Rectangular 3-snip punctoplasty versus punch punctoplasty with silicone intubation for acquired external punctal stenosis: a prospective randomized comparative study
Xin Cao, Zi-Zhong Hu, Ying Wu, Yu Song, Qing-Huai Liu
1Department of Ophthalmology, the First Affiliated Hospital of Nanjing Medical University, Nanjing 210029, Jiangsu Province, China
2Department of Ophthalmology, the Second Affiliated Hospital of Nantong University, Nantong 226000, Jiangsu Province,China
Abstract
● KEYWORDS: acquired external punctal stenosis;punctoplasty; Kelly punch
INTRODUCTION
Acquired external punctal stenosis (AEPS) is a common disorder with clinical manifestations such as epiphora.It can be caused by a toxic effect of topical or systemic medications, various infections, lid malposition, or different forms of trauma and tumors[1]. Until now, there has been no acceptable guidelines for the management of AEPS. Attempts to resolve the stenosis has been reported as a 1‐snip, 2‐snip,3‐snip or 4‐snip procedure, punctal dilatation (with or without mitomycin‐C), perforated punctal plugs, Mini‐Monoka, and self‐retaining bicanalicular stents[2‐10]. However, how to reduce the surgical injury and improve the success rate of operation remains controversial. The rectangular 3‐snip procedure is believed to be better than the triangular variant in preventing restenosis and preserving the lacrimal pump mechanisms[11]. As an innovative procedure, Hughes and Maris[12]first performed posterior ampullectomy using a punch in 1967. Later, Edelsteinet al[13]and Carrimet al[14]reported punctoplasty with an available punch. They all think that punch punctoplasty is a convenient and effective way to resolve AEPS. However, no prospective,randomized, comparative study has been performed until now.In this study, we aimed to investigate that whether punctoplastyviaKelly punch with silicone intubation has better outcomes than rectangular 3‐snip punctoplasty for AEPS.
SUBJECTS AND METHODS
Ethical ApprovalThis prospective, randomized, comparativestudy was conducted with the approval from the institutional review board and ethics committee of the Second Affiliated Hospital of Nantong University in Jiangsu, China. And it was performed in adherence with the tenets of the Declaration of Helsinki. Informed consent was obtained from each patient before enrollment.
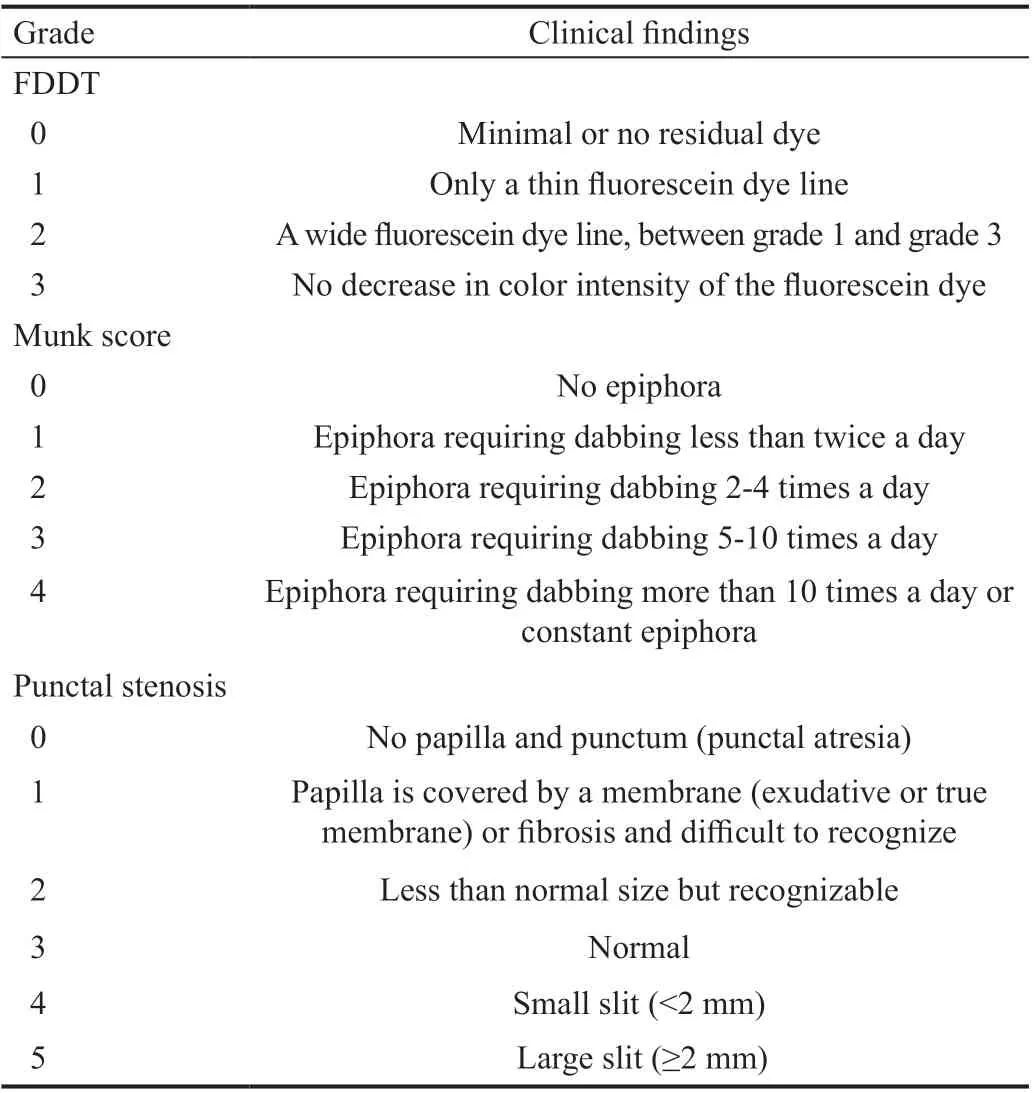
Table 1 Grading of epiphora according to Munk score, punctal stenosis according to Kashkouli’s grading system and fluorescein dye disappearance time test
Subjects and ExaminationsParticipants with AEPS grades 0 and 1 (according to Kashkouli’s grading system[1]) affecting the lower punctum were recruited from the Ophthalmology Department of the Second Affiliated Hospital of Nantong University from June, 2016 to June, 2019. Patients with associated dry eye, nasolacrimal duct obstructions, congenital punctal disorders, canalicular obstructions, dacryocystitis,untreated blepharitis, eyelid malpositions, and prior trauma or interventions were excluded. The participants were randomly divided into 2 groups based on the intervention: group A received rectangular 3‐snip punctoplasty, while group B underwent punctoplastyviaKelly punch with RS silicone intubation (Runshi Medical Equipment Co., Jinan, China). The silicone tube remained in place for 3mo before it was removed.All patients were followed up for at least 12mo.
At every follow‐up point, each case’s symptoms were graded according to Munk score (Table 1)[2]. Punctal stenosis was detected on slit‐lamp examination, and we categorized the severity of punctal stenosis according to Kashkouli’s grading system (Table 1)[1]. We also performed a fluorescein dye disappearance time test (FDDT), and improved our grading system according to the Zappia score (Table 1)[15]. A drop of 2% fluorescein was instilled in the conjunctival sac and on the sclera and observed at the end of five minutes and graded in terms of color intensity. Furthermore, we measured the lower tear meniscus height (TMH) using a Keratograph 5M ocular surface analyzer (Oculus, Germany). Subjects sitted in front of the detector and gazed the central point of the device, and the image was obtained under the TMH measurement mode. The TMH was measured by the random software caliper tool below the center of the cornea. Patients were examined three times at 5min intervals to calculate an average of the TMH.
At the last follow‐up, we evaluated the clinical therapeutic effect. The judging criteria were as follows: 1) anatomical success: Kashkouli score of the opening of the inferior lacrimal punctum was kept above 1; 2) functional success:Munk score was 0 or 1 and FDDT graded 0 or 1; 3) functional improvement: Munk score was 2, FDDT graded 0, 1 or 2; 4)treatment failure: persistent point stenosis (graded 0 or 1) or/and Munk score greater than 2, FDDT was 3.
Surgical TechniqueAll the surgical procedures were performed by a same experienced surgeon (Wu Y). Group A received a rectangular 3‐snip punctoplasty. In total, 1 mL of 2% lidocaine mixed with epinephrine (1:200 000) was injected locally around the puncta after instillation of topical anesthesia(0.4% oxybuprocaine, eyedrops, Santen Pharmaceutical Co., Japan). Dilatation of the stenosed puncta was carefully performed with a dilator, and then the posterior wall of the ampulla was grasped with toothed microforceps. An excision of the posterior wall of the ampulla was performed with Vannas scissors as follows: the first 2 downward at either side of the vertical canaliculus and the third across the bottom.There was no remarkable bleeding observed in each patient.The lacrimal passages were rinsed with normal saline to ensure the patency of the naso‐lacrimal duct.
The eyes of group B underwent the surgical interventions as follows. After anesthesia of the anterior ethmoid nerve and infraorbital nerve, membranes over the punctum were perforated with a 25/27‐G needle as needed. The opening of the punctum was enlarged circumferentially with a dilator. A Kelly punch with a 0.8 mm diameter head was then inserted into the canaliculi at approximately 2 mm depth, and then bite off the membrane covering the punctum to achieve enlargement of the punctal opening toward the conjunctival surface. A new RS silicon tube (Runshi Medical Equipment Co., Jinan, China) was inserted through the upper and lower puncta of each eye into the nasolacrimal duct. The metal guide probe in the silicone tube was pulled out, and the other end of the RS lacrimal duct was placed into the lacrimal duct through the superior lacrimal canaliculus in the same way, and the final depth is that the blue mark point is located in the middle of the upper and lower lacrimal punctum. Syringing and probingwere performed at the end of surgery, in order to confirm the patency of the lacrimal drainage system. The tube was removed 3mo after the operation.
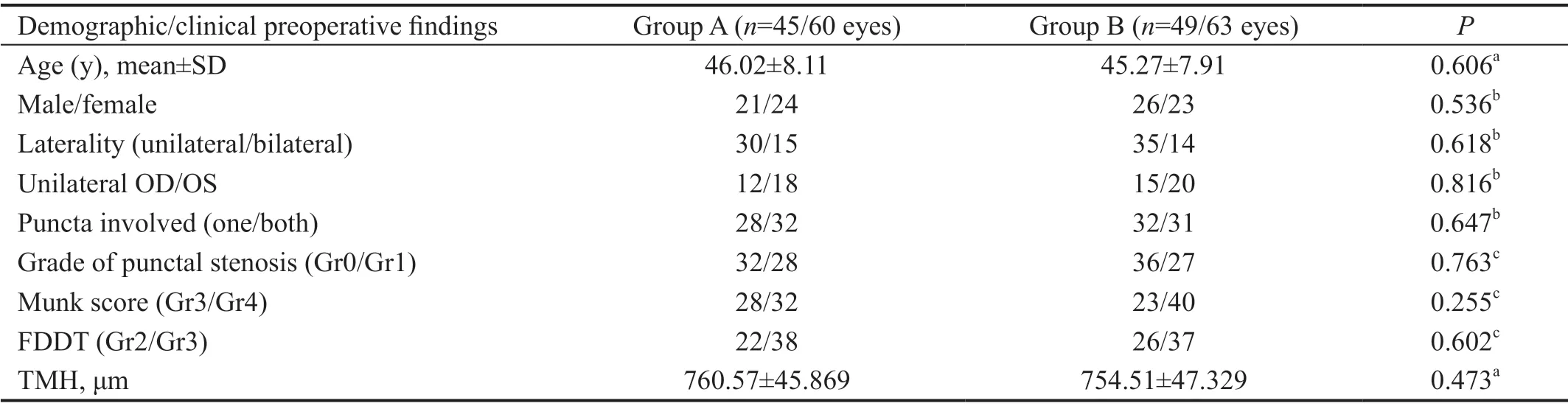
Table 2 Demographic and clinical preoperative data
Postoperatively, all subjects received steroid and antibiotic eyedrops (0.1% fluorometholone and 0.5% levofloxacin eyedrops, Santen Pharmaceutical Co., Japan) six times a day and were reduced within 3‐5wk depending on the postoperative inflammation. All participants were followed up for at least 12mo. During the follow‐ups, the epiphora severity assessment,FDDT, TMH, and punctal stenosis severity assessment were assessed for all patients using the same scoring systems.
Statistical AnalysisStatistical analysis was done using SPSS version 19.0 (IBM Corporation, Armonk, NY, USA). Normally distributed continuous data was compared using the Student’st‐test while distribution was compared using Mann‐Whitney test, and Chi‐square test were used to compare categorical variables. APvalue of <0.05 was considered statistically significant.
RESULTS
In the current study, 123 eyes of 94 patients were included,with 60 eyes in group A and 63 eyes in group B. No significant differences between the groups were detected in baseline clinical characteristics concerning age, gender, eye laterality,unilateral OD/OS, puncta involved, preoperative grade of punctal stenosis, Munk score, FDDT and TMH (Table 2).
After surgery, the FDDT were significantly decreased in both groups at 6 and 12mo compared with their baseline(allP<0.05,Table 3). The grade of punctal stenosis was significantly increased after 6 and 12mo in both groups (allP<0.05, Table 3). After 6 and 12mo, the FDDT of group B is lower than that of group A (P=0.01, 6mo;P=0.012, 12mo; Table 3).The grade of punctal stenosis of group B is higher than that of group A (bothP<0.001; Table 3). Although there was no difference in the FDDT between 6 and 12mo after surgery in each group (P=0.517, 0.854; Table 3), the grade of punctal stenosis between 6 and 12mo after surgery is of statistical significance in each group (P=0.001,<0.001; Table 3).
After 6 and 12mo, the Munk score of group B is lower than that of group A (P=0.001, 6mo;P=0.004, 12mo; Table 3). The TMH of group B is also lower than that of group A (P=0.001,6mo;P=0.002, 12mo; Table 3). There was no difference in the Munk score and the TMH between 6 and 12mo after surgery in each group (Table 3). There was a positive correlation between TMH and Munk score at 6mo after surgery (R=0.616,P<0.001; Figure 1) and 12mo after surgery (R=0.655,P<0.001; Figure 1). No complication such as infection or displacement of tube in group B within 3mo.
Despite the anatomical success was similar in both group(96.7% in group A and 98.4% in group B,P=0.613; Table 4),the functional success was higher in group B than that in group A (65.1%vs46.7%,P=0.047; Table 4). Treatment failure is lower in group B than that of group A (7.9%vs23.3%,P=0.024; Table 4).
DISCUSSION
The current study showed that punctoplastyviaKelly punch with RS silicone intubation provides better outcomes than rectangular 3‐snip punctoplasty. Although the anatomical success between the two groups was similar, the rate of functional success of punctoplastyviathe Kelly punch group was higher than that of the rectangular 3‐snip punctoplasty group, and treatment failure was less frequent.
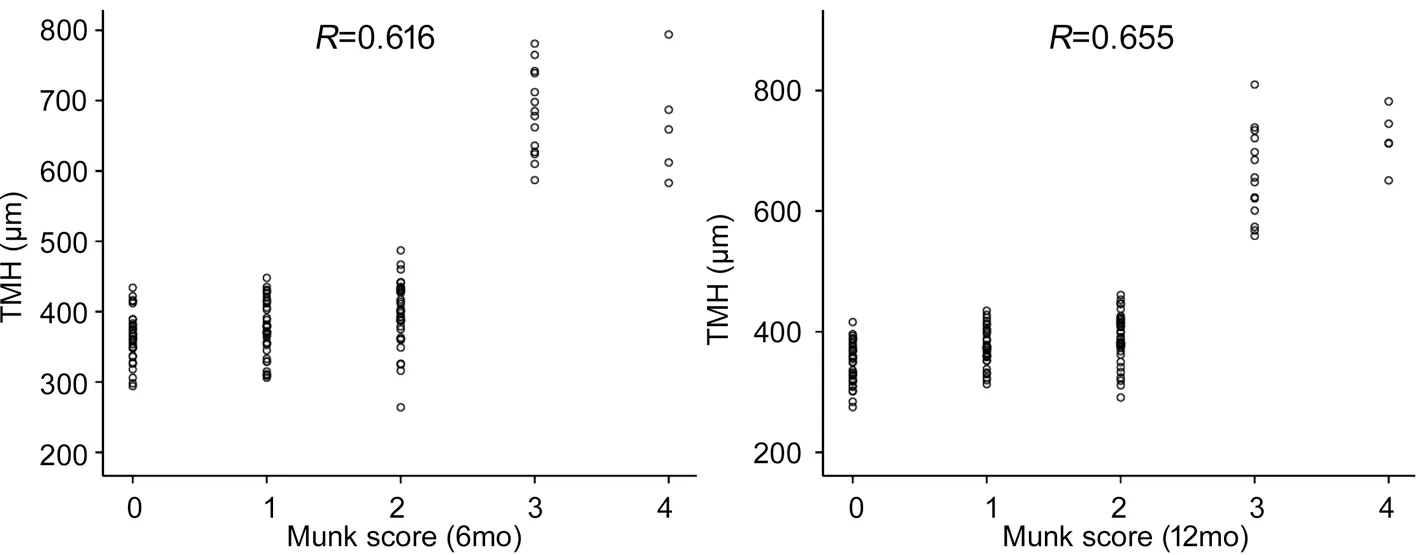
Figure 1 Scatter plots demonstrating the correlation between TMH and Munk score at 6 and 12mo postoperative follow-up points.
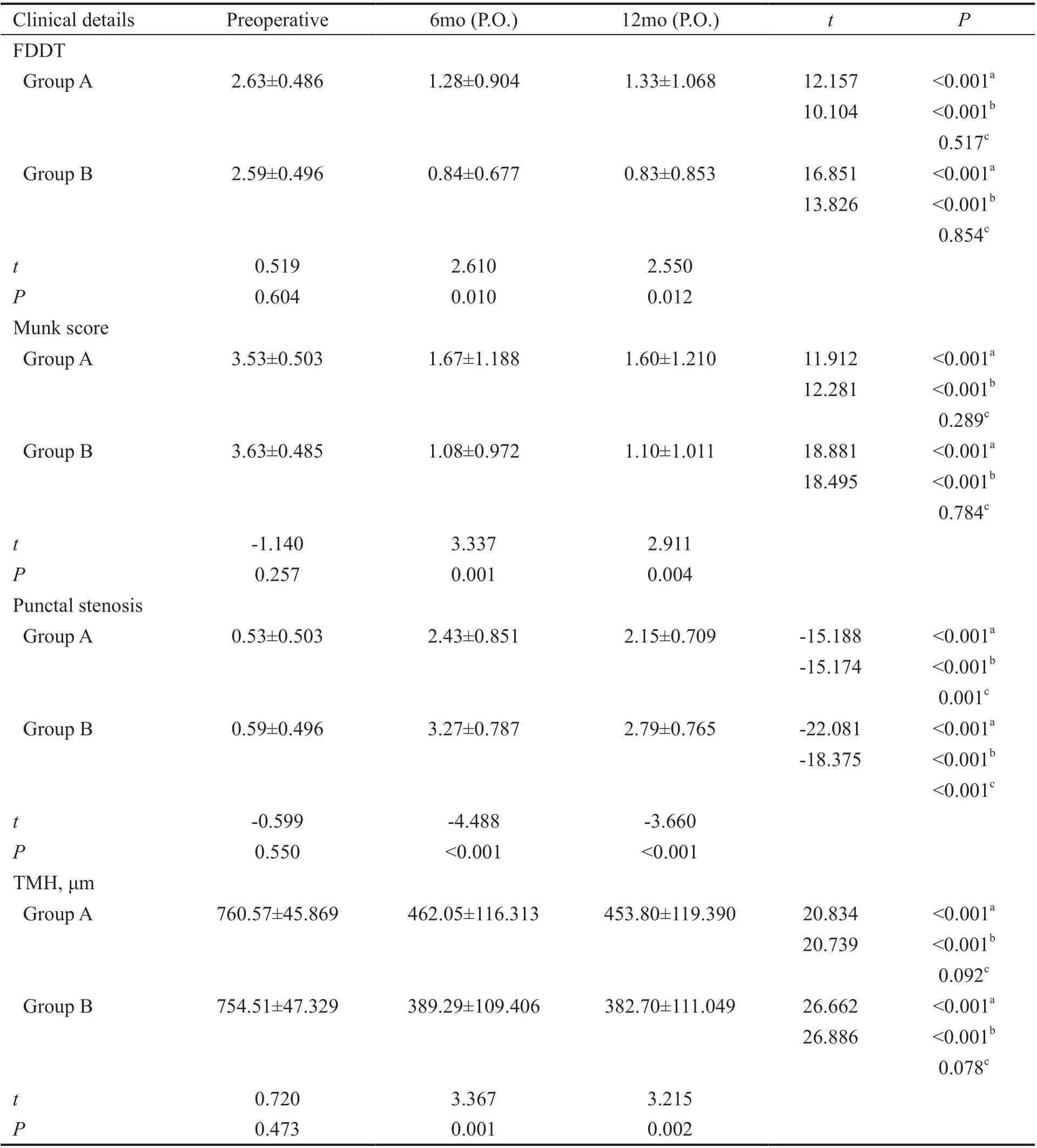
Table 3 Grade of FDDT, Munk score, grade of punctal stenosis and TMH at preoperative, 6 and 12mo postoperative follow-up points of both groups with AEPS
To treat AEPS, an appropriate functional punctum with right position to tear lakes is needed. A number of methods have been reported. One‐snip, 2‐snip, 3‐snip and 4‐snip punctoplasty procedures were subsequently introduced[16‐19], in which Thomas’s triangular 3‐snip punctoplasty was the most popular,but there were still complications such as re‐approximation of cut ends, restenosis and tear drainage system impairment.Furthermore, Chak and Irvine[11]introduced a rectangular 3‐snip punctoplasty, which is a less destructive procedure.They only excise the vertical section of the canaliculus, not the horizontal section, to preserve the normal anatomy and physiologic functioning of the lacrimal system. Aliet al[20]followed up 87 eyes, and found 82% of cases demonstrated complete resolution of symptoms postoperatively, but 10.3%of the eyes had functional epiphora and 5.3% had restenosis postpunctoplasty. In addition, perforated punctal plugs were also used subsequently in the management of punctal stenosis, most of which achieved a success rate up to 85% on average[10,21]. However, Singhet al[22]reported no significant difference between 3‐snip punctoplasty and minimally invasive intubation with Mini‐Monoka in the treatment of AEPS. In particular, a recent study showed a higher success rate of 93.3%, which is the first to use mitomycin‐C in conjunction with perforated plugs to prevent restenosis[10]. But no standardized grade system was conducted for quantification of epiphora. Subsequently, Wonget al[23]showed a nonincisional and minimally invasive procedure with Kelly punch instead of 3‐snip punctoplasty. Approximately 92% functional success rate was achieved, which was easier to perform 3rdless invasive than 3‐snip punctoplasty. However, the vertical and 2‐3 mm horizontal canaliculi are excised during punching and may destroy the function of canaliculi. The physiological role of the punctum is to maintain positive pressure during eyelid closure and negative pressure during eyelid opening within the horizontal canaliculus[24]. Any invasive surgery such as canalicular incision or ampullatectomy, will expose the canaliculi to atmospheric pressure and disrupt the normal physiological mechanism. This partly explains the reduction lacrimal system function.
In our study, we used a Kelly punch with a 0.8 mm diameter head to insert the vertical canaliculi only 2 mm deep after dilating the punctum and then bite off a full‐layer proliferative membrane covering the punctum to form a round and smooth edge of the punctum maintaining the closed lacrimal system. Every step was performed precisely under a surgical microscope. Unlike Wonget al’s[23]report, we argue that combination of the vertical lacrimal canaliculi and the horizontal canaliculi should be reserved for the normal lacrimal system. In fact, any invasive procedure will impair the function of the canaliculus. It would be more physiological protective to widen the punctum itself rather than the canaliculus tissue. Furthermore, punctoplastyviaKelly punch is simpler and easier to obtain than 3‐snip punctoplasty, and the cut edge of the punctum is much similar to the physiological and anatomical morphology. The key to success is to strictly maintain the punch depth of the vertical canaliculus, and then bite off the membrane covering the punctum with no damage to the vertical canaliculus, ampulla and the horizontal lacrimal canaliculi. In this way, a punctum similar to the normal one would be formed. However, the 3‐snip procedure destroys the vertical lacrimal canaliculi, even involves the ampulla, which is a destructive procedure that may cause a scar around the punctum. At the last follow‐up, we found that the contractionof the punctum could lead to the restenosis of lacrimal punctum in the 3‐snip group. On the other hand, the Kelly punch usually formed para round punctum with a smooth edge,which is much closer to the normal physiological structure.
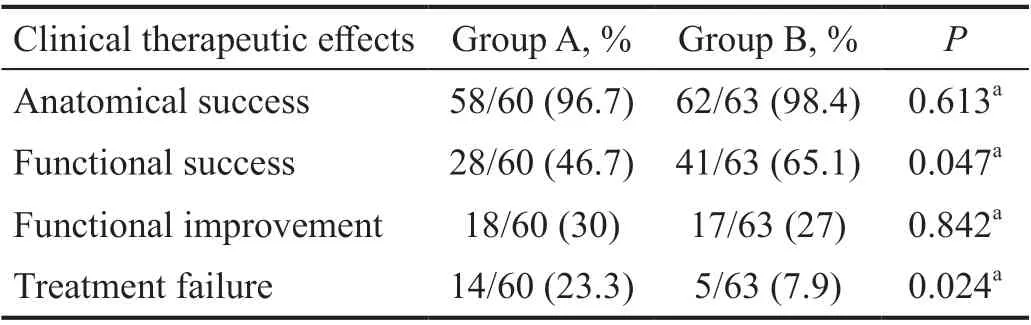
Table 4 Evaluation of clinical therapeutic effect comparison between groups at 12mo postoperatively
A new RS silicon tube was inserted through the punctum into the nasolacrimal duct in this technique. The RS tube is made of high‐purity silicone, and part of the inner canthus is designed to be slimmer and softer. First, compared with the U‐shaped silicon tube commonly used in lacrimal duct obstruction, there is no need for nasal knots or suture fixation,as it provides less stimulation to lacrimal punctum and a lower risk of lacrimal punctum cracking caused by traction. The process of the new RS intubation is simple and fast, similar to probing for nasolacrimal duct obstruction, which has no need to retrieve the tube from the nose at the area below the inferior turbinate. When taking off the tube, we hold the blue mark with a tweezer and gently pull it to the temporal side. Second,compared with punctal plugs such as Mini‐Monoka, is more easy to follow and cost‐effective, has better stability and is more suitable for continuous dilatation of the punctum, which can prevent restenosis of lacrimal punctum. This new type of operation not only avoids impairment of the horizontal and vertical parts of the canaliculi but also prevents early healing of lacrimal punctum in patients with active ocular inflammation.On the other hand, some patients with lacrimal canaliculus stenosis can be cured after three months of canaliculus dilation with the tube, which is beneficial for the recovery of lacrimal drainage function and the success rate at the last follow‐up.
In the present study, the assessment of tear drainage using FDDT and showed significant improvement for the patients after tube removal, indicating that our technique could improve the function of tear drainage. At the last follow‐up, a total of 41 eyes represented a normal tear drainage function,reaching 65.1%, and the effective rate was 98.4%. Only 4 improved subjects who had epiphora symptoms were patients aged over 70, and they all had different degrees of eyelid skin relaxation and decreased function of orbicularis oculi muscle.The punctoplastyviaKelly punch with RS silicone intubation,compared with the control group, achieved a higher anatomical and functional success rate. We think that the Kelly punch is easier to obtain a quasi‐circular incision similar to the normal punctum. Coupled with the use of RS tube, the new technique can more effectively prevent the long‐term contraction and poor formation of the punctum. So the significant higher functional success rate in group B can be attributed to the combination effects of the punch and the tube. Also, the postoperative symptom score of the patients was also relatively better, and the patient satisfaction was higher. Furthermore, we found a strong positive correlation between TMH and Munk score. We believe that measuring TMH is a rapid, quantitative, and objective way to evaluate the canalicular patency in APES cases.
In conclusion, we here reported a new technique, with simple surgical procedures, can effectively treat the membrane closure of lacrimal punctum, keep the lacrimal punctum open, prevent restenosis and obtain satisfactory clinical outcomes. A larger sample size and longer follow‐ups is needed in future to further verify its safety and effectiveness.
ACKNOWLEDGEMENTS
Conflicts of Interest: Cao X,None;Hu ZZ,None;Wu Y,None;Song Y,None;Liu QH,None.
 International Journal of Ophthalmology2021年6期
International Journal of Ophthalmology2021年6期
- International Journal of Ophthalmology的其它文章
- A decrease in macular microvascular perfusion after retinal detachment repair with silicone oil
- Role of bevacizumab intraocular injection in the management of neovascular glaucoma
- Primary rhegmatogenous retinal detachment: evaluation of a minimally restricted face-down positioning after pars plana vitrectomy and gas tamponade
- Association of eleven single nucleotide polymorphisms with refractive disorders from Eskisehir, Turkey
- Evaluation of macular vessel density changes after vitrectomy with silicone oil tamponade in patients with rhegmatogenous retinal detachment
- Triamcinolone as an adjunct to the combination of anti-VEGF for the management of diabetic macular edema
