影響高血壓腦出血患者手術治療后近期預后不良的危險因素
胡慧慧 趙敬平 楊剛 鐘玉婷
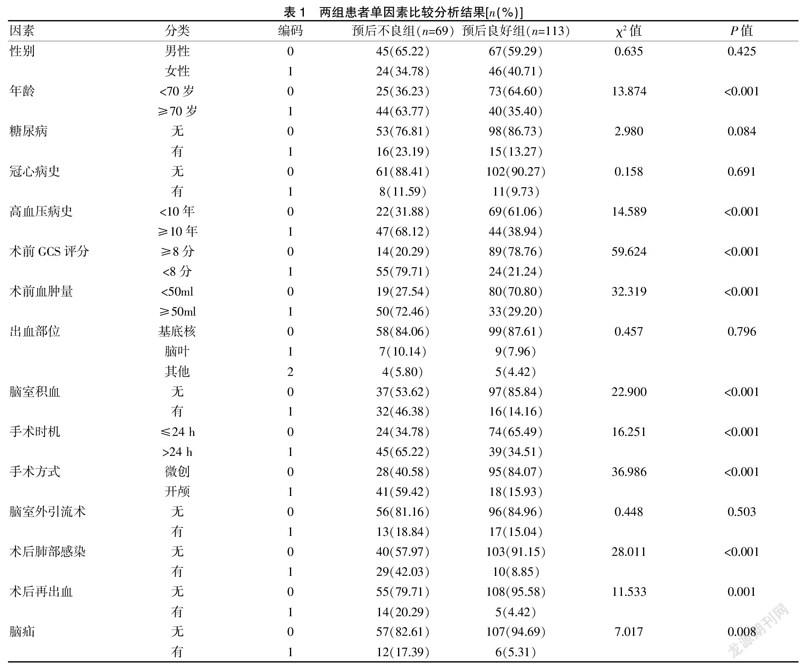

[摘要] 目的 探討影響高血壓腦出血(HICH)患者手術治療后近期預后不良發生率及其相關危險因素。 方法? 選取2019年1月至2020年12月浙江省諸暨市人民醫院收治的182例HICH患者進行隨訪,依據術后3個月的預后情況,將其分為預后不良組(69例)和預后良好組(113例);比較兩組間年齡、性別、糖尿病、冠心病史、高血壓病史、術前GCS評分、術前血腫量、出血部位、腦室積血、手術時機、手術方式、腦室外引流術、術后肺部感染、術后再出血、腦疝等因素分布;再采用多因素logistic回歸法篩選影響HICH患者術后預后不良的相關危險因素。結果? 182例HICH患者術后3個月的預后不良發生率為37.91%(69/182);多因素logistic回歸結果顯示:影響HICH患者手術治療后預后不良的危險因素包含年齡(OR=2.869)、術前GCS評分(OR=4.811)、術前血腫量(OR=3.536)、手術時機(OR=3.294)、開顱手術(OR=4.137)、術后肺部感染(OR=3.885)、術后再出血(OR=3.083)。結論? HICH患者術后近期預后不良發生率高達38%,且影響其近期預后不良的高危因素較多,應早期進行預防和治療,降低預后不良發生率,改善HICH患者的預后。
[關鍵詞] 高血壓腦出血;手術;預后;危險因素
[中圖分類號] R743.2? ? ? ? ? [文獻標識碼] B? ? ? ? ? [文章編號] 1673-9701(2022)13-0038-04
[Abstract] Objective To explore the incidence of poor prognosis and its related risk factors in patients with hypertensive intracerebral hemorrhage (HICH) after surgical treatment. Methods A total of 182 HICH patients admitted to Zhuji People′s Hospital of Zhejiang Province from January 2019 to December 2020 were followed up. According to the prognosis after 3 months, they were divided into the poor prognosis group (69 cases) and the good prognosis group (113 cases). The age, gender, diabetes, coronary heart disease history, hypertension history, preoperative GCS score, preoperative hematoma volume, bleeding site, intraventricular hemorrhage, operation opportunity, operation method, extraventricular drainage, postoperative pulmonary infection, postoperative rebleeding and cerebral hernia were compared between the two groups. Then, multivariate Logistic regression was used to screen the related risk factors affecting the poor postoperative prognosis of HICH patients. Results The incidence of poor prognosis of 182 patients with HICH 3 months after operation was 37.91% (69/182). Multivariate Logistic regression showed that the risk factors affecting the poor prognosis of HICH patients after surgical treatment included age (OR=2.869), preoperative GCS score (OR=4.811), preoperative hematoma volume (OR=3.536), surgical opportunity (OR=3.294), craniotomy (OR=4.137), postoperative pulmonary infection (OR=3.885) and postoperative rebleeding (OR=3.083). Conclusion The incidence of short-term poor prognosis of HICH patients is as high as 38%, and there are many high-risk factors that affect their short-term poor prognosis. Early prevention and treatment should be carried out to reduce the incidence of poor prognosis and improve the prognosis of HICH patients.
[Key words] Hypertensive cerebral hemorrhage; Operation; Prognosis; Risk factor
高血壓腦出血(hypertensive intracerebral hemorrhage,HICH)是由于高血壓所引起的腦內動靜脈或毛細血管破裂從而造成腦出血等癥狀的腦血管疾病,約占我國腦血管意外的30%,病死率高達38%~43%[1];多見于基底核、腦葉部位出血,多損及內囊,臨床表現為突然劇烈頭痛、躁動、嗜睡、昏迷等[2]。腦外科血腫清除術是治療HICH最為常用的方法,可迅速解除血腫壓迫、減少腦組織神經細胞的損傷,盡管如此,患者術后仍會有不同程度的后遺癥,從而影響患者的預后和生活質量[3]。……

