新產程管理模式下活躍期不同時限對母嬰結局的影響
崔建玲 廖曉禮 曾麗香

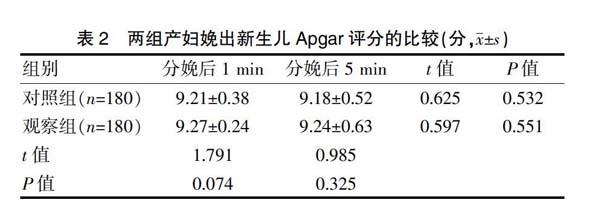

[摘要]目的 探討新產程管理模式下活躍期不同時限對母嬰結局的影響。方法 回顧性分析2018年7月~2019年7月我院婦產科收治的360例足月初產婦的臨床資料,根據活躍期的不同進行分組,將其中180例活躍期<4 h的產婦納入對照組,將另外180例活躍期≥4 h的產婦納入觀察組。比較兩組產婦圍術期指標、新生兒分娩后1、5 min Apgar評分、妊娠結局以及妊娠并發癥發生情況。結果 觀察組產婦產后出血量少于對照組,總產程時間長于對照組,差異有統計學意義(P<0.05);兩組新生兒分娩后5 min的Apgar評分與分娩后1 min比較,差異無統計學意義(P>0.05);觀察組產婦中轉剖宮產率低于對照組,差異有統計學意義(P<0.05);兩組羊水糞染及新生兒窒息發生率比較,差異無統計學意義(P>0.05)。結論 新產程管理模式以活躍期停滯時間>4 h再考慮是否作為手術的指征,可使產婦有充分的時間試產,降低剖宮產率,改善圍術期指標,利于產婦預后,推薦臨床推廣應用。
[關鍵詞]新產程管理模式;活躍期不同時限;母嬰結局
[中圖分類號] R714? ? ? ? ? [文獻標識碼] A? ? ? ? ? [文章編號] 1674-4721(2020)7(b)-0122-03
Effect of different time limits of active period on maternal and infant outcomes under the new labor management mode
CUI Jian-ling1? ?LIAO Xiao-li1? ?ZENG Li-xiang2
1. Department of Obstetrics, Medical and Child Health Care and Family Planning Service Center of Huizhou City, Guangdong Province, Huizhou? ?516001, China; 2. Department of Medical Records, Medical and Child Health Care and Family Planning Service Center of Huizhou City, Guangdong Province, Huizhou? ?516001, China
[Abstract] Objective To explore the effect of different time limits of active period on the maternal and infant outcomes under the new labor management model. Methods Retrospective analysis of the clinical data of 360 full-term primiparas treated to the department of obstetrics and gynecology in our hospital from July 2018 to July 2019. Grouped according to the different active periods, 180 pregnant women with active period <4 h were included in the control group, and another 180 pregnant women with active period ≥4 h were included in the observation group. The perioperative indicators, the Apgar scores at 1 minute and 5 minutes after delivery, the pregnancy outcomes and complications were compared between the two groups. Results The maternal postpartum hemorrhage volume in the observation group was lower than that in the control group, and the total duration of labor was longer than that in the control group, the differences were statistically significant (P<0.05). There were no significant differences in the Apgar score of newborns between the two groups 5 minutes after delivery and 1 minute after delivery (P>0.05). The rate of maternal conversion tocesarean section in the observation group was lower than that in the control group, and the difference was statistically significant (P<0.05). There was no significant difference in the incidence of amniotic fluid fecal infection and neonatal asphyxia between the two groups (P>0.05). Conclusion The new labor management mode takes the active period >4 h as the treatment time limit to allow the pregnant women to have sufficient time for trial delivery, reduce the cesarean delivery rate, improve the perioperative index, and benefit the prognosis of the pregnant women. It is recommended of clinical application.
為此本研究將新產程管理模式應用于產婦分娩,觀察其不同活躍期時限對于兩組產婦的圍術期指標、新生兒分娩后1、5 min的Apgar評分以及妊娠結局與妊娠并發癥發生情況的差異。結果顯示,觀察組產婦產后出血量少于對照組,中轉剖宮產率低于對照組,總產程時間長于對照組,差異有統計學意義(P<0.05);兩組新生兒分娩后5 min的Apgar評分與分娩后1 min的評分、羊水糞染及新生兒窒息發生率比較,差異無統計學意義(P>0.05)。提示新產程管理模式利于改善產婦圍術期指標,且將活躍期>4 h不進展作為活躍期停滯標準時,產婦轉行剖宮產率更低,但對于新生兒評分及并發癥無明顯意義。究其原因在于,新產程管理模式相較于Friedman產程圖而言,其以宮口擴張至6 cm作為活躍期起點,以4 h不進展作為活躍期停滯,要積極尋找原因,將產程時間與活躍期時間充分延長,可顯著降低轉剖宮產率,同時也使產婦有充足的陰道試產時間[12-13]。此外,活躍期停止進展時間>4 h時,可減少分娩產程中的醫療干預,使初產婦分娩過程遵循自然規律,順利經陰道分娩[14-16]。
綜上所述,初產婦采用新產程管理模式有利于改善圍術期指標,且將活躍期>4 h不進展診斷為活躍期停滯標準可顯著降低剖宮產率,促進自然分娩,值得臨床應用推廣。
[參考文獻]
[1]錢夏柳,詹澤森,覃惠鳳.以新產程標準為指導的產程處理對分娩結局的影響研究[J].中國全科醫學,2017,20(15):1845-1848.
[2]趙娜,李娜,蔣小芒,等.新產程標準對產程中臨床指征及母嬰預后的影響[J].現代生物醫學進展,2017,17(27):5362-5364.
[3]諶雯麗,秦豐江,吳慶蓉,等.新產程標準管理下無痛分娩對妊娠結局的影響[J].浙江臨床醫學,2019,21(8):1057-1058.
[4]時春艷,李博雅.新產程標準及處理的專家共識(2014)[J].中華婦產科雜志,2014,23(7):486.
[5]李容芳,徐燕媚,鄧瓊.新產程標準中活躍期拐點在初產婦與經產婦臨床應用中的影響[J].熱帶醫學雜志,2017, 17(7):932-935.
[6]姜麗,曹云桂,張青.持續性剖宮產瘢痕妊娠的臨床特點分析[J].中國計劃生育學雜志,2019,27(1):99-101.
[7]周友芬,郭雅琴,鄧艷華,等.新產程圖產程管理在初產婦中的應用效果[J].中國婦幼保健,2018,33(5):994-996.
[8]孟璐璐,蘇秀娟,花靜,等.產程圖的研究歷程[J].中華圍產醫學雜志,2018,21(11):780-782.
[9]黃秋明,陳暉,梁美娟,等.新產程標準的應用對妊娠結局的影響[J].海南醫學,2017,28(6):989-990.
[10]包菊,赫英東,包艾榮,等.新產程標準下全產程分娩鎮痛對母嬰結局的影響[J].中華圍產醫學雜志,2019,22(2):106-112.
[11]楊小妹,馮小明,張蕾,等.陰道分娩過程中新產程時限管理標準的臨床效果[J].中國婦幼保健,2018,33(7):1504-1506.
[12]葉立.以產程特性比較為基礎的新舊產程標準臨床實踐效果研究[J].檢驗醫學與臨床,2017,14(13):1951-1953.
[13]馬瑤,陳磊,曹冬如,等.實施新產程及催引產指南后剖宮產率及剖宮產指征的變化分析[J].中國生育健康雜志,2017,25(5):468-469,478.
[14]王春芳,王慧敏,歐陽林.新產程標準與助產措施對產鉗助產、中轉剖宮產和新生兒窒息發生率的影響分析[J].醫學臨床研究,2017,34(6):1135-1137.
[15]陸眸清,馮碧波,翟建軍,等.新產程實施對助產、中轉剖宮產及母兒結局的影響[J].中國醫藥導報,2018,15(21):90-93.
[16]劉蘭,王金蓮,張立敏,等.新產程標準下剖宮產后陰道試產239例妊娠結局[J].安徽醫藥,2019,23(5):939-941.
(收稿日期:2019-12-18)

