神經(jīng)外科顱腦損傷患者開展優(yōu)質(zhì)護(hù)理對(duì)睡眠質(zhì)量的影響研究
于海靜
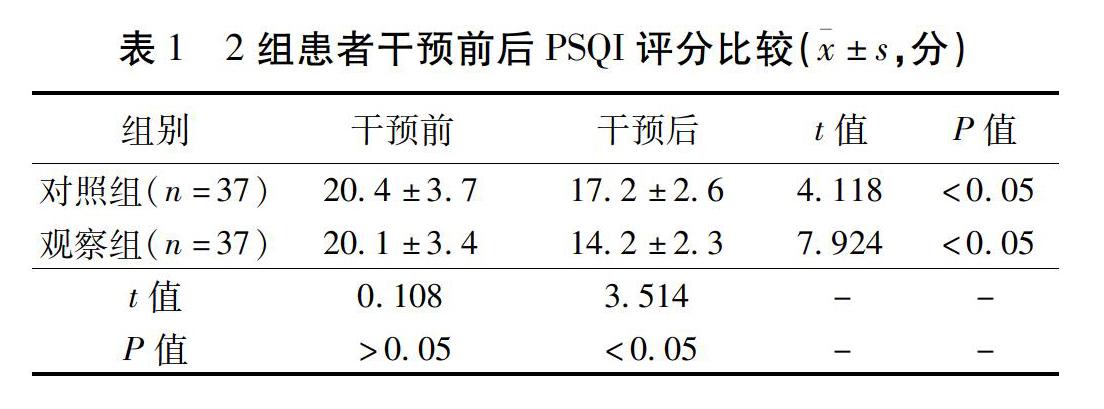
摘要 目的:探討優(yōu)質(zhì)護(hù)理在神經(jīng)外科顱腦損傷患者中使用對(duì)睡眠質(zhì)量的臨床影響。方法:選取2018年8月至2019年8月德州市陵城區(qū)中醫(yī)院神經(jīng)外科收治的顱腦損傷患者74例作為研究對(duì)象,按照隨機(jī)數(shù)字表法隨機(jī)分成觀察組和對(duì)照組,每組37例。其中對(duì)照組采取常規(guī)護(hù)理,觀察組采取優(yōu)質(zhì)護(hù)理,比較2組睡眠質(zhì)量改善情況。結(jié)果:2組干預(yù)前PSQI評(píng)分比較差異無統(tǒng)計(jì)學(xué)意義(P>0.05),干預(yù)后觀察組PSQI評(píng)分為(14.2±2.3)分,明顯低于對(duì)照組,且2組干預(yù)后PSQI評(píng)分均低于同組干預(yù)前,比較差異有統(tǒng)計(jì)學(xué)意義(P<0.05)。結(jié)論:優(yōu)質(zhì)護(hù)理在神經(jīng)外科顱腦損傷患者中使用可有效改善患者睡眠質(zhì)量,值得推廣。
關(guān)鍵詞 神經(jīng)外科;顱腦損傷;優(yōu)質(zhì)護(hù)理;睡眠質(zhì)量;影響
Abstract Objective:To explore the clinical effect of quality nursing on sleep quality in patients with craniocerebral injury in neurosurgery department.Methods:A total of 74 cases of craniocerebral injury patients admitted to the neurosurgery department of our hospital from August 2018 to August 2019 were included in this study.The patients were randomly divided into two groups,37 cases each.The control group received routine nursing,the observation group received quality nursing,and the improvement of sleep quality was compared between the two groups.Results:There was no significant difference in PSQI score between the two groups before intervention(P>0.05),and the PSQI score of the observation group was(14.2±2.3)points,significantly lower than that of the control group after intervention,and the PSQI score of both groups was lower than that of the same group before intervention,with a statistical difference(P<0.05).Conclusion:High-quality nursing can effectively improve the sleep quality of patients with craniocerebral injury in neurosurgery,and it is worth promoting.
Keywords Neurosurgery; Brain injury; Quality care; Sleep quality; Impact
中圖分類號(hào):R338.63 文獻(xiàn)標(biāo)識(shí)碼:A doi:10.3969/j.issn.2095-7130.2020.08.069
顱腦外傷為神經(jīng)外科常見創(chuàng)傷性疾病,主要因外界暴力導(dǎo)致的頭部損傷,包括腦震蕩、頭皮撕脫傷、顱內(nèi)血腫及顱骨骨折等,且伴隨程度不一的惡心嘔吐、頭痛頭暈及意識(shí)障礙等癥狀,主要特點(diǎn)為發(fā)生率高且預(yù)后差[1]。近年來我國高空作業(yè)及交通事業(yè)不斷發(fā)展進(jìn)步,導(dǎo)致顱腦外傷發(fā)生率也逐年提升,資料稱[2]顱腦外傷中嚴(yán)重性顱腦損傷占比為10% ~20%,嚴(yán)重威脅患者生命安全。顱腦外科手術(shù)技術(shù)不斷更新完善,臨床十分重視顱腦損傷的診治及康復(fù)訓(xùn)練,但常規(guī)護(hù)理方案效果欠佳,預(yù)后較差,近年來護(hù)理醫(yī)學(xué)逐年發(fā)展后臨床各個(gè)科室均引入優(yōu)質(zhì)護(hù)理,研究證實(shí)[3]科學(xué)合理的護(hù)理服務(wù)可有效改善臨床預(yù)后。現(xiàn)選取患者74例,詳述優(yōu)質(zhì)護(hù)理的應(yīng)用效果。
1 資料與方法
1.1 一般資料 選取2018年8月至2019年8月德州市陵城區(qū)中醫(yī)院神經(jīng)外科收治的顱腦損傷患者74例作為研究對(duì)象,按照隨機(jī)數(shù)字表法隨機(jī)分成觀察組和對(duì)照組,每組37例。所有患者均經(jīng)影像學(xué)檢查證實(shí)為顱腦損傷,知曉本研究并簽署知情同意書。對(duì)照組采取常規(guī)護(hù)理,觀察組采取優(yōu)質(zhì)護(hù)理。對(duì)照組中男24例,女13例,年齡23~64歲,平均年齡(40.7±7.4)歲;致傷原因:車禍傷23例,高空墜落傷8例,打擊斗毆傷6例。觀察組中男22例,女15例,年齡21~67歲,平均年齡(41.2±7.9)歲;致傷原因:車禍傷22例,高空墜落傷8例,打擊斗毆傷7例。2組患者一般資料經(jīng)統(tǒng)計(jì)學(xué)分析,差異無統(tǒng)計(jì)學(xué)意義(P>0.05),具有可比性。
1.2 研究方法 對(duì)照組采取常規(guī)護(hù)理,急性期做好搶救工作,遵醫(yī)囑開展護(hù)理操作,待患者病情穩(wěn)定且處于清醒狀態(tài)后開展健康宣教,對(duì)康復(fù)注意事項(xiàng)予以講解。觀察組基于此采取優(yōu)質(zhì)護(hù)理,具體如下:1)全面評(píng)估:護(hù)士要主動(dòng)溝通于患者,對(duì)其基礎(chǔ)資料予以全面了解和收集,包括生命體征、病情程度及意識(shí)狀態(tài)等,分析相關(guān)數(shù)據(jù)后使用通俗易懂的語言講解疾病相關(guān)知識(shí)、科室管理規(guī)定等,提高患者配合度。2)將護(hù)理方案制定出來:將患者資料收集完畢后護(hù)士需結(jié)合患者病情程度與傷情對(duì)頭骨外的損傷予以細(xì)致檢查,對(duì)脈搏、呼吸、顱內(nèi)壓及心電圖等生命體征予以密切觀察,開展APACHEII動(dòng)態(tài)監(jiān)測(cè),并依據(jù)分?jǐn)?shù)對(duì)護(hù)士予以分配,將護(hù)理策略制定出來,密切觀察患者疾病情況,評(píng)估生命體征變化情況。3)心理疏導(dǎo):顱腦損傷患者因擔(dān)憂預(yù)后不良及病情程度故而表現(xiàn)出嚴(yán)重不良情緒,家屬也在一定程度上表現(xiàn)負(fù)性情緒,導(dǎo)致患者不良情緒狀態(tài)加重。護(hù)士需與患者及其家屬溝通交流,把握患者心理特征及個(gè)性特點(diǎn),開展針對(duì)性心理護(hù)理,通過鼓勵(lì)、解釋及安慰等方法對(duì)其抑郁、焦慮、擔(dān)憂及恐懼等情緒予以緩解,可對(duì)治療成功案例予以講解以增強(qiáng)其抗病信心。4)生活指導(dǎo):結(jié)合患者生活習(xí)慣將科學(xué)合理的生活作息計(jì)劃表制定出來,包括休息、飲食及運(yùn)動(dòng)等,如多補(bǔ)充纖維素、蛋白質(zhì)及維生素等,限制鹽分與脂肪攝取,將機(jī)體抵抗力增強(qiáng)。對(duì)患者口腔黏膜及皮膚予以觀察,了解有無瞳孔與角膜變化、出血及導(dǎo)管有無壓迫或反折現(xiàn)象等。5)預(yù)防感染:每日定時(shí)消毒病房,將污染床單及衣物及時(shí)更換,確保病房處于潔凈狀態(tài);限制病房人員出入量,合理使用抗生素,對(duì)痰液黏度、量及性質(zhì)等予以觀察,以控制感染。

