observed (
, occult NV). This alteration of the vascular endothelium of preexisting blood vessels precedes the formation of new vessels. In CRVO, biomicroscopy reveals tortuosity and engorgement of all branches affected by CRVO, extensive deep blot and flameshaped hemorrhages in the peripheral retina and posterior pole, severe disc edema and disc hyperemia. The area of the nonperfused retina and the presence of peripheral retinal hemorrhages are directly associated with the development of NVG in individuals with ischemic CRVO.
NVG results from the formation of a fibrovascular membrane initially on the anterior face of the iris that continues at the iridocorneal angle preceding the increase in IOP. The trabeculum is occluded by this membrane, which is gradually drawn forward to close the angle. Fibrovascular proliferation of the anterior segment ultimately causes the formation of progressive peripheral anterior synechiae that progressively close the anterior chamber angle and produce an intractable increase in IOP. Obstruction of the trabecular meshwork by the fibrovascular membrane and the associated inflammatory and hemorrhagic phenomena are implicated in the pathogenesis of NVG.
DIAGNOSIS
The full disease is characterized by iris NV, a closed anterior chamber angle, high IOP with severe eye pain, and devastating visual outcomes
. The evolution of clinical and pathological changes from the causal condition to the appearance of iris NV and NVG occurs in 4 stages, as visualized using anterior biomicroscopy and gonioscopy: prerubeosis, preglaucoma (rubeosis iridis), open angle glaucoma and angle-closure glaucoma.
Retinal ischemia and hypoxia initiate and accelerate the production and secretion of myriad vasoproliferative growth factors, including VEGF (the major angiogenic factor contributing to the process of ocular NV), insulin growth factor-1, the inflammatory cytokines interleukin (IL)-6,endothelin-1, and nitric oxide, and the expression of plateletderived growth factor-C
, transforming growth factor beta 1 and beta 2, and other angiogenic factors, which trigger or favor the release of a cascade of angiogenic factors that promotes the development of iris and anterior chamber angle NV
. These factors induce proliferative ischemic retinopathy in the posterior segment of the eyeball and diffuse
(anteriorly) into the anterior segment, causing iris and anterior chamber angle NV. Lensectomy, Nd:YAG laser capsulotomy, and other procedures that reduce barriers to the diffusion of these angiogenic factors may be associated with a high incidence of rubeosis iridis. The vasoproliferative factors use the same passages as the aqueous humor, which explains the preferential impairment of vessels of the pupillary margin over angular vessels. Intraocular surgeries such as cataract extraction increase the risk of anterior segment NV because VEGF moves more easily into the anterior chamber in a pseudophakic eye, especially an aphakic eye.
The IOP is normal in this stage if the patient does not have preexisting primary open angle glaucoma
. Iris NV begins to develop in addition to retinal ischemia. A careful examination of the iris and camerular angle is essential before dilation of the pupil and instillation of any eye drops. Anterior biomicroscopy shows tiny tufts of new vessels from preexisting iris capillaries and fine, delicate new aberrant vessels that are arranged irregularly at the pupillary border and extend to the trabecular meshwork in a nonradial pattern, unlike the normal iris vessels that tend to lie in the stroma and are radial in orientation
. New vessels exhibit gaps in endothelial cells on electron microscopy and basement membrane changes. These new tortuous and irregular dilated vessels are highlighted on iris angiography,which shows the rapid and massive leakage of fluorescein through vascular wall defects at the level of the pupillary margin. Gonioscopy shows a normal chamber angle with a fine net of newly formed vessels that extend beyond the ciliary body band and sclera spur branching onto the surface of the trabecular meshwork, whereas normal vessels are typically retained behind the scleral spur
. The angle examination must be performed under high magnification with minimal pressure on the gonioscopic lens to prevent the emptying of abnormal new blood vessels and to avoid overlooking early angle NV
.Iris NV generally precedes angle NV, but the opposite result has also been reported, which justifies the need for a thorough gonioscopic examination. The preglaucoma stage in patients with CRVO is not fundamentally different from this stage in patients with diabetes, but its progression is generally faster and more explosive. The neovascular network appears more regular and finer in patients with diabetes than in patients with CRVO. This network is difficult to highlight in patients with diabetes, especially in subjects with brown irises. The differential diagnosis of the preglaucoma stage includes several conditions with engorged iris vessels, such as anterior uveitis and retinopathy of prematurity
.
NV of the chamber angle must be differentiated from vessels that are normally observed on routine gonioscopic examination. Specifically, the normal blood vessels are localized behind the scleral spur near the root of the iris, and the abnormal vessels cross the scleral spur and trabecular meshwork.
“四十年前,三北防護(hù)林工程啟動后,政府號召種樹。當(dāng)時,村長給村民開會,要求村民種楊樹。其實,不用村長說,大家心里都有數(shù)——楊樹不挑剔,種上就活,不用過多管它。”
Venous and arterial occlusion are representative diseases.
Pain and inflammatory signs develop rapidly and almost without warning because earlier stages of the development of iris NV frequently pass unperceived.The eye is red with dilatation of the episcleral vessels and perikeratic injection, the cornea is edematous, with flattening and effacement of the anterior surface of the iris, and the anterior chamber becomes deep and shows the presence of flare. The pupil is fixed and semidilated as a result of ischemia of the pupil sphincter. It is frequently irregular due to the presence of posterior synechiae. The iris NV reaches the trabeculum and passes through the front of the lens.Examination by biomicroscopy does not generally allow visualization of the fine fibrovascular membrane, consisting of proliferating myofibroblasts with contractile properties,that develops along these newly immature formed vessels and passes on the anterior surface of the iris and within the iridocorneal angle, sometimes extending onto the posterior surface of the iris. The trabeculum is obstructed by this iridotrabecular fibrovascular membrane, which is gradually drawn forward to occlude the angle. The iridocorneal angle remains partially open in various regions of the angle with a sharp NV, and the IOP is high and may increase suddenly,similar to the clinical presentation of acute glaucoma
.Hyphema is frequently present during this dramatic onset and may contribute to or precipitate an acute increase in IOP. NVG after CRVO has a fulminating evolution compared to diabetic retinopathy. Optic glaucomatous neuropathy may develop in this stage due to the increased IOP. The differential diagnosis includes several ocular disorders with associated iris or angle vessel variants that may mimic true NV, such as Fuchs’heterochromic iridocyclitis, severe nongranulomatous uveitis with dilated iris vessels and protein in the aqueous humor,essential iris atrophy, and pseudoexfoliation syndrome.
CONCLUSIONS
1) NVG is a devastating and intractable severe ocular disease that may cause blindness and is directly linked to prolonged retinal ischemia and the proliferation of newly formed vessels on the iris and camerular angle.
Other ocular diseases and surgical cases are thoroughly described in Table 1 and are less frequently causes of iris NV and NVG. Retinal ischemia and the development of retinal capillary nonperfusion are the most likely factors responsible for the emergence of ocular NV and NVG in patients with many of these diseases.
3) VEGF is an important and likely predominant protein involved in the pathogenesis of intraocular NV and NVG.
“他是我親弟,昨天從衢州趕來給我報喪,早上就被炸死在碉堡里,后來,被鬼子割了頭。所有的弟兄都被鬼子割了頭。”孔老一慢慢說著,好像在說別人的故事。
4) The evolution of the clinical and histopathological changes from the predisposing condition to the appearance of rubeosis iridis and NVG is divided into 4 stages: prerubeosis,preglaucoma, open angle glaucoma, and angle-closure glaucoma.
4)對2股滲瀝液進(jìn)行中試試驗,結(jié)果表明,當(dāng)進(jìn)水氨氮為1 700 mg/L時,塔釜液最終出水氨氮濃度低于75 mg/L,滿足設(shè)計值;塔頂出料濃度最高為67 875 mg/L,未達(dá)到設(shè)計值。……
 International Journal of Ophthalmology
2022年6期
International Journal of Ophthalmology
2022年6期
- International Journal of Ophthalmology的其它文章
- Intraocular lens removal or not during vitrectomy for acute infectious endophthalmitis after cataract surgery
- Vitreous function and intervention of it with vitrectomy and other modalities
- Short-term outcomes of mitomycin C-augmented excisional bleb revision with capsulectomy for failed Ahmed glaucoma valve
- Evaluation of nintedanib as a new postoperative antiscarring agent in experimental extraocular muscle surgery
- Multimodal imaging of experimental choroidal neovascularization
- A novel Nance-Horan syndrome mutation identified by next-generation sequencing in a Chinese family
