Multimodal imaging in Purtscher-like retinopathy associated with sarcoidosis: a case report
鼻咽癌是一種較常見的惡性腫瘤,發生在鼻咽部位,有研究表明,大多數為低分化鱗癌,具有較高的惡性程度,發生廣泛轉移、局部浸潤的可能性也比較高。腫瘤細胞可能對顱底造成破壞,進而對腦組織形成侵犯。另外,對于鼻咽癌來說,其發生淋巴結轉移的機率也相對較高。由于鼻咽癌發病位置解剖結構特殊,周圍重要的神經組織、血管等比較豐富,因此手術治療有較大的局限[1-2]。鼻咽癌對放射治療敏感性較高,所以一般采用放射治療的方法,常規放射治療效果一般,采用調強放射治療,對靶區三維形狀進行獲取,減少對正常組織的照射劑量,能保護正常組織,減少副反應,并且提高治療效果[3-4]。
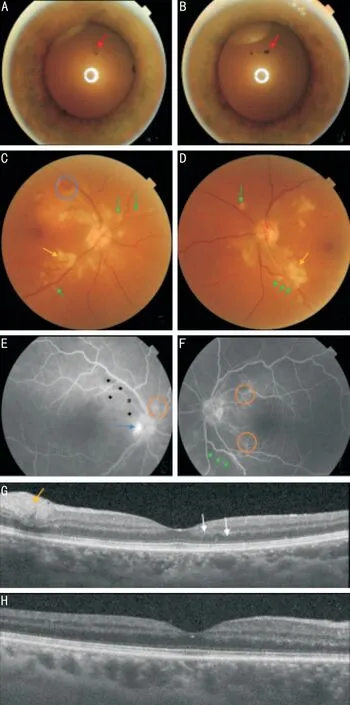
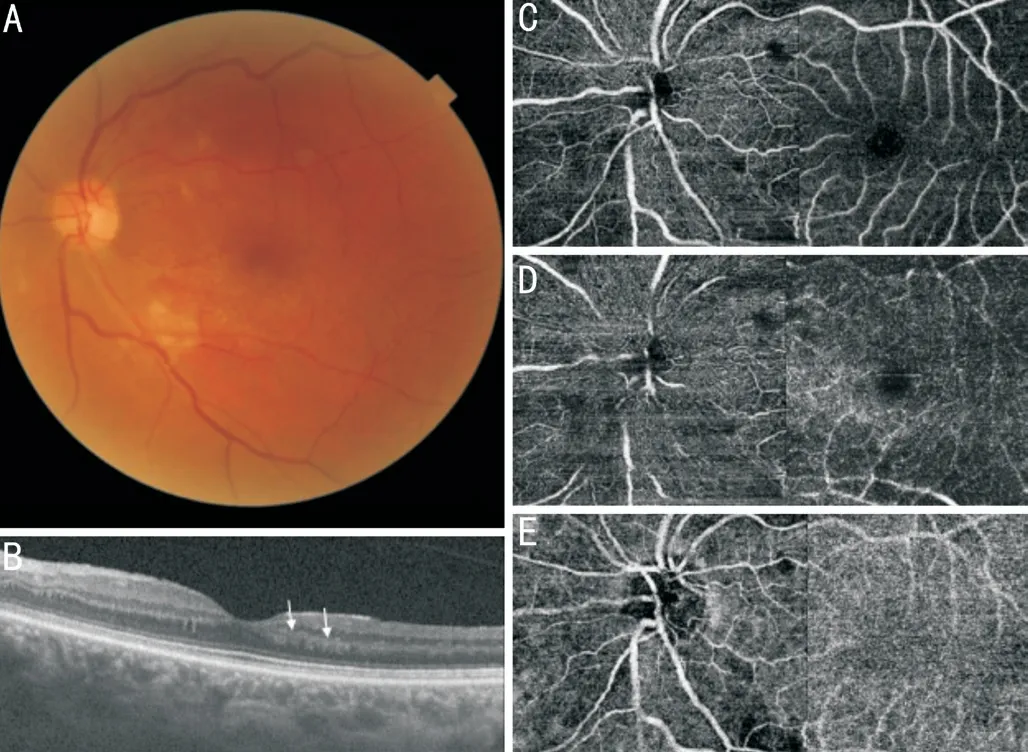
We report a case of Purtscher-like retinopathy (PLR)in the presence of acute pancreatitis secondary to sarcoidosis. To our knowledge, this is the first case report of a PLR in a patient with sarcoidosis. A 54-year-old female, hospitalized at the Internal Medicine Department for stage E pancreatitis, hypercalcemia, and mediastinal lymphadenopathies, consulted with a visual impairment in both eyes evolving for a month, especially in her left eye (LE). The best-corrected visual acuity (BCVA), was 20/32 in the right eye(RE) and 20/50 in the LE. The slit-lamp examination revealed iris pigments on the anterior lens capsule, corresponding to disrupted posterior synechiae in both eyes (Figure 1A,1B). The vitreous was clear, whereas fundus examination(Figure 1C, 1D) showed a stage 1 papillary edema and few superficial intra-retinal hemorrhages in the RE associated with multiple peri-papillary cotton-wool spots (CWS) in both eyes. Moreover, we noted focal whitening surrounding the retinal arterioles with a clear zone on either side of the vessels(Purtscher fleken). These findings were compatible with the diagnosis of PLR. Fluorescein angiography (FA) showed papillary early hyper fluorescence (papillary edema), peripapillary non-perfusion areas associated with late capillary staining. We also noted peri-papillary and peri-vascular hypofluorescent spots, corresponding respectively to CWS and Purtscher fleken (Figure 1E, 1F). Macular Swept-source optical coherence tomography (SS-OCT) detected a focal thickening of the retinal fiber layer corresponding to CWS in both eyes.Besides, hyperreflectivity of the inner nuclear layer consisting of a paracentral acute middle maculopathy (PAMM), was revealed in the LE (Figure 1G, 1H). However, no disruption of the ellipsoid zone or macular thickening was noted. Sweptsource optical coherence tomography angiography (SSOCTA) showed superficial and deep capillary non-perfusion(CNP) areas (Figure 2A-2D). Flow void areas were noted in the choriocapillaris, in addition to a shadowing effect due to the overlying CWS (Figure 2E, 2F). Regarding the association of ocular inflammation sequelae (disrupted posterior synechiae) with hypercalcemia and deep lymphadenopathies,the diagnosis of sarcoidosis was suspected. However, the dosage of angiotensin-converting enzyme and salivary gland biopsy was normal. Infectious causes, including tuberculosis,systemic diseases, and malignancies were ruled out. Thus,a mediastinoscope-guided biopsy of the lymphadenopathies was performed. Histopathological specimen revealed, giant cells with non-caseating granulomas, confirming the diagnosis of sarcoidosis. The patient received an immunosuppressive dose of systemic steroids, initiated by three intravenous boluses of methylprednisolone (1 g/d) followed by oral prednisolone(1 mg/kg·d). A month later, the patient’s vision improved, with a BCVA of 20/25 in both eyes. The fundus examination revealed a decrease in the number of CWS and the disappearance of retinal hemorrhages (Figure 3A). The PAMM persisted in the LE (Figure 3B). However, CNP and flow void areas decreased on OCTA (Figure 3C-3E).
此外,加之金融方式的介入以及B2C模式形成的在線直供,最終形成了一個完整的全產業鏈閉環。一位肥料企業老總“驚爆”:“傳統肥料企業已經意識到迫近的形勢,全產業鏈服務模式讓我們沒有活路了。”
DISCUSSION

Acute pancreatitis is the first cause of PLR, it represents 19.1% of cases
. The physiopathology of this retinopathy, in the cases of acute pancreatitis, was explained by complement activation that results in leukocyte aggregates or leukoemboli,which are released in the bloodstream and occlude the retinal vessels
. In sarcoidosis, pancreatic involvement is uncommon,moreover acute pancreatitis due to hypercalcemia is rare
. The association between systemic diseases and PLR was reported in some cases, however, to our knowledge, the association between sarcoidosis and PLR was never described. Sarcoidosis is well known to induce occlusive retinal vasculitis
, thus we hypothesized that microangiopathy that led to the PLR,in our case, could be explained by two vascular occlusive entities, sarcoidosis, and acute pancreatitis. In the context of a probable etiology, the diagnosis of PLR is based on a sudden visual impairment (bilateral in 60% of cases) and fundoscopic findings restricted to the posterior pole: CWS,retinal hemorrhages, and Purtscher flecken. Papillary edema has been observed in some cases
. FA shows different degrees of CNP areas and fluorescein staining from retinal vessels,according to the severity of the retinopathy. Hypo-fluorescent spots corresponding to the CWS and Purtscher flecken are also observed
. In the majority of cases of PLR, optical coherence tomography shows macular edema
. However, in this case, the macular thickness was normal, and a PAMM was revealed. This condition in the context of PLR, might be explained by the ischemia induced by the retinal arteriolar emboli
. SS-OCTA is a recent multimodal imaging technique that showed, in this case, not only multiple areas of CNP in the superficial and deep capillary plexuses but also flow void in the choriocapillaris, described by Li
as a honeycomblike pattern. This finding suggests the involvement of the choroid in the physiopathology of PLR. The evolution of PRL is favorable in some cases, however, no prognosis criteria have been fixed
. In this case, the patient regained a correct visual acuity in both eyes, despite the persistence of PAMM in her LE. This evolution might be explained by the decrease in CNP areas in the retinal capillary plexuses and the choriocapillaris as shown on SS-OCTA. The treatment of PLR is based on treating the underlying cause, corticosteroids in our patient,however, no consensus has been defined
.
None;
None;
None;
None;
None;
None.
1 Miguel AIM, Henriques F, Azevedo LFR, Loureiro AJR, Maberley DAL. Systematic review of Purtscher’s and purtscher-like retinopathies.
(
) 2013;27(1):1-13.
2 Behrens-Baumann W, Scheurer G, Schroer H. Pathogenesis of Purtscher’s retinopathy. An experimental study.
1992;230(3):286-291.
3 Gebreselassie A, Mehari A, Dagne R, Berhane F, Kibreab A.Hypercalcemic pancreatitis a rare presentation of sarcoidosis: a case report.
(
) 2018;97(2):e9580.
4 Pasadhika S, Rosenbaum JT. Ocular sarcoidosis.
2015;36(4):669-683.
5 Li B, Li DH, Chen YX. Purtscher-like retinopathy presented a honeycomb-like pattern in optical coherence topography angiography.
2019;19(1):232.
6 Vezzola D, Allegrini D, Romano MR, Pagano L, Montericcio A, Fogagnolo P, Rossetti LM, de Cillà S. Optical coherence tomography angiography in Purtscher-like retinopathy associated with dermatomyositis: a case report.
2019;13(1):206.
 International Journal of Ophthalmology
2022年5期
International Journal of Ophthalmology
2022年5期
- International Journal of Ophthalmology的其它文章
- Multimodal imaging in immunogammopathy maculopathy secondary to Waldenstrom’s macroglobulinemia: a case report
- Periorbital necrotizing fasciitis accompanied by sinusitis and intracranial epidural abscess in an immunocompetent patient
- Can a sneeze after phacoemulsification cause endophthalmitis? A case report
- Persistent macular oedema following Best vitelliform macular dystrophy undergoing anti-VEGF treatment
- Genetic, environmental and other risk factors for progression of retinitis pigmentosa
- lnflammation and dry eye disease—where are we?
