Prognostic value of neutrophil/lymphocyte,platelet/lymphocyte,lymphocyte/monocyte ratios and Glasgow prognostic score in osteosarcoma:A meta-analysis
Li-Peng Peng,Jie Li,Xian-Feng Li
Li-Peng Peng,Jie Li,Xian-Feng Li,Department of Orthopedic,The Second People's Hospital of Yibin,Yibin 644000,Sichuan Province,China
Abstract BACKGROUND Some studies investigated the prognostic role of several blood biomarkers,including the neutrophil/lymphocyte ratio(NLR),platelet/lymphocyte ratio(PLR),lymphocyte/monocyte ratio(LMR)and Glasgow prognostic score(GPS),in osteosarcoma,but their results were inconsistent with each other.AIM To identify the prognostic value of NLR,PLR,LMR and GPS in osteosarcoma patients through reviewing relevant studies.METHODS The PubMed,EMBASE,Web of Science and CNKI databases were searched up to October 2,2021.The primary and second outcomes were overall survival(OS)and disease-free survival(DFS),respectively.The hazard ratios(HRs)with 95%confidence intervals(CIs)were combined to assess the association between these indicators and prognosis of osteosarcoma patients.RESULTS A total of 13 studies involving 2087 patients were eventually included.The pooled results demonstrated that higher NLR and GPS were significantly associated with poorer OS(HR = 1.88,95%CI:1.38-2.55,P < 0.001;HR = 2.19,95%CI:1.64-2.94,P <0.001)and DFS(HR = 1.67,95%CI:1.37-2.04,P < 0.001;HR = 2.50,95%CI:1.39-4.48,P < 0.001).However,no significant relationship of PLR and LMR and OS(P= 0.085;P = 0.338)and DFS(P = 0.396;P = 0.124)was observed.CONCLUSION Higher NLR and GPS were related with worse prognosis and might serve as novel prognostic indicators for osteosarcoma patients.
Key Words:Neutrophil/lymphocyte;Platelet/lymphocyte;Lymphocyte/monocyte ratios;Glasgow prognostic score;Osteosarcoma;Prognosis;Meta-analysis
lNTRODUCTlON
Osteosarcoma is a malignant bone tumor that seriously affects the health of children and adolescents with annual incidence of 2-3/1 million,accounting for about 20%-30% of all primary bone tumors[1].It has the characteristics of high malignant degree,early metastasis and high mortality.Before the 1070s,the treatment of osteosarcoma was mainly based on the surgical resection with the five-year survival rate of 10%-20%[2,3].In recent years.Through the combination of preoperative neoadjuvant chemotherapy,surgical resection,postoperative adjuvant chemotherapy and other important therapies,the five-year survival rate of osteosarcoma patients has increased to 60%-70%[4,5].
However,osteosarcoma tends to metastasize to the lungs and nearly half of osteosarcoma cases have pulmonary metastases,which is the main cause of death in patients with osteosarcoma[6].Nevertheless,less than 20% of patients showed metastases at the time of diagnosis and the five-year survival rate of patients with pulmonary metastases is less than 30%[6,7].Thus,some reliable and valuable prognostic indicators are still clinically needed to accurately predict the survival of osteosarcoma patients and contribute to the formulation of appropriate treatment strategies.
In recent years,many haematological indexes have been reported to show high prognostic value in cancer patients,including the neutrophil to lymphocyte ratio(NLR)[8,9],platelet to lymphocyte ratio(PLR)[10,11],lymphocyte to monocyte ratio(LMR)[10]and Glasgow prognostic score(GPS)[12-14].Besides,the NLR has been also reported to play a role in predicting postoperative complications like the anastomotic leakage[15].Some investigators explored the prognostic value of these indicators in osteosarcoma[16-28],but inconsistent results were reported in their studies.Whether they could be used to predict prognosis of osteosarcoma patients in clinics remains unclear.
Thus,the aim of this study was to identify the prognostic role of NLR,PLR,LMR and GPS in osteosarcoma,which might help formulate the appropriate treatment strategies for osteosarcoma patients.
MATERlALS AND METHODS
This systematic review and meta-analysis were conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines[29].
Literature search
The PubMed,EMBASE,Web of Science and CNKI electronic databases were searched up to October 2,2021.The following key works were used during the literature search:neutrophil/lymphocyte ratio,neutrophil to lymphocyte ratio,NLR,platelet/ lymphocyte ratio;platelet to lymphocyte ratio,PLR,lymphocyte/monocyte ratio,lymphocyte to monocyte ratio,LMR,Glasgow prognostic score,GPS,osteosarcoma,osteogenic sarcoma,prognostic,prognosis and survival.Besides,the references cited in the included studies were also evaluated for availability.
Inclusion and exclusion criteria
The following inclusion criteria were applied:(1)Patients were pathologically diagnosed with osteosarcoma;(2)Patients were divided into two groups according to the NLR,PLR,LMR or GPS and the long-term survival of patients between the two groups were compared;and(3)Hazard ratios(HRs)with corresponding 95% confidence intervals(CIs)of overall survival(OS)or disease-free survival(DFS)were reported in the articles directly.
The following exclusion criteria were applied:(1)None of the prognostic value of NLR,PLR,LMR or GPS were investigated;(2)Duplicated or overlapped data;and(3)Conference abstracts,animal trials,case reports or reviews.
Data extraction and quality assessment
The following information were collected from included studies:the name of first author,publication year,country,sample size,indicators(NLR,PLR,LMR or GPS),cutoff values of NLR,PLR or LMR,endpoints and corresponding HRs with 95%CIs.
The Newcastle-Ottawa scale(NOS)was used for the quality assessment of included studies and highquality studies were defined as a NOS of 6 or higher[30].
In the current meta-analysis,the literature search,selection,data extraction and quality assessment were all performed by two authors independently and any disagreement was resolved by team discussion.
Statistical analysis
The HRs with 95%CIs were combined to assess the relationship between NLR,PLR,LMR and GPS and prognosis of osteosarcoma patients.The heterogeneity among included studies was evaluated byI2statistics andQtest.When obvious heterogeneity was observed presenting as theI2> 50% or(and)P<0.1,the random effect model was used;otherwise,the fix effect model was used[31].Considering the similarity,we combined the cancer-specific survival,event-free and progression-free as DFS.The sensitivity analysis was performed to detect the source of heterogeneity and evaluated the stability of pooled results.Besides,the Begg’s funnel plot and Egger’s test were conducted to detect publication bias[32].If significant publication bias was observed presenting as aP< 0.05,then the nonparametric trim-and-fill method was used to re-estimate a corrective effect size after publication bias was adjusted[33].All statistical analyses were conducted by STATA 15.0 software.
RESULTS
Literature selection process
Ninety-one records were initially identified and 21 duplicated records were removed.Then 28 potentially relevant publications were assessed and 10 of them were excluded because of meeting abstract,case reports and reviews.Eighteen full texts were reviewed and a total of 13 studies were included eventually[16-28].The detailed selection process was presented in Figure 1.
Basic characteristics of included studies
All include studies were retrospective.Most of them were from China and a total of 2087 patients were enrolled,with the sample size ranging from 55 to 327.All of them were high-quality studies with a NOS of 6 or higher.The specific information was presented in Table 1.
Association between NLR and prognosis of osteosarcoma patients
Eleven studies involving 1623 patients investigated the prognostic role of NLR in osteosarcoma[17-24,26-28].The pooled results indicated that higher NLR was significantly associated with poor OS(HR =1.88,95%CI:1.38-2.55,P< 0.001;I2= 80.2%,P< 0.001)(Figure 2A)and DFS(HR = 1.67,95%CI:1.37-2.04,P< 0.001;I2= 35.4%,P= 0.186)(Figure 2B).NLR was demonstrated to be a prognostic indicator for osteosarcoma patients(Table 2).
Association between PLR and prognosis of osteosarcoma patients
Eight studies involving 1215 patients explored the prognostic value of PLR in osteosarcoma patients[17,19-21,23,24,27,28].However,no significant relationship of PLR with OS(HR = 1.29,95%CI:0.97-1.72,P=0.085;I2= 77.4%,P< 0.001)(Figure 3A)and DFS(HR = 1.12,95%CI:0.87-1.44,P< 0.001;I2=0.0%,P=0.465)(Figure 3B)was observed(Table 2).
Association between LMR and prognosis of osteosarcoma patients
Six studies involving 906 participants were included to identify the association of LMR with prognosis of osteosarcoma patients[16,17,25-28].The pooled results manifested that LMR was not related with OS(HR = 0.82,95%CI:0.54-1.23,P= 0.338;I2= 70.8%,P= 0.004)(Figure 4A)or DFS(HR = 0.68,95%CI:0.41-1.11,P= 0.124;I2= 76.1%,P= 0.041)(Figure 4B)of osteosarcoma patients(Table 2).
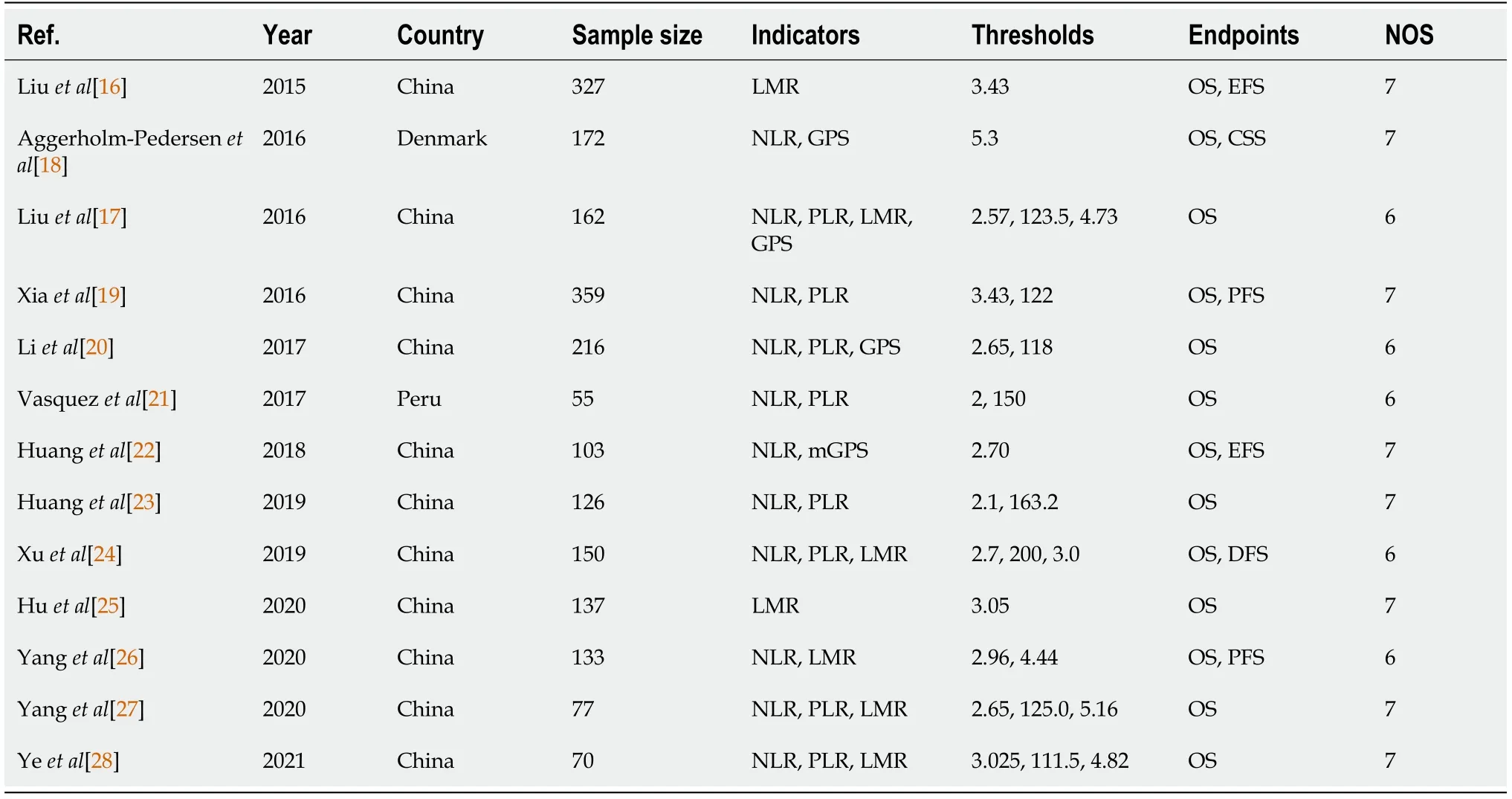
Table 1 Basic characteristics of included studies

Table 2 Results of meta-analysis
Association between GPS and prognosis of osteosarcoma patients
Only four studies investigate the relationship of GPS with survival of osteosarcoma patients[17,18,20,22].The pooled results certified that GPS was a novel predictor for OS(HR = 2.19,95%CI:1.64-2.94,P<0.001;I2= 0.0%,P= 0.602)(Figure 5A)and DFS(HR = 2.50,95%CI:1.39-4.48,P< 0.001;I2= 0.0%,P=0.342)(Figure 5B)of osteosarcoma patients(Table 2).

Figure 1 The flow diagram of this meta-analysis.1PubMed(n = 22),EMBASE(n = 26),Web of Science(n = 30),CNKI(n = 13).
Sensitivity analysis and publication bias analysis
The sensitivity analysis and publication bias analysis for the association between NLR and OS of osteosarcoma patients were performed.The sensitivity analysis indicated that the pooled results were stable and reliable(Figure 6).Furthermore,the Begg’s funnel plot was asymmetric(Figure 7A)and thePvalue of Egger’s test was < 0.001,which indicated significant publication bias.Then the nonparametric trim-and-fill method was used and six potentially unpublished papers were found(Figure 7B).After combining these six publications,the pooled HRs for the fixed effect model and random effect model were 1.137(95%CI:1.036-1.247,P= 0.007)and 1.255(95%CI:0.952-1.654,P= 0.107),which indicated that the potentially unpublished studies might have a significant impact on the pooled results.Thus,more prospective studies with high-quality are still needed to verify our findings.
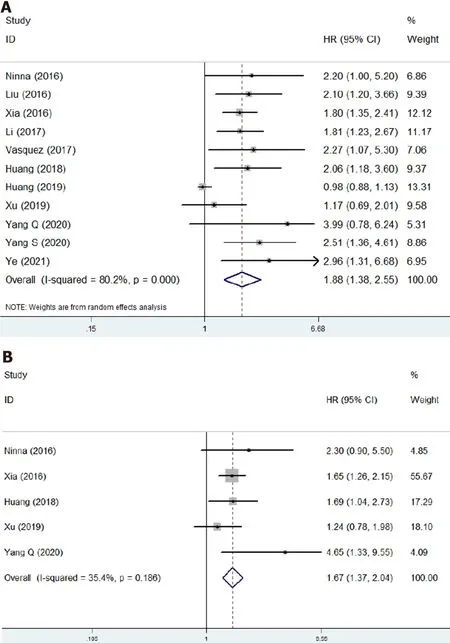
Figure 2 The association of neutrophil to lymphocyte ratio with prognosis of osteosarcoma patients.A:The association of neutrophil to lymphocyte ratio with overall survival of osteosarcoma patients;B:The association of neutrophil to lymphocyte ratio with disease-free survival of osteosarcoma patients.CI:Confidence interval;HR:Hazard ratio.
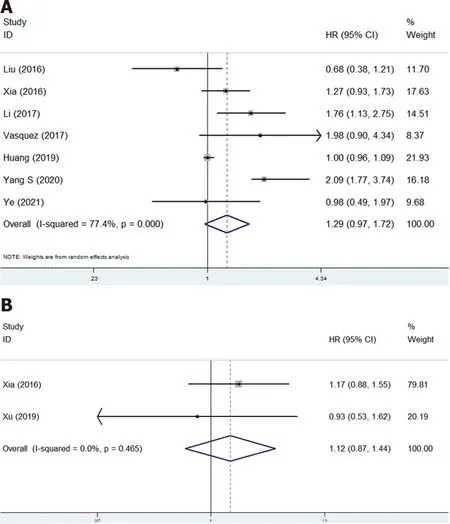
Figure 3 The association of platelet to lymphocyte ratio with prognosis of osteosarcoma patients.A:Overall survival;B:Disease-free survival.CI:Confidence interval;HR:Hazard ratio.

Figure 4 The association of lymphocyte to monocyte ratio with prognosis of osteosarcoma patients.A:The association of lymphocyte to monocyte ratio with overall survival of osteosarcoma patients;B:The association of lymphocyte to monocyte ratio with disease-free survival of osteosarcoma patients.CI:Confidence interval;HR:Hazard ratio.
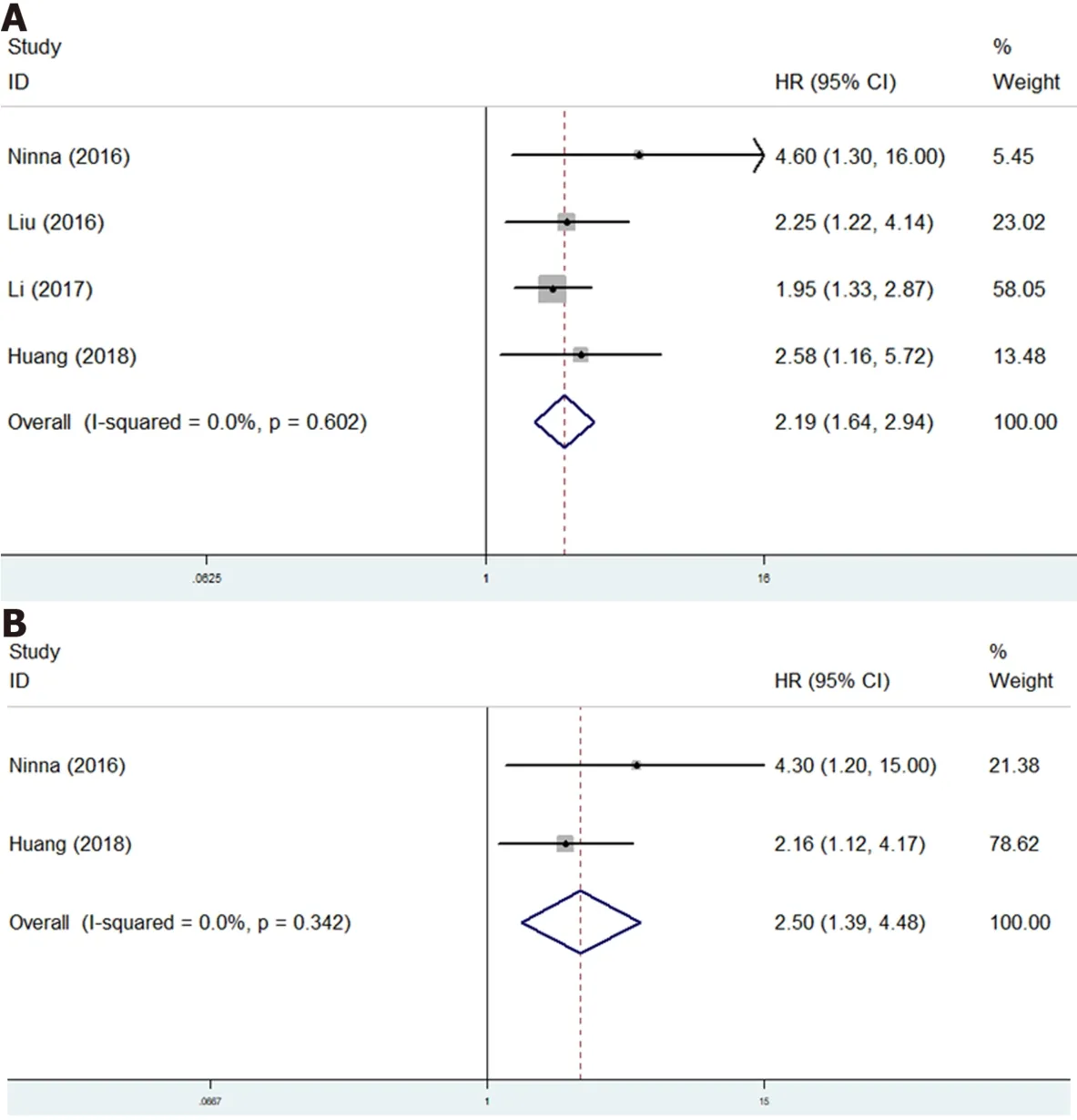
Figure 5 The association of Glasgow prognostic score with prognosis of osteosarcoma patients.A:The association of Glasgow prognostic score with overall survival of osteosarcoma patients;B:The association of Glasgow prognostic score with disease-free survival of osteosarcoma patients.CI:Confidence interval;HR:Hazard ratio.

Figure 6 Sensitivity analysis about the association of neutrophil to lymphocyte ratio with overall survival of osteosarcoma patients.CI:Confidence interval.

Figure 7 Begg’s analysis.A:Begg’s funnel plot;B:Trimed Begg’s funnel plot.
DlSCUSSlON
The current study demonstrated that higher NLR and GPS were independent prognostic risk factors for poorer OS and DFS of osteosarcoma patients,but no significant association of PLR and LMR with prognosis in osteosarcoma was identified.However,obvious publication bias was observed in this meta-analysis and more prospective high-quality studies are still needed to verify above findings.
It has been widely known that the systematic inflammation response is closely related with the occurrence and development of tumors.The detailed internal mechanisms have been deeply explored and introduced in previous literatures[8,33-35].The neutrophils,lymphocytes,platelets,monocytes and C-reactive protein are all common inflammatory biomarkers and a great number of studies have revealed the prognostic role of NLR,PLR,LMR and GPS in tumors.Several met-analyses demonstrated that elevated pretreatment NLR was a prognostic risk factor in colorectal cancer(HR = 1.57,95%CI:1.39-1.78,P< 0.001)[36],gastric cancer(HR = 1.78,95%CI:1.59-1.99,P< 0.001)[37],laryngeal cancer(HR =1.76,95%CI:1.53-2.03,P< 0.001)[38]and non-small cell lung cancer patients(HR = 2.86,95%CI:2.11-3.87,P< 0.001)[39].Furthermore,the prognostic value of GPS has been verified in ovarian cancer(HR =1.62,95%CI:1.38-1.91,P< 0.001),esophageal squamous cell cancer(HR = 1.66,95%CI:1.14-2.41,P=0.008),colorectal cancer(HR = 2.20,95%CI:1.88-2.57,P< 0.001)and lung cancer patients(HR = 2.058,95%CI:1.51-2.80,P< 0.05)by several meta-analyses[14,40-42].Similarly,the PLR and LMR have also been reported to show high prognostic value in cancer patients by some studies with high-quality evidence[33,43-47].However,whether the NLR,PLR,LMR and GPS could serve as valuable predictors for long-term survival in osteosarcoma remained unclear.Thus,we conducted the current meta-analysis and revealed the high prognostic value of NLR and GPS in osteosarcoma patients.
In our study,the LMR was not statistically related with prognosis of osteosarcoma patients.However,among the six included studies,two of them reported significantly positive association of lower LMR with poorer OS[16,28].Remarkably,Yanget al[27]seemed to report conflicting results.According to the Kaplan-Meier survival curve,patients with lower LMR had poorer OS than patients with higher LMR did;however,the univariate analysis indicated that higher LMR was a risk factor for worse OS[27].After excluding this study,the pooled HR was 0.69(95%CI:0.55-0.87,P= 0.002)by combining the remaining studies.Thus,we deem that LMR is also a valuable prognostic indicator in osteosarcoma patients,but more relevant studies are needed to further verify this.
Actually,we suppose that there are still some fields worth further investigation.Although we identified the prognostic role of these indexes,a comparison of their prognostic values was not conducted and it is not clear whether a combination of them would show higher predictive role for prognosis in osteosarcoma patients.Whether these indicators could predict the therapeutic effects of neoadjuvant or adjuvant chemotherapy is unclear.Besides,we deem that these blood parameters might play a role in the diagnosis of osteosarcoma or its recurrence.Based on our findings,we suggested that the NLR and GPS should be considered for the assessment of disease status and formulation of therapy strategies and osteosarcoma patients with higher pretreatment NLR or GPS might receive more aggressive treatment and follow-up.Besides,it is worth exploring whether anti-inflammation treatment,reducing the NLR and GPS,is beneficial for osteosarcoma patients with high NLR or GPS.
There are several limitations in this meta-analysis.First,all included studies are retrospective with relatively small sample size,which might cause some bias.Second,most studies are from China,which limits the application of our results in other regions or countries.Third,subgroup analyses based on some important parameters such as the disease stage,age and treatment were not able to performed due to lack of relevant data.
CONCLUSlON
In overall,higher NLR and GPS were related with worse prognosis and might serve as valuable prognostic indicators for osteosarcoma patients.However,more prospective high-quality studies are still needed to verify our findings.
ARTlCLE HlGHLlGHTS
Research background
Previous researches explored the prognostic role of the neutrophil/lymphocyte ratio(NLR),platelet/lymphocyte ratio(PLR),lymphocyte/monocyte ratio(LMR)and Glasgow prognostic score(GPS)in osteosarcoma,but their results were inconsistent with each other.
Research motivation
To verify the prognostic value of these blood indexes in osteosarcoma patients.
Research objectives
To verify the prognostic value of these blood indexes in osteosarcoma patients.
Research methods
Several electronic databases were searched to identify relevant articles.The hazard ratio(HR)with 95%confidence interval(CI)was combined to the evaluate the association between these indicators and overall survival(OS)and disease-free survival(DFS).
Research results
Higher NLR and GPS were significantly associated with poorer OS(P< 0.001;P< 0.001)and DFS(P<0.001;P< 0.001).However,no significant relationship of PLR and LMR and OS(P= 0.085;P= 0.338)and DFS(P= 0.396;P= 0.124)was observed.
Research conclusions
Higher NLR and GPS were related with worse prognosis in osteosarcoma.
Research perspectives
The NLR and GPS might serve as reliable and valuable prognostic indicators for osteosarcoma patients.
FOOTNOTES
Author contributions:Li XF made the substantial contributions to the conception and design of the work;Peng LP and Li J searched,selected materials and extracted data;Peng LP wrote this manuscript;Li J and Li XF revised the paper carefully and also contributed to the statistical analysis;all authors have read and approved the final manuscript.
Conflict-of-interest statement:The authors declared no potential conflicts of interest with respect to the research,authorship,and/or publication of this article.
PRlSMA 2009 Checklist statement:This systematic review and meta-analysis were conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial(CC BYNC 4.0)license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See:https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORClD number:Peng-Peng Li 0000-0003-1922-0153;Jie Li 0000-0002-6178-4377;Xian-Feng Li 0000-0003-3469-3143.
S-Editor:Ma YJ
L-Editor:A
P-Editor:Ma YJ
 World Journal of Clinical Cases2022年7期
World Journal of Clinical Cases2022年7期
- World Journal of Clinical Cases的其它文章
- Relationship between treatment types and blood-brain barrier disruption in patients with acute ischemic stroke:Two case reports
- Ultrasound-guided rectus sheath block for anterior cutaneous nerve entrapment syndrome after laparoscopic surgery:A case report
- Spontaneous dissection of proximal left main coronary artery in a healthy adolescent presenting with syncope:A case report
- Acute esophageal obstruction after ingestion of psyllium seed husk powder:A case report
- Novel mutations of the Alstr?m syndrome 1 gene in an infant with dilated cardiomyopathy:A case report
- Cutaneous leishmaniasis presenting with painless ulcer on the right forearm:A case report
