Direct antiglobulin test-negative autoimmune hemolytic anemia in a patient with β-thalassemia minor during pregnancy:A case report
INTRODUCTION
As an autosomal inherited hemoglobin (Hb) disorder,due to the absence or reduced synthesis of the globin chains of Hb,thalassemia has two main types,α-and βthalassemia.Over 300 types ofgene mutations have been reported causing varying degrees of reduced β-globin synthesis,usually categorized as minor,intermedia,or major on the basis of their clinical manifestations and dependence on blood transfusion[1].China has a high prevalence of thalassemia,especially in the south of the Yangtze River.From epidemiological data,the thalassemia carrier population in China is over 30 million,among which over 1% has the major or intermedia type[2].Patients with asymptomatic β-thalassemia minor,also known as silent carriers,who have mild microcytic,hypochromic anemia or even a normal Hb level,usually require little medical care.
Pregnancy complications are considered uncommon among β-thalassemia minor patients[3].Aside from accurate and timely antenatal counseling,β-thalassemia minor patients do not require more frequent antenatal check-ups than normal,as this type of anemia during pregnancy rarely progresses to a serious condition that can cause significant adverse effects with a high risk of maternal mortality.
We report the case of a 30-year-old multipara with β-thalassemia minor who experienced severe hemolytic anemia throughout pregnancy.Fortunately,the maternal and fetal outcome was favorable following diagnosis and treatment.To our knowledge,this is the first report of such a case.
CASE PRESENTATION
Chief complaints
A 30-year-old woman,gravida 2 para 1,presented with fatigue,chest tightness,and shortness of breath for over 1 mo after activities at the 17-wk gestation.
History of present illness
The patient was diagnosed with severe anemia at a local hospital.Her Hb level was 40 g/L and she had several blood transfusions,but her Hb did not increase as expected and began to drop when the transfusion stopped.
And all this while his sister was pacing up and down the palace, hardly letting the knife out of her hand, and dreading18 what she knew she would see, and what she did see
It was the end of my exhausting first day as a waitress in a busy New York restaurant. My cap had gone awry1(,), my apron2() was stained, my feet ached. The loaded trays I carried felt heavier and heavier. Weary and discouraged, I didn t seem able to do anything right. As I made out a complicated check for a family with several children who had changed their ice-cream order a dozen times, I was ready to quit.
History of past illness
Signs of anemia had not been taken seriously until the patient was hospitalized for pleuritis in 2019,when she was found to be an IVS-II-654(C>T) carrier.Her husband is not a carrier of thalassemia trait.Special medication history (other than Vitamin Complex Tablets) and transfusion history before this pregnancy were denied.
51. Perish miserably: Burning occurs often in fairy tales. It is symbolic120 of purification (Matthews 1986). The witch being burnt can also represent evil destroying itself (Luthi 1976).
Personal and family history
No contributory personal history or similar family history.
Physical examination
DAT-negative autoimmune hemolytic anemia (AIHA) during pregnancy.
Laboratory examinations
According to the patient’s test results,the presence of intravascular hemolysis was basically established;however,the gene sequencing did not match thalassemia major.Erythrocyte CD55 and CD59 should be analyzed to rule out paroxysmal nocturnal hemoglobinuria.
Imaging examinations
Abdominal ultrasound showed a spleen diameter of 68 mm.Echocardiography demonstrated a left atrial diameter of 40 mm and mild mitral,tricuspid,and aortic regurgitation.
Further diagnostic work-up
The evidence for connective tissue disease was insufficient.
His hair stood on end, and he wore a huge bag- purse and a cravat91 tied in a bow, his mantle was made of a shower of silver coins with a lining92 of rose colour, and his delight in his own appearance knew no bounds
MULTIDISCIPLINARY EXPERT CONSULTATION
Ming-Yang Deng,MD,PhD,Assistant Professor,Department of Hematopathology,The Second Xiangya Hospital,Central South University
The patient was referred to our hospital at the 25-wk gestation.Laboratory investigations showed severe anemia,with an Hb level of 39 g/L,mean corpuscular Hb of 22.5 pg,mean corpuscular volume of 74.6 fL,and fraction of Hb A2 of 4.7%,as well as a raised bilirubin level of 34.8 μmol/L,direct bilirubin level of 15.9 μmol/L,raised lactate dehydrogenase (LDH) level of 392.5 U/L,reticulocyte count of 3.15%,and haptoglobin below the detection limit.The ferritin level was 291.57 ng/mL,and B12 and folate levels were normal.Oral glucose tolerance test and other routine prenatal blood test results were within the normal range.We performed TORCH (comprising toxoplasmosis,,rubella,cytomegalovirus,herpes virus,and hepatitis viruses) serology to rule out preceding infection.Signs of intravascular hemolysis that could not be ascribed to β-thalassemia minor were observed.
Jing Tian,MD,PhD,Assistant Professor,Department of Rheumatology and Immunology,The Second Xiangya Hospital,Central South University
We carried out a multidisciplinary consultation on the third day after the patient’s admission.Taking expert opinions from a hematologist and rheumatologist,we performed further examinations.Bone marrow cytology suggested active proliferation of erythrocytes.Flow cytometry showed normal erythrocyte levels of CD55 and CD59.Connective tissue screening including antinuclear antibody and extractable nuclear antigen was also negative.A normal complement C3 level and slightly decreased C4 level were detected.We performed the direct antiglobulin test (DAT;also referred to as the "Coombs" test) including IgG and C3 several times;however,the results were negative.According to the principle of exclusion,the patient’s severe hemolytic anemia could be due to autoimmune reasons.On the other hand,the patient’s intermediate Down's screening indicated a high risk of trisomy 21;thus,a prenatal diagnosis was performed.The karyotype of the fetus was normal and copy number variation-sequencing did not find any disease-causing gene mutations.
FINAL DIAGNOSIS
The patient’s vital signs were normal.She had a pale appearance,her uterus size matched the gestational age,and fetal heart rate was normal.
The prince did all as he was told, then they took flight; they crossed the seven seas, and at each one the prince fed the Simurgh When they alighted on the shore of the last sea, it said: O my son! there lies your road; follow it to the city
TREATMENT
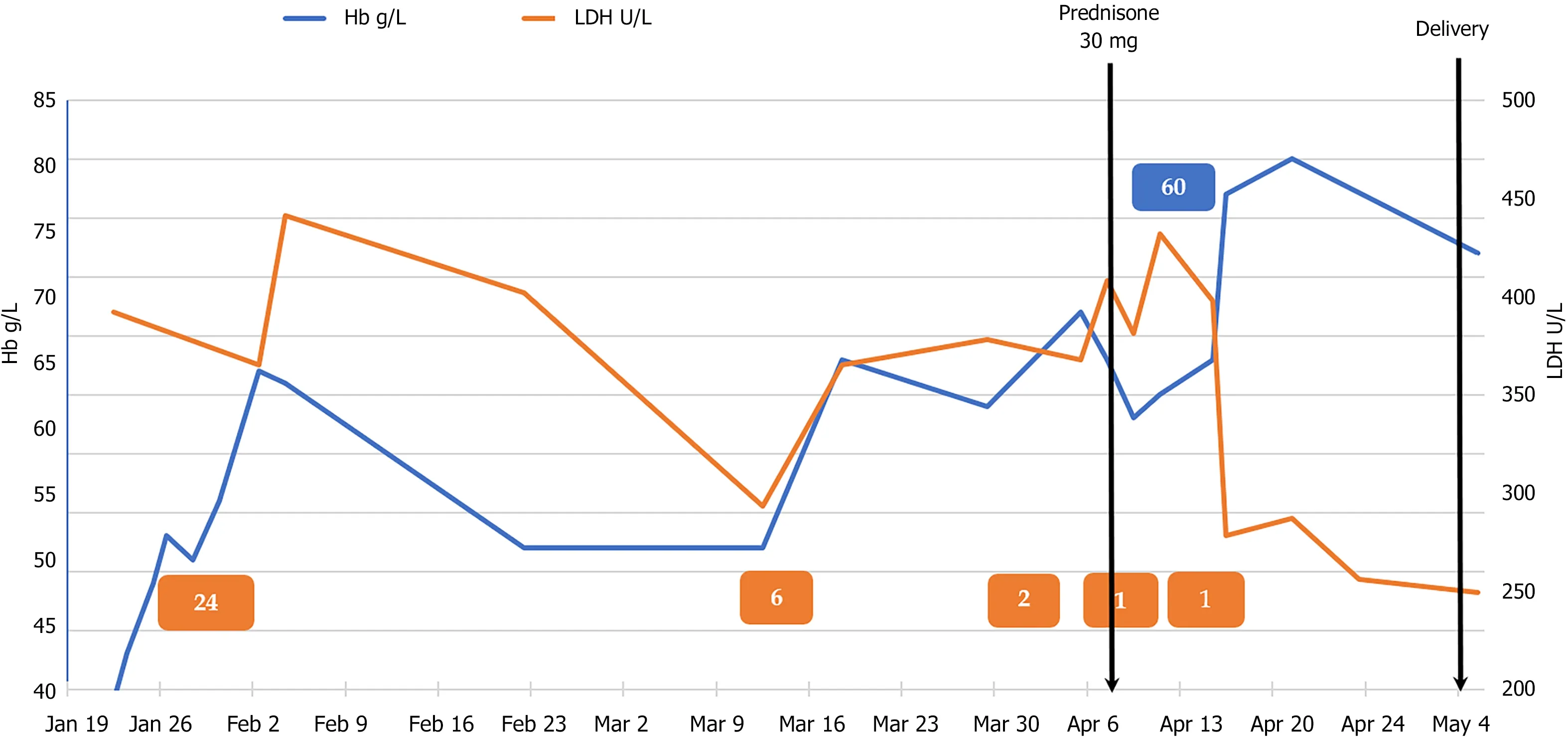
The patient was given red blood cell (RBC) transfusions with other symptomatic and supportive treatment,and the growth parameters and middle cerebral artery peak systolic velocity (MCA-PSV) of the fetus were monitored.Fortunately,fetal growth and development matched the gestational age and the MCA-PSV did not increase.The patient was discharged 2 wk later and underwent strict follow-up.She returned to her hometown for 1 mo,and at the 31-wk gestation,she underwent echocardiographic reexamination at the local hospital,which showed an atrial septal aneurysm 35 mm × 14 mm in size,indicating anemic cardiomyopathy.She was admitted to our hospital for the second time.Her blood tests still suggested severe hemolytic anemia,but this time we were very cautious regarding blood transfusion in order to avoid heart overload.We suspected that the hemolysis was due to autoimmune factors,and after discussions with the patient and her family,she was given corticosteroid and immunoglobulin therapy.She received prednisone 30 mg orally qd and intravenous immunoglobulin (IVIG) 20 g/d for 3 d.Her Hb level rose to>80 g/L.The patient’s Hb and LDH values throughout pregnancy in relation to medication administration and RBC transfusion are shown in Figure 1.At 38+wk gestation,she was given vaginal misoprostol to induce labor,following echocardiography which found no abnormalities.
OUTCOME AND FOLLOW-UP
A live 3255-g boy was born by normal vaginal delivery.The neonate was transferred to the Neonatology Department 35 h after birth due to hyperbilirubinemia.Blood test results showed no sign of hemolysis;however,Hb was 136 g/L,white blood cell count was 9.07 × 10/L,platelet count was 314 × 10/L,and inflammatory indicators were elevated,indicating neonatal infection,and he had inherited the same IVS-II-654(C>T) mutation from his mother.The neonate was discharged after antibiotic treatment and phototherapy 10 d later.The mother discontinued oral corticosteroid postnatally,and maintained an Hb level above 90 g/L.
DISCUSSION
β-thalassemia carriers are asymptomatic;however,little research is available on the pregnancy outcome of β-thalassemia carriers,although it has been reported that the incidence of intrauterine growth retardation and oligohydramnios is higher[3-5].It is recommended that pregnant women with mild thalassemia should follow the health care guidelines for normal pregnancy[6].Thalassemia carriers tend to become more anemic during pregnancy,and it is commonly believed that this is due to physiological hemodilution[3].It has been reported that only 3% of pregnant β-thalassemia carriers have an Hb level lower than 80 g/L,which can be associated with maternal clinical symptoms of anemia and adverse neonatal outcomes[3].In this case,hemoglobinopathy itself might be a cause of hemolysis anemia,but it is difficult to ascribe severe and acute hemolytic anemia to simply β-thalassemia minor.
Rich and prospering16 in every respect, he said; the woman isbrave and good, but you are in my heart. I have fought the battle,it will soon be ended; we shall not see each other again now untilwe meet before God!
AIHA is characterized by the production of RBC autoantibodies,accelerating their destruction[7].The incidence of AIHA in the general population is 1/100.000[8].AIHA is rare during pregnancy,and the exact incidence has not been reported[9,10].It has been reported that ovarian teratomas were suggested as a possible trigger of AIHA in pregnant and non-pregnant patients[11].The diagnosis is generally based on the presence of anemia along with signs of hemolysis such as reticulocytosis,low haptoglobin,increased LDH,elevated indirect bilirubin,and a positive DAT.DATnegative AIHA,as in our patient,only occurs in 5%-10% of all cases,and requires more specific detection with new diagnostic tools[7,9].Due to insufficient knowledge and conditions,we did not perform a more sensitive DAT test such as anti-IgA and IgM antisera[12],and there is still room for improvement in this area.The prognosis is usually favorable once an accurate diagnosis of AIHA has been made,patients usually respond to first-line corticosteroids,and AIHA resolves after delivery[13].Other treatments include RBC transfusions and IVIG.It was reported that cyclosporine A was safe and effective in a case of β-thalassemia major,AIHA,and insulin treated diabetes mellitus when first-line corticosteroids were unsuitable[14].Research focused on AIHA in patients with thalassemia is very limited.Available reports are usually on alloimmunization in thalassemia major patients after receiving multiple blood transfusions.A multicenter study showed that erythrocyte autoantibodies occurred in 6.5% of chronically or intermittently transfused thalassemia patients[15].As reported,the presence of underlying RBC autoantibodies may be predictors of AIHA in βthalassemia patients[16].Our thalassemia patient was not transfusion dependent,and as pregnancy is a semi-allogeneic process,we thought that there might be potential links between these three pathological processes.
CONCLUSION
We report a rare case of severe refractory anemia during pregnancy.Following various examinations,the underlying cause of the anemia was finally identified,and the patient received timely treatment.Very little research has been carried out on AIHA in pregnant patients with thalassemia.Little is known about possible pathologic process and ignoring it can lead to delays in treatment and adverse pregnancy outcome.We suggested that DAT-negative AIHA should be suspected in cases of severe hemolytic anemia in pregnant patients with and without other hematological diseases.Hopefully,there will be more detailed and in-depth studies carried out on this issue in the future.
Special thanks to the nurses and physicians for their care of this patient.
 World Journal of Clinical Cases2022年4期
World Journal of Clinical Cases2022年4期
- World Journal of Clinical Cases的其它文章
- Surgical treatment of acute cholecystitis in patients with confirmed COVID-19:Ten case reports and review of literature
- Rituximab as a treatment for human immunodeficiency virusassociated nemaline myopathy:What does the literature have to tell us?
- Eustachian tube involvement in a patient with relapsing polychondritis detected by magnetic resonance imaging:A case report
- Endoscopic clipping for the secondary prophylaxis of bleeding gastric varices in a patient with cirrhosis:A case report
- Inflammatory myofibroblastic tumor after breast prosthesis:A case report and literature review
- Langerhans cell histiocytosis presenting as an isolated brain tumour:A case report
