鹽酸麻黃堿皮下浸潤聯合晶體共負荷預防剖宮產腰麻后低血壓的效果分析
張雪苗 岳圓圓 趙文琪 范修穎 張月順
【摘要】 目的:觀察鹽酸麻黃堿與1%利多卡因混合皮下逐層浸潤聯合晶體液共負荷預防剖宮產產婦腰麻后低血壓的效果以及對新生兒的影響。方法:選取牡丹江市婦女兒童醫院2019年10月-2020年1月收入院的60例擇期在腰麻下行剖宮產產婦。根據電腦生成的隨機數字,按隨機數字表法將產婦隨機分為C組和E組,每組30例。C組采用晶體共負荷,E組采用晶體共負荷聯合鹽酸麻黃堿皮下浸潤。比較兩組各時間點MAP、HR水平和并發癥發生情況。比較兩組靜脈應用鹽酸麻黃堿劑量,比較兩組新生兒的酸中毒及Apgar評分情況。結果:T4~T8,E組的MAP均明顯高于C組,差異均有統計學意義(P<0.05);T0~T3,兩組的MAP、HR比較,差異均無統計學意義(P>0.05);T4~T8,兩組的HR比較,差異均無統計學意義(P>0.05)。E組低血壓發生率為33.3%,低于C組的63.3%,差異有統計學意義(P<0.05);E組惡心發生率為13.3%,低于C組的36.7%,差異有統計學意義(P<0.05);兩組反應性高血壓、嘔吐發生率比較,差異均無統計學意義(P>0.05);C組靜脈應用鹽酸麻黃堿的總劑量明顯高于E組,差異有統計學意義(P<0.05)。E組的pH明顯高于C組,堿剩余、乳酸均明顯優于C組,差異均有統計學意義(P<0.05);新生兒的1、5 min Apgar評分比較,差異均無統計學意義(P>0.05)。結論:鹽酸麻黃堿皮下浸潤聯合晶體液共負荷用于預防腰麻后低血壓,血流動力學穩定,無明顯反應性高血壓,對新生兒影響較小,可以作為一種安全、有效的預防手段。
【關鍵詞】 低血壓 蛛網膜下腔麻醉 剖宮產 鹽酸麻黃堿 晶體共負荷
[Abstract] Objective: To observe the effect of Ephedrine Hydrochloride and 1% Lidocaine mixed subcutaneous layer by layer infiltration combined with crystal co-loading on the prevention of hypotension after lumbar anesthesia in cesarean section parturients and its effect on neonates. Method: A total of 60 parturients who received cesarean section under lumbar anesthesia were selected from Mudanjiang Women’s and Children’s Hospital from October 2019 to January 2020. According to the computer generated random numbers, the parturient women were randomly divided into group C and group E according to the random number table method,?30 cases in each group. Group C was treated with crystal co-loading, while group E was treated with crystal co-loading combined with Ephedrine Hydrochloride subcutaneous infiltration. MAP, HR level and complications were compared between the two groups at each time point. The dose of intravenous Ephedrine Hydrochloride was compared between the two groups, the acidosis and Apgar score of neonates in the two groups were compared. Result: T4 to T8, the MAP of group E were significantly higher than those of group C, the differences were statistically significant (P<0.05). T0 to T3, comparison of MAP and HR between the two groups, there were no statistical significance between the two groups (P>0.05). T4 to T8, comparison of HR between the two groups, there were no statistically significant differences (P>0.05). The incidence of hypotension in group E was 33.3%, which was lower than 63.3% in group C, the difference was statistically significant (P<0.05). The incidence of nausea in group E was 13.3%, compared with 36.7% in group C, the difference was statistically significant (P<0.05). The incidences of reactive hypertension and vomiting were compared between the two groups, the differences were not statistically significant (P>0.05). The total dose of intravenous Ephedrine Hydrochloride in group C was significantly higher than that in group E, the difference was statistically significant (P<0.05). The pH of group E was significantly higher than that of group C, base excess and lactic acid were significantly better than those of group C, the differences were statistically significant (P<0.05). Comparison of 1 and 5 min Apgar scores between the two groups, there were no statistically significant differences (P>0.05). Conclusion: Ephedrine Hydrochloride subcutaneous infiltration combined with crystal co-loading can be used to prevent hypotension after spinal anesthesia, with stable hemodynamics and no obvious reactive hypertension, it has little effect on newborns, and can be used as a safe and effective prevention method.
[Key words] Hypotension Spinal anesthesia Cesarean delivery Ephedrine Hydrochloride Crystal co-loading
First-author’s address: Mudanjiang Medical University, Mudanjiang 157000, China
doi:10.3969/j.issn.1674-4985.2021.22.005
蛛網膜下腔麻醉又稱腰麻,是產科麻醉的首選麻醉方式,而腰麻后低血壓(spinal anaesthesia-induced hypotension, SAIH)是其最常見的不良并發癥。SAIH可導致產婦術中出現惡心、嘔吐等,嚴重的低血壓還會導致產婦循環功能障礙、胎兒缺血、缺氧、酸中毒,甚至危及產婦及胎兒生命[1-2]。SAIH的定義和監測手段尚存在爭議,SAIH的發生率達30%~100%[3-5]。目前,體位干預、晶體液或膠體液共負荷/預負荷、應用血管活性藥物等方法在治療和預防SAIH方面都展現出不同效果。但是,液體預擴容或者體位干預預防SAIH,臨床效果欠佳,通常需要使用補救性血管活性藥物[6-7]。麻黃堿是產科麻醉中常用的血管收縮藥物之一,其升壓效果具有一定劑量依賴性,低劑量升壓效果不足,較高劑量常常又會引起產婦高血壓且易導致心動過速[8]。研究表明腰麻前10 min肌肉注射0.5 mg/kg麻黃堿預防SAIH,術中產婦血壓波動范圍較小[9],表明合適劑量的麻黃堿肌肉注射或者皮下局部浸潤可使產婦術中血流動力學穩定。鹽酸麻黃堿皮下局部浸潤聯合晶體共負荷預防SAIH的研究鮮見報道,故本研究旨在探討這種方案在剖宮產術中預防SAIH是否為一種安全、有效的臨床方案,現報道如下。
1 資料與方法
1.1 一般資料 選取牡丹江市婦女兒童醫院2019年
10月-2020年1月收入院的60例擇期在腰麻下行剖宮產產婦。納入標準:(1)足月擇期剖宮產;(2)胎兒發育正常,無畸形;(3)胎膜早破無嚴重感染;(4)產婦年齡22~35周歲;(5)ASA分級Ⅰ級或Ⅱ級;(6)單胎。排除標準:(1)妊娠合并高血壓、糖尿病、心臟病;(2)患有HELLP綜合征;(3)蛛網膜下腔麻醉失敗;(4)椎管內麻醉穿刺禁忌證。根據電腦生成的隨機數字,按隨機數字表法將產婦分為C組和E組,每組30例。患者或家屬同意并簽署知情同意書,研究經該院倫理委員會同意批準。
1.2 方法 所有產婦無術前用藥,常規禁水4 h、禁食6 h,入手術室后,平臥位,右側髖部側墊高15°,常規監測心電圖(ECG)、血壓(BP)、心率(HR)、血氧飽和度(SpO2)。18G留置針左前臂建立靜脈通道,面罩吸氧4 mL/min。囑患者平靜休息5 min后,每間隔2 min連續3次測量,每次測量的MAP波動范圍<10%,三次測量的MAP均值記為產婦基礎MAP,三次測量對應的平均HR,記為產婦基礎HR,此時間點記為T0。產婦取左側膝胸位,L3~4行蛛網膜下腔麻醉。L3~4椎間隙逐層浸潤麻醉,C組局麻藥配制:1%鹽酸利多卡因注射液(生產廠家:山東華魯制藥有限公司,批準文號:國藥準字H37022839,規格:10 mL︰0.2 g)
4 mL;E組局麻藥配制:1%利多卡因+15 mg鹽酸麻黃堿注射液(生產廠家:東北制藥集團沈陽第一制藥有限公司,批準文號:國藥準字H21022412,規格:1 mL︰30 mg)至4 mL,用18G硬膜外針(埃斯埃麻醉穿刺包,上海)硬膜外穿刺至硬膜外腔,成功后用腰麻針穿刺至蛛網膜下腔,見腦脊液外流后,緩慢注入重比重腰麻液[0.75%羅哌卡因(生產廠家:AstraZeneca AB,批準文號:注冊證號H20140764,規格:10 mL︰75 mg)2 mL+50%葡萄糖(生產廠家:山東華魯制藥有限公司,批準文號:國藥準字H20184027,規格:20 mL︰10 g)
0.2 mL+0.9%氯化鈉注射液(生產廠家:辰欣藥業股份有限公司,批準文號:國藥準字H20013310,規格:100 mL︰0.9 g)0.8 mL,推注速度為0.1 mL/s,硬膜外腔置管備用,將麻醉平面調節控制在T6~8,右側髖部墊高15°。C、E兩組在腰麻液注入蛛網膜下腔即刻,15 mL/kg的乳酸鈉林格注射液(生產廠家:山東威高藥業股份有限公司,批準文號:國藥準字H20044239,規格:500 mL)以最大速度靜脈輸注。腰麻液注入蛛網膜下腔后1、3、5、7、10、15、20、30 min的各個時間點分別記為T1、T2、T3、T4、T5、T6、T7、T8,測量記錄腰麻液注入蛛網膜下腔后各時間點MAP、HR。胎兒娩出后未啼哭前夾閉臍帶即刻采取臍帶動脈血1 mL,立刻使用血氣分析儀(RADIOMETER)進行血氣分析。術中產婦若出現低血壓(MAP<基礎值20%)靜脈應用鹽酸麻黃堿5~10 mg,效果不明顯可重復使用,直到血壓恢復>基礎血壓80%;若出現心動過緩(HR<50次/min)靜脈應用硫酸阿托品注射液(生產廠家:安徽長江藥業有限公司,批準文號:國藥準字H34021900,規格:1 mL︰0.5 mg)0.5 mg直到心率恢復>50次/min;若出現反應性高血壓,MAP>基礎值30%時,靜脈應用烏拉地爾注射液(生產廠家:廣州萬正藥業有限公司,批準文號:國藥準字H20010806,規格:5 mL︰25 mg)5 mg,C、E兩組晶體液速度降至40~60滴/min。
1.3 觀察指標及判定標準 比較兩組T1~T8各時間點MAP、HR水平。比較兩組并發癥發生情況,包括低血壓、反應性高血壓、惡心、嘔吐。比較兩組靜脈應用鹽酸麻黃堿劑量。比較兩組新生兒的酸中毒及Apgar評分情況,包括新生兒臍動脈pH值、堿剩余、乳酸及新生兒1、5 min Apgar評分情況,Apgar評分滿分10分,分數越高新生兒情況越好。
1.4 統計學處理 采用SPSS 22.0軟件對所得數據進行統計分析,計量資料用(x±s)表示,比較采用t檢驗;計數資料以率(%)表示,比較采用字2檢驗。以P<0.05為差異有統計學意義。
2 結果
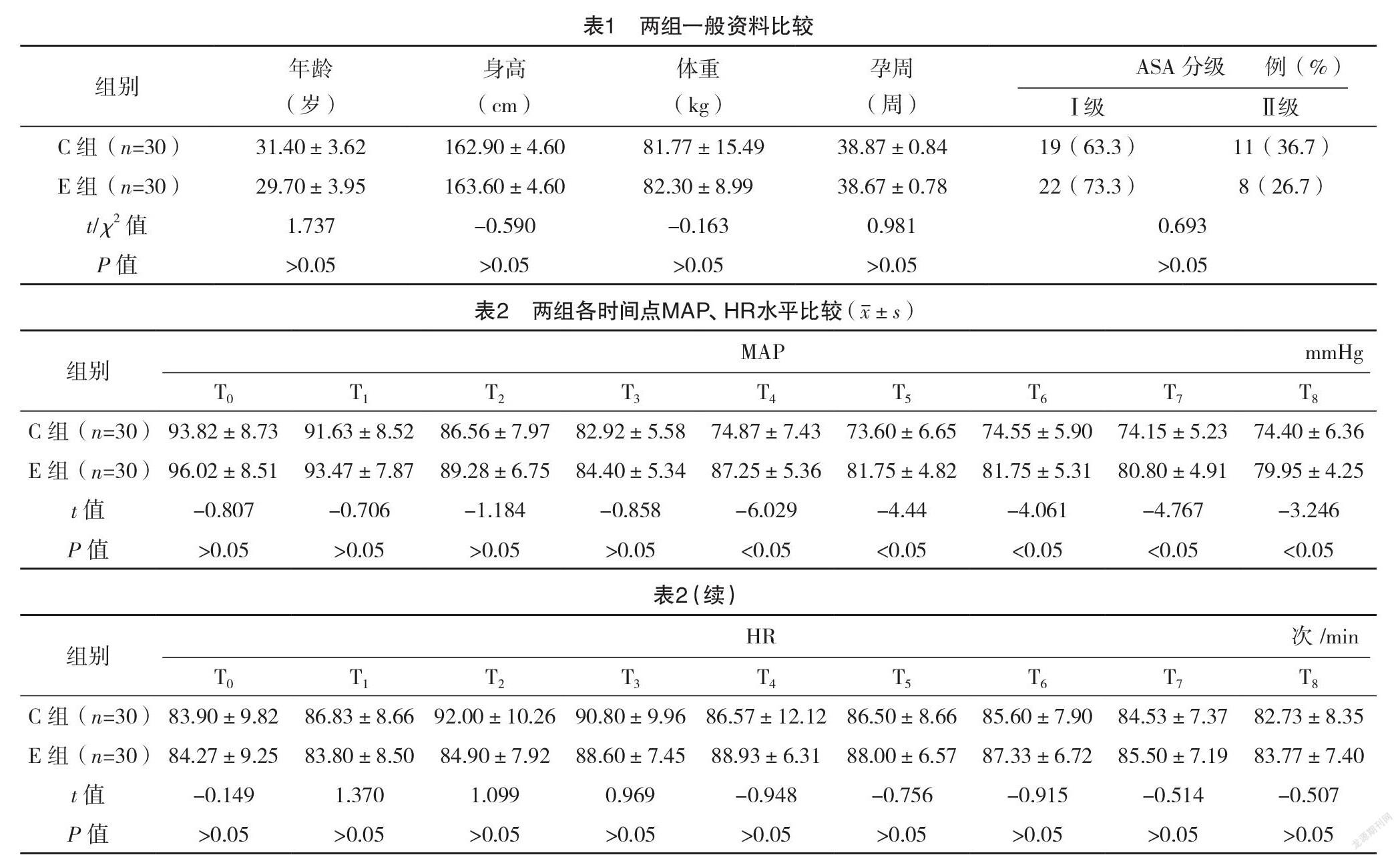
2.1 兩組一般資料比較 兩組年齡、身高、體重、孕周、ASA分級比較,差異均無統計學意義(P>0.05),見表1。
2.2 兩組各時間點MAP、HR水平比較 T4~T8,E組的MAP均明顯高于C組,差異均有統計學意義(P<0.05);T0~T3,兩組的MAP、HR比較,差異均無統計學意義(P>0.05);T4~T8,兩組的HR比較,差異均無統計學意義(P>0.05)。見表2。
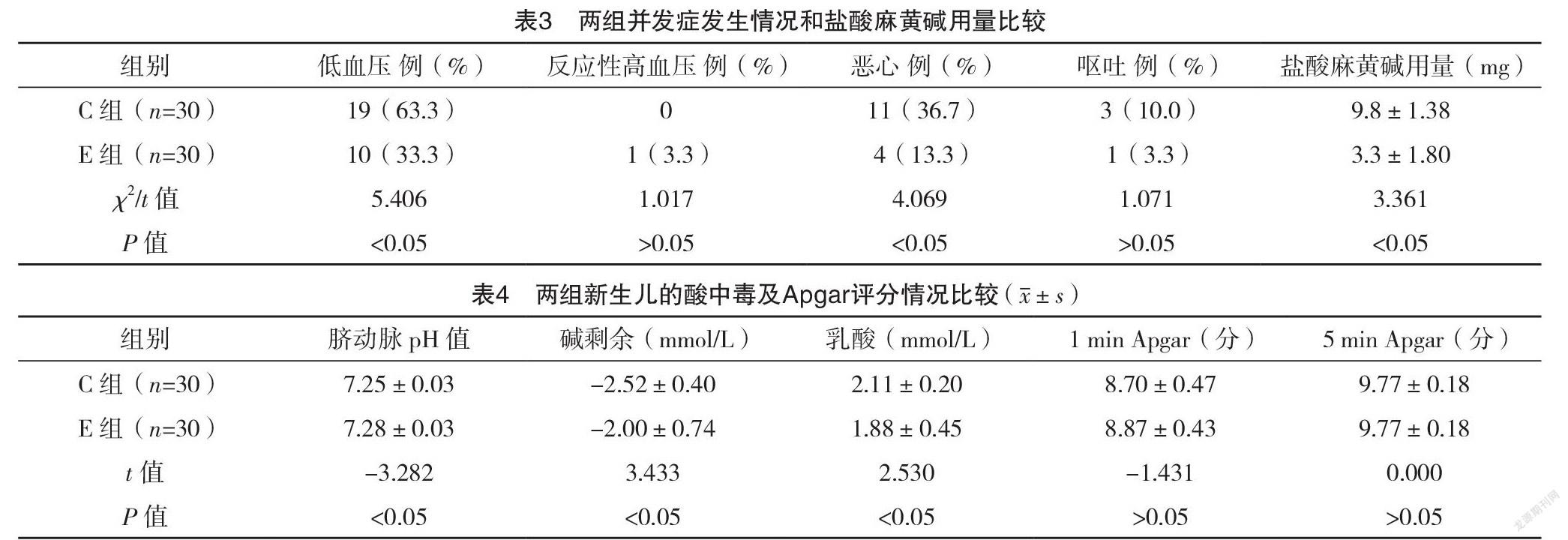
2.3 兩組并發癥發生情況和鹽酸麻黃堿用量比
較 E組低血壓發生率為33.3%,低于C組的63.3%,差異有統計學意義(P<0.05);E組惡心發生率為13.3%,低于C組的36.7%,差異有統計學意義(P<0.05);兩組反應性高血壓、嘔吐發生率比較,差異均無統計學意義(P>0.05);C組靜脈應用鹽酸麻黃堿的總劑量明顯高于E組,差異有統計學意義(P<0.05)。見表3。
2.4 兩組新生兒的酸中毒及Apgar評分情況比較 E組的pH明顯高于C組,堿剩余、乳酸均明顯優于C組(P<0.05);新生兒的1、5 min Apgar評分比較,差異均無統計學意義(P>0.05)。見表4。
3 討論
麻黃堿可以增加產婦心排血量(CO)和改善胎盤的血供[10]。臨床上常常在SAIH發生時靜脈推注麻黃堿5~10 mg,較少預防性肌注或皮下應用麻黃堿。鹽酸麻黃堿肌注/皮下單次劑量為15~30 mg,極量為60 mg,為預防反應性高血壓的發生,本研究選擇了肌注最小有效劑量15 mg。近年來,剖宮產術中防治SAIH發生的液體管理方案一直存在爭議,主要表現在液體的選擇、晶膠輸注配比、液體的輸注時機這三方面[6],目前最常用的液體管理方案為晶體預/共負荷、膠體預/共負荷。蘇鴻莉等[11]的研究發現膠體液預負荷與晶體液共負荷預防剖宮產術中SAIH的效果無明顯統計學差異,而膠體液易導致過敏反應、凝血功能障礙等不良并發癥發生[12],因此臨床上常選用晶體進行擴容。另外,Ni等[13]的研究發現晶體共負荷預防SAIH的效果優于晶體預負荷。因此本研究選擇15 mL/kg乳酸林格共負荷預防產婦術中SAIH。
晶體共負荷可以減少SAIH的發生率,但單獨晶體共負荷預防SAIH效果有限。Mercier[14]分析得出,在腰麻后最初的5~10 min輸注足夠的液體,并預防性應用血管收縮藥物可以增加單獨晶體共負荷預防SAIH的效果。與此結論一致,Buthelezi等[15]的研究中將苯腎上腺素500 μg加入1 000 mL乳酸林格液中共負荷輸注,產婦SAIH的發生率降低了29%。與Mercier[14]的研究結果一致,本研究中,與單純晶體共負荷輸注相比,局麻時1%利多卡因與15 mg鹽酸麻黃堿混合局部浸潤,低血壓的發生率降低了30%。其作用機制可能是鹽酸麻黃堿在SAIH發生前逐漸發揮作用,從而減少了SAIH的發生。但33%的產婦出現SAIH,這不除外本試驗中鹽酸麻黃堿劑量較小的可能,提示對一般產婦來說可能存在更適合的劑量,需進一步探索。本研究中E組發生了1例反應性高血壓,但是MAP升高的幅度<基礎血壓30%,且產婦無不適發生。
本研究結果顯示,T4~T8,E組的MAP均明顯高于C組,差異均有統計學意義(P<0.05);T0~T3,兩組的MAP、HR比較,差異均無統計學意義(P>0.05);T4~T8,兩組的HR比較,差異均無統計學意義(P>0.05)。從T4~T8時間點,與T0時相比,E組MAP的下降程度明顯小于C組,表明E組血壓波動較小,血流動力學較C組穩定。這說明晶體共負荷聯合應用麻黃堿可以從降低低血壓的發生率及低血壓的嚴重程度,從而維持產婦腰麻后血流動力學的穩定。然而,鹽酸麻黃堿皮下局部浸潤給藥相對于靜脈給藥而言,吸收緩慢,達到有效血藥濃度需要一定的時間,這在一定程度上削弱了其對SAIH的預防作用。但在本研究中鹽酸麻黃堿達到有效血藥濃度之前,靜脈快速輸注的晶體液可以抵消一部分因腰麻導致血管擴張造成的血容量相對不足;另外,局部麻醉藥所具有的血管擴張作用加速了鹽酸麻黃堿的吸收,從而維持血壓平穩。
產婦血流動力學的穩定,良好的胎盤灌注對于胎兒酸堿狀態的影響至關重要。麻黃堿可通過胎盤影響胎兒pH值。Kee等[16]的研究發現鹽酸麻黃堿可通過胎盤激動胎兒的β受體增加其新陳代謝,使氧氣相對不足,致臍動脈血pH降低。Rolbin等[17]進一步研究表明腰麻前預防性肌肉注射鹽酸麻黃堿45 mg對胎兒的pH值和Apgar評分無顯著影響,當鹽酸麻黃堿肌肉注射增至50 mg時才出現胎兒酸中毒。可見鹽酸麻黃堿對胎兒pH的影響可能存在劑量相關性。本研究結果顯示,E組的pH明顯高于C組,差異有統計學意義(P<0.05),沒有出現1例嚴重酸中毒(pH<2.0),并且無一例pH<2.5。這可能是E組麻黃堿維持血流動力學穩定的結果,也不除外鹽酸麻黃堿使用劑量較小。另外,E組的堿剩余、乳酸均明顯低于C組,差異均有統計學意義(P<0.05);進一步表明E組維持血壓較平穩,對新生兒的不良影響較小。蛛網膜下腔阻滯引起的低血壓和仰臥位低血壓綜合征、飽胃、手術牽拉刺激等均可引起產婦惡心嘔吐[18-19]。本研究結果顯示,E組惡心發生率低于C組,差異有統計學意義(P<0.05)。C組靜脈應用鹽酸麻黃堿的總劑量明顯高于E組,差異有統計學意義(P<0.05),也進一步表明E組的血壓維持優于C組。本研究選取的研究對象為健康產婦,有研究表明先兆子癇產婦的SAIH的發生率和嚴重程度均低于健康女性[20],而該方案在循環功能障礙、妊娠期高血壓產婦或者先兆子癇產婦中的應用安全性有待進一步研究。
綜上所述,鹽酸麻黃堿局部浸潤聯合晶體共負荷預防SAIH,低血壓發生率明顯降低,術中血壓波動范圍小,且無明顯反應性高血壓等不良反應,對胎兒的酸堿狀態影響較小,可安全應用于健康產婦。
參考文獻
[1] George R B,Mckeen D M,Dominguez J E,et al.A randomized trial of phenylephrine infusion versus bolus dosing for nausea and vomiting during Cesarean delivery in obese women[J].Can J Anaesth,2018,65(3):254-262.
[2] Lappen J R,Chien E K,Mercer B M.Contraction-Associated Maternal Heart Rate Decelerations: A Pragmatic Marker of Intrapartum Volume Status[J].Obstet Gynecol,2018,132(4):1011-1017.
[3]杜唯佳,徐振東,劉志強.剖宮產腰麻后低血壓預測方法的研究進展[J].臨床麻醉學雜志,2019,35(2):192-194.
[4] Tan H S,Gan Y T,Tan E C,et al.Association of renin-angiotensin-aldosterone system genetic polymorphisms with maternal hypotension during spinal anaesthesia for caesarean delivery - a retrospective cohort study[J].International Journal of Obstetric Anesthesia,2020,44:3-12.
[5]王云秀,左小清.剖宮產椎管內麻醉產婦發生低血壓的危險因素分析[J].臨床醫學研究與實踐,2019,4(11):85-86,99.
[6]陳偉,陳永權.剖宮產腰麻后低血壓防治措施的研究進展[J/OL].中華臨床醫師雜志(電子版),2019,13(4):312-315.
[7]丁振東,譚慧玲,鄭洪,等.麻醉前預泵注間羥胺對剖宮產產婦腰麻后低血壓的防治作用[J].臨床麻醉學雜志,2020,36(6):599-601.
[8] Nag D S.Vasopressors in obstetric anesthesia: A current perspective[J].World Journal of Clinical Cases,2015,3(1):58-64.
[9] Bhar D,Bharati S,Halder P S,et al.Efficacy of prophylactic intramuscular ephedrine in prevention of hypotension during caesarean section under spinal anaesthesia: a comparative study[J].J Indian Med Assoc,2011,109(5):300-303,307.
[10] Guo R,Xue Q,Qian Y,et al.The Effects of Ephedrine and Phenylephrine on Placental Vascular Resistance During Cesarean Section Under Epidual Anesthesia[J].Cell Biochem Biophy,2015,73(3):687-693.
[11]蘇鴻莉,晉雅凌.膠體液預負荷和晶體液共負荷在預防腰麻剖宮產術中低血壓效應的臨床療效對比[J].安徽醫藥,2015,19(11):2210-2212.
[12] Heesen M,Stewart A,Fernando R.Vasopressors for the treatment of maternal hypotension following spinal anaesthesia for elective caesarean section: past, present and future[J].Anaesthesia,2015,70(3):252-257.
[13] Ni H F,Liu H Y,Zhang J,et al.Crystalloid Coload Reduced the Incidence of Hypotension in Spinal Anesthesia for Cesarean Delivery, When Compared to Crystalloid Preload: A Meta-Analysis[J].BioMed Research International,2017,2017:1-10.
[14] Mercier F J.Cesarean delivery fluid management[J].Curr Opin Anaesthesiol,2012,25(3):286-291.
[15] Buthelezi A S,Bishop D G,Rodseth R N,et al.Prophylactic phenylephrine and fluid co-administration to reduce spinal hypotension during elective caesarean section in a resource-limited setting: a prospective alternating intervention study[J].Anaesthesia,2019,75(4):487-492.
[16] Kee W N,Khaw K S,Tan P E,et al.Placental transfer and fetal metabolic effects of phenylephrine and ephedrine during spinal anesthesia for cesarean delivery[J].Anesthesiology,2009,111(3):506-512.
[17] Rolbin S H,Cole A,Hew E M,et al.Prophylactic intramuscular ephedrine before epidural anaesthesia for caesarean section: Efficacy and actions on the foetus and newborn[J].Can Anaesth Soc J,1982,29(2):148-153.
[18]趙軍博,姜麗華,楊波.多拉司瓊與托烷司瓊用于預防子宮收縮劑引發的剖宮產產婦惡心嘔吐的效果比較[J].數理醫藥學雜志,2020,33(7):1013-1015.
[19] Ashagrie H E,Chekol T D,Melese D Y,et al.The incidence and factors associated with intraoperative nausea and vomiting during cesarean section under spinal anesthesia, July 2019. An institution based cross sectional study[J].International Journal of Surgery Open,2020,26:49-54.
[20] Sivevski A,Ivanov E,Karadjova D,et al.Spinal-Induced Hypotension in Preeclamptic and Healthy Parturients Undergoing Cesarean Section[J].Open Access Maced J Med Sci,2019,7(6):996-1000.
(收稿日期:2020-11-11) (本文編輯:姬思雨)