多烯磷脂酰膽堿聯合谷胱甘肽治療妊娠期肝內膽汁淤積癥患者的效果及對圍產結局的影響
方芳 潘丹 蔡軍波
[摘要] 目的 探討多烯磷脂酰膽堿聯合谷胱甘肽治療妊娠期肝內膽汁淤積癥(ICP)患者的效果及對圍產結局的影響。方法 選取2015年1月~2018年12月ICP患者124例,隨機分為兩組。兩組均予以臥床休息、間斷吸氧、高滲葡萄糖、維生素C及能量合劑等治療。對照組在此基礎上予以多烯磷脂酰膽堿針15 mL靜脈滴注,1次/d;觀察組在對照組基礎上再加谷胱甘肽針2.4 g靜脈滴注,1次/d。兩組均連用2周。觀察兩組治療后臨床癥狀及血清生化指標改善情況,并比較其圍產結局。 結果 治療2周后,兩組瘙癢評分均較治療前顯著下降(P<0.01或P<0.05),且觀察組下降幅度較對照組更明顯(P<0.05);觀察組黃疸和瘙癢消失時間明顯少于或短于對照組(P<0.05)。治療2周后,兩組血清ALT、TBA和AST水平均較治療前明顯下降(P<0.01或P<0.05),且觀察組下降幅度較對照組更明顯(P<0.05)。同時觀察組宮內窘迫、早產和新生兒窒息發生率明顯低于對照組,分娩出血量明顯少于對照組,新生兒體重明顯大于對照組(P<0.05)。 結論 多烯磷脂酰膽堿聯合谷胱甘肽治療ICP患者不僅能明顯改善其臨床癥狀,降低肝酶指標與膽汁酸水平,而且能降低發生不良圍產結局,有利于母嬰安全。
[關鍵詞] 妊娠期肝內膽汁淤積癥;多烯磷脂酰膽堿;谷胱甘肽;圍產結局
[中圖分類號] R714.255? ? ? ? ? [文獻標識碼] A? ? ? ? ? [文章編號] 1673-9701(2020)02-0016-04
Effect of polyene phosphatidylcholine combined with glutathione on patients with intrahepatic cholestasis of pregnancy and its influence on perinatal outcome
FANG Fang1? ?PAN Dan1? ?CAI Junbo2
1.Department of Gynecology, Taizhou Municipal Hospital in Zhejiang Province, Taizhou? ?318000, China; 2.Department of Oncological Surgery, Taizhou Municipal Hospital in Zhejiang Province, Taizhou? ?318000, China
[Abstract] Objective To investigate the effect of polyene phosphatidylcholine combined with glutathione on patients with intrahepatic cholestasis of pregnancy (ICP) and the influence of perinatal outcome. Methods A total of 124 patients with ICP from January 2015 to December 2018 were randomly divided into two groups. Both groups were treated with bed rest, intermittent oxygen, hypertonic glucose, vitamin C and energy mixture. On the basis of this, the control group was given an intravenous infusion of 15 ml of polyene phosphatidylcholine needle once a day. The observation group was treated with an intravenous infusion of 2.4 g of glutathione needle once a day based on the treatment of the control group. Both groups were used for 2 weeks. The improvement of clinical symptoms and serum biochemical parameters of two groups after treatment was observed, and the perinatal outcomes were compared. Results After 2 weeks of treatment, the pruritus scores of the two groups were significantly lower than those before (P<0.01 or P<0.05), and the decrease of the observation group was more significant than that of the control group (P<0.05). The disappearance time of jaundice and itching in the observation group was significantly less than or shorter than that of the control group (P<0.05). After 2 weeks of treatment, the serum levels of ALT, TBA and AST in the two groups were significantly lower than those before treatment (P<0.01 or P<0.05), and the decrease in the observation group was more significant than that in the control group (P<0.05). The incidence of distress, premature delivery and neonatal asphyxia in the observation group was significantly lower than that of the control group. The amount of bleeding after delivery in the observation group was significantly lower than that of the control group, and the weight of the newborn in the observation group was significantly higher than that of the control group(P<0.05). Conclusion Polyene phosphatidylcholine combined with glutathione in the treatment of ICP patients can not only significantly improve their clinical symptoms, reduce liver enzymes and bile acid levels, but also reduce the occurrence of adverse perinatal outcomes, which is conducive to maternal and child safety.
[Key words] Intrahepatic cholestasis of pregnancy of polyene phosphatidylcholine; Glutathione; Perinatal outcome
妊娠期肝內膽汁淤積癥(Intrahepatic cholestasis of pregnancy,ICP)是妊娠中晚期較少見的一種并發癥,主要表現為皮膚瘙癢和黃疸,極易發生胎兒宮內窘迫、死胎、早產等,引起不良圍產結局[1-2]。ICP的病因及發病機制迄今無明確定論,臨床上尚無特效藥物[3-4]。多烯磷脂酰膽堿與谷胱甘肽均是治療ICP的常用藥物,但兩者聯用治療ICP的效果及對圍產結局的影響國內外報道較少[5-6]。本研究分析多烯磷脂酰膽堿聯合谷胱甘肽治療ICP患者的效果及圍產結局的影響,現報道如下。
1 資料與方法
1.1 一般資料
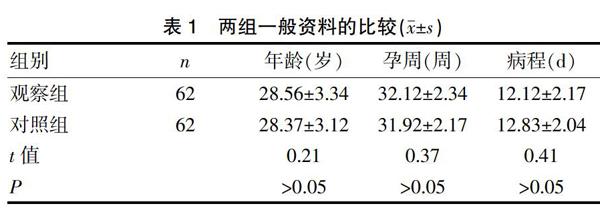
選取2015年1月~2018年12月我院婦產科住院治療ICP患者124例。納入標準[7]:①符合中華醫學會婦產科學分會產科學組制定的《ICP診療指南》中的標準[8];②妊娠中晚期,均為單胎。排除標準[9]:①合并其他妊娠并發癥及全身性疾病者;②以往存在肝膽系統疾病。采用隨機數字表分為兩組各62例。兩組年齡、孕周和病程等比較差異無統計學意義(P>0.05),具有可比性。見表1。
表1? ?兩組一般資料的比較(x±s)
1.2 方法
兩組均予以臥床休息、間斷吸氧、高滲葡萄糖、維生素C及能量合劑等治療。對照組在此基礎上予以多烯磷脂酰膽堿針(北京安萬特制藥有限公司,規格5 mL/232.5 mg,國藥準字J20040114)15 mL+5%葡萄糖靜脈滴注,1次/d。觀察組在對照組基礎上再加谷胱甘肽針(重慶藥友制藥有限責任公司,規格:0.6 g/支,國藥準字H20051600)2.4 g+5%葡萄糖靜脈滴注,1次/d。兩組均連用2周。觀察兩組治療后臨床癥狀及血清生化指標改善情況,并比較其圍產結局。
1.3 觀察指標
1.3.1 臨床癥狀改善情況? 包括瘙癢評分變化、黃疸和瘙癢消失時間。瘙癢評分采用5級評分法[10],分值區間為0~4分,分別為無瘙癢、偶爾瘙癢、輕度不頻繁瘙癢、時斷時續瘙癢及持續無緩解瘙癢。
1.3.2 血清生化指標? 包括谷丙轉氨酶(Alanine transaminase,ALT)、膽汁酸(Total bile acid,TBA)和谷草轉氨酶(Aspartic transaminase,AST)。采用日立7600型全自動生化分析儀進行檢測。
1.3.3 圍產結局? 包括宮內窘迫、早產、新生兒窒息、分娩出血量和新生兒體重等。
1.4 統計學方法
采用SPSS21.0統計學軟件進行分析,計量資料以(x±s)表示,采用t檢驗,計數資料以[n(%)]表示,采用χ2檢驗,P<0.05為差異有統計學意義。
2 結果
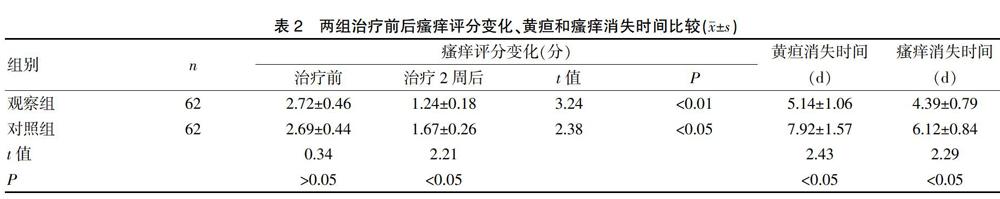
2.1 兩組治療前后瘙癢評分變化、黃疸和瘙癢消失時間比較
治療前兩組瘙癢評分比較,差異無統計學意義(P>0.05);治療2周后,兩組瘙癢評分均較治療前顯著下降(P<0.01或P<0.05),且觀察組下降幅度較對照組更明顯(P<0.05)。觀察組黃疸和瘙癢消失時間明顯少于或短于對照組(P<0.05)。見表2。
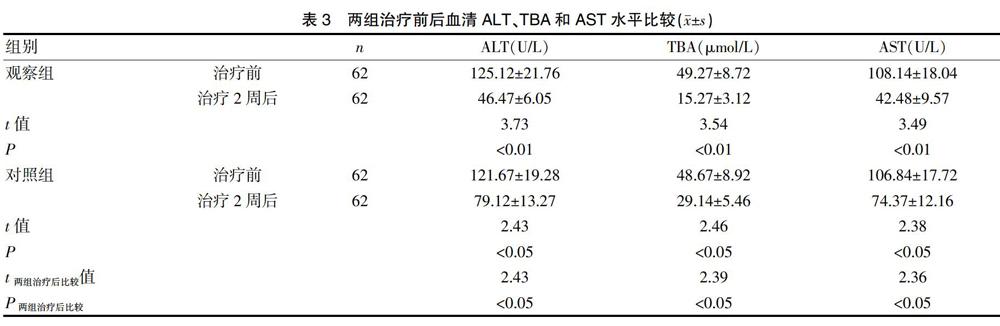
2.2 兩組治療前后血清ALT、TBA和AST水平比較
治療前兩組血清ALT、TBA和AST水平比較,差異無統計學意義(P>0.05);治療2周后,兩組血清ALT、TBA和AST水平均較治療前明顯下降(P<0.01或P<0.05),且觀察組下降幅度較對照組更明顯(P<0.05)。見表3。
2.3 兩組治療后圍產結局比較
觀察組宮內窘迫、早產和新生兒窒息發生率明顯低于對照組,分娩出血量明顯少于對照組,新生兒體重明顯大于對照組(P<0.05)。見表4。
3 討論
ICP是妊娠中晚期特有的非常嚴重的并發癥,主要臨床表現為皮膚瘙癢和黃疸,伴有血膽汁酸升高和肝酶異常,一般在分娩后逐漸消失[11-12]。ICP的發病機制國內外尚未完全闡明,可能與雌性激素過高、肝酶代謝發生異常、免疫異常、遺傳、環境污染等因素密切相關[13-15]。ICP患者本身的預后較好,一般情況下分娩后多種臨床癥狀會自行消退,但其對胎兒具有較嚴重的不良影響。ICP 孕婦由于膽酸代謝發生異常,膽鹽造成小膽管梗阻或膽汁酸發生逆流使膽汁流出受阻形成淤積,使得膽汁酸濃度急劇上升,引起胎盤的正常功能受損,主要危害是引起胎盤絨毛膜靜脈血管收縮,引起血管痙攣,降低胎兒組織器官的血流灌注,紅細胞攜氧量顯著下降,引起胎兒宮內缺氧造成羊水污染、胎兒窘迫甚至早產等嚴重并發癥,增加了不良圍產結局發生率,不利于母嬰安全,增加圍生兒發病率與死亡率,預后較差[16-19]。因此,對ICP患者予積極有效的藥物治療,對降低不良圍產結局具有十分重要的意義。
多烯磷脂酰膽堿是從大豆中的磷脂提煉獲取的,通過二亞油酰磷脂酰膽堿替換內源性磷脂修復受損肝細胞膜及細胞器膜,改善膽汁淤積情況,加快受損肝功能逐漸恢復正常,繼而增強肝細胞膜的流動性,有效調節膜結合酶系統的活性,抑制脂質過氧化,降低氧自由基水平;提升谷胱甘肽還原酶、過氧化氫酶等酶的活性,加快肝臟的排毒能力;同時可將中性脂肪及膽固醇在體內轉換成易代謝分解的方式,改善膽汁淤積情況,加快膽汁的分泌,降低膽汁酸的濃度,減輕膽汁酸及代謝產物對肝臟細胞的影響,減輕肝臟壓力改善肝功能,恢復肝細胞的能量代謝平衡[20-21]。谷胱甘肽是一種代表性的三肽類型化合物,可參與人體內糖代謝和三羧酸的循環過程,使人體獲得更多能量起輔酶作用;還可能激活機體中巰基酶,促進蛋白質、碳水化合物、脂肪的代謝,調節肝細胞膜和細胞器膜的能量代謝;并可結合有毒物質將其轉變成無毒或毒性減少物質;還可通過轉丙氨基或轉甲基作用實現其對肝臟解毒、滅活激素等作用;保護并修復肝細胞,加快膽酸代謝[6]。多烯磷脂酰膽堿與谷胱甘肽的作用機制不同,兩藥聯用具有治療ICP的良好協同增效作用,從而提高治療效果,且不增加藥物的不良反應。本研究顯示治療2周后,觀察組瘙癢評分下降幅度明顯高于對照組,黃疸和瘙癢消失時間明顯少于或短于對照組,且觀察組血清ALT、TBA和AST水平下降幅度較對照組更明顯。提示多烯磷脂酰膽堿聯合谷胱甘肽治療ICP患者能明顯改善其臨床癥狀,降低肝酶指標與膽汁酸水平。同時研究還發現,觀察組的宮內窘迫、早產和新生兒窒息發生率明顯低于對照組,分娩出血量明顯少于對照組,新生兒體重明顯大于對照組。提示多烯磷脂酰膽堿聯合谷胱甘肽治療ICP患者能降低不良圍產結局的發生,有利于母嬰安全。
總之,多烯磷脂酰膽堿聯合谷胱甘肽治療ICP患者不僅能明顯改善其臨床癥狀,降低肝酶指標與膽汁酸水平,而且能降低不良圍產結局的發生,有利于母嬰安全。但納入本次研究的病例數相對較少,必要時增加病例數進行深入研究。
[參考文獻]
[1] Kurtulmu S,Gür EB,Kztekin D,et al. The impact of intrahepatic cholestasis of pregnancy on fetal cardiac and peripheral circulation[J]. J Turk Ger Gynecol Assoc,2015, 16(2):74-79.
[2] Erlinger S. Ursodeoxycholic acid in intrahepatic cholestasis of pregnancy:Good,but can do better[J]. Clin Res Hepatol Gastroenterol,2013,37(2):117-119.
[3] Zhang Y,Pan Y,Lin C,et al. Bile acids evoke placental inflammation by activating Gpbar1/NF-κB pathway in intrahepatic cholestasis of pregnancy[J]. J Mol Cell Biol,2016,8(6):530-541.
[4] Ghosh S,Chaudhuri S. Intra-hepatic cholestasis of pregnancy:A comprehensive review[J]. Indian J Dermatol,2013, 58(4):327-329.
[5] 何國梅. 多烯磷脂酰膽堿對妊娠期肝內膽汁淤積癥的治療效果及對妊娠結局的影響[J]. 中國婦幼保健,2016, 31(24):5301-5304.
[6] 謝鑫,黃曉平,曹曉輝,等. 谷胱甘肽聯合熊去氧膽酸治療妊娠期肝內膽汁淤積癥的效果及對圍產結局的影響[J]. 江蘇醫藥,2018,44(4):444-446.
[7] 楊海艷,胡敏,陳江鴻. 妊娠期肝內膽汁淤積癥孕婦的母兒結局及其影響因素分析[J]. 中華婦產科雜志,2016, 51(7):535-537.
[8] 中華醫學會婦產科學分會產科學組. 妊娠期肝內膽汁淤積癥診療指南(第1版)[J]. 中華婦產科雜志,2011, 46(5):391-395.
[9] 趙丹陽. 熊去氧膽酸與多烯磷脂酰膽堿治療對妊娠期肝內膽汁淤積癥患者妊娠結局及胎兒并發癥的影響[J].中國婦幼保健,2017,32(18):4380-4382.
[10] Garcia-Flores J,Caamares M,Cruceyra M,et al. Clinical value of maternal bile acid quantification in intrahepatic cholestasis of pregnancy as an adverse perinatal outcome predctor[J]. Gynecol Obstet Invest,2015,79(4):222-228.
[11] Covach AJ,Rose WN. Intrahepatic cholestasis of pregnancy refractory to multiple medical therapies and plasmapheresis[J]. AJP Rep,2017,7(4):e223-e225.
[12] Wensink MJ. The risk of infant and fetal death by each additional week of expectant management in intrahepatic cholestasis of pregnancy by gestational age:Various objections[J]. Am J Obstet Gynecol,2016,215(6):807-808.
[13] Joutsiniemi T,Timonen S,Leino R,et al. Ursodeoxycholic acid in the treatment of intrahepatic cholestasis of pregnancy:A randomized controlled trial[J]. Arch Gynecol Obstet,2014,289(3):541-547.
[14] 王海英,徐麗菊. 妊娠期肝內膽汁淤積癥臨床特點與妊娠結局[J]. 浙江預防醫學,2015,21(1):91-92.
[15] Dixon PH,Williamson C. The pathophysiology of intrahepatic cholestasis of pregnancy[J]. Clin Res Hepatol Gastroenterol,2016,40(2):141-153.
[16] 孫璐,李芳,朱啟英. 妊娠期肝內膽汁淤積癥的研究現狀[J]. 新疆醫學,2015,45(3):377-381.
[17] Sanhal CY,Kara O,Yucel A. Can fetal left ventricular modified myocardial performance index predict adverse perinatal outcomes in intrahepatic cholestasis of pregnancy?[J]. J Matern Fetal Neonatal Med,2017,30(8):911-916.
[18] Liu X,Landon MB,Chen Y,et al. Perinatal outcomes with intrahepatic cholestasis of pregnancy in twin pregnancies[J]. J Matern Fetal Neonatal Med,2016,29(13):2176-2181.
[19] 羅一沖,普燕芳. 妊娠期肝內膽汁淤積癥的藥物治療[J].中國當代醫藥,2014,21(6):194-196.
[20] Cao M,Li X,Zhang B,et al. The effect of polyene phosphatidyl choline intervention on nonalcoholic steatohepatitis and related mechanism[J]. American Journal of Research,2016,8(5):2325-2327.
[21] 李永紅,閆芳. 多烯磷脂酰膽堿注射液治療妊娠期肝內膽汁淤積癥的療效觀察[J]. 實用婦產科雜志,2014, 30(6):469-471.
(收稿日期:2019-01-22)

