Bleeding risk assessment in elderly patients with acute coronary syndrome
Lucía Riobóo-Lestón, Sergio Raposeiras-Roubin, Emad Abu-Assi, Andrés I?iguez-Romo
Department of Cardiology, University Hospital álvaro Cunqueiro, Vigo, Spain
Abstract Nowadays, elderly people represent a growing population segment with a well known increased risk of both ischemic and bleeding events. Current acute coronary syndrome guidelines, strongly recommend dual antiplatelet therapy (DAPT) with few specific references for aged patients due to lack of evidence. Patients aged ≥ 75 years are misrepresented in the classic derivation trials cohorts. Strategies to reduce the bleeding risk in this group of patients are urgently needed for the daily clinical practice. Identify the specific age related bleeding risk factors and the importance of an integral geriatric assessment remains challenging. Some of the available in-hospital and out-hospital bleeding risk scores have shown a lower to moderate predictive ability in older patients and no specific tools are developed in elderly population.The importance of an appropriate vascular access choice, type and duration of antiplatelet drugs is crucial to reduce the bleeding risk. Increase radial approaches and short DAPT duration leads to reduce hemorrhages. One interesting subgroup of patients is those who need chronic anticoagulation therapy after percutaneous coronary intervention, due to their very high risk of bleeding. New alternatives as dual therapy with oral anticoagulation and only one antiplatlet drug should be considered. In current review, we evaluate the available evidence about bleeding risk in elderly.
Keywords: Acute coronary syndrome; Bleeding risk; Dual antiplatelet treatment; Elderly patients
1 Introduction
Each year, 17.9 million people die from cardiovascular disease, which is the main cause of loss of quality of life and dependency, especially in elderly people who represent a growing population segment.[1]
Nowadays, the cornerstones of the acute coronary syndrome (ACS) treatment are the new antitrombotic therapies and the percutaneous coronary intervention (PCI), exposing our patients to a higher risk of bleeding. Dual antiplatelet therapy (DAPT) is the standard care in ACS patients underwent PCI.
Elderly patients have been under-represented in the main ACS trials derivation cohorts which makes difficult to extrapolate the available information.[2]Currently, several studies have studied the effectiveness of an invasive strategy in elderly patients.[3-6]Results were controversial, especially in non-ST segment elevation ACS (NSTE-ACS), probably because of the heterogeneous basal characteristics of the groups like the degree of comorbidity or frail. The management of DAPT in elderly people remains challenging,with few specific recommendations in current guidelines,being an important gap of knowledge.[7]
It is known that elderly patients have increased both ischemic and bleeding risk.[8]It could be related to their intrinsic characteristics as: comorbidity, complex coronary disease, physical disabilities and frail. Recent studies have demonstrated that hemorrhagic risk exponentially rise from the seventh decade, increasing mortality, length of hospitalization and costs.[9,10]This is the reason why the evaluation of hemorrhagic risk plays a crucial role when faced the treatment of ACS in elderly patients. The use of bleeding risk scores identifies high risk patients and it helps clinicians to determine the DAPT regime and duration. At the present time, we have in the literature multiple bleeding classifications (Table 1); generating difficulties to compare the avaliable bleeding risk scores.
The aim of this paper is summarizing the available information that it could help the clinicians facing the bleeding risk assessment of elderly people.
2 Factors associated with bleeding risk in elderly
Historically, factors related to the risk of bleeding havebeen identified, some of them closely related to age.Broadly speaking, we could classify them as non modifiable,potentially modifiable and modifiable factors.
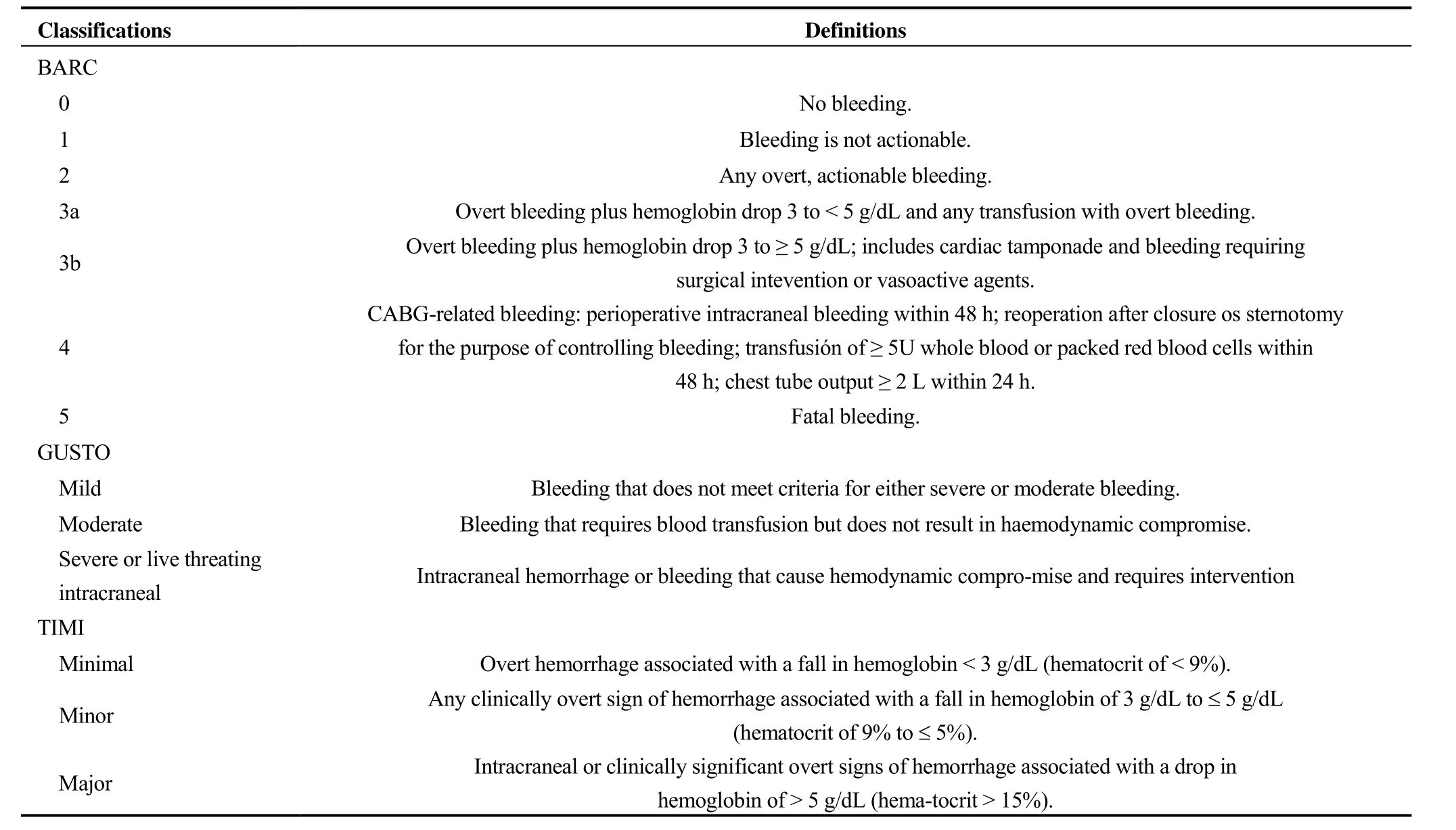
Table 1. Bleeding classifications and definitions.
2.1 Non modifiable
The principal non modifiable bleeding risk factors are age and female sex. Most of them are generally related to patient comorbidity as peripheral arteriopathy, diabetes mellitus, hypertension, stroke, malignancy and previous bleeding.
2.2 Potentially modifiable
Within the potentially modifiable factors, we include those that vary during the time and they may be affected by the medical therapies. For example: anticoagulation, use of chronic steroid or non steroid antiinflammatory drugs, renal function, hemoglobin, and a very frequent finding in elderly patients, trombocytopenia. Patients with thrombocytopenia were excluded from the derivation trials, but there is evidence that the risks of mortality and bleeding correlated directly with the thrombocytopenia severity.[11]
2.3 Modifiable
The modifiable factors are the cornerstone of the bleeding assessment. The type and duration of dual antiplatlet therapy, the invasive management, and the choice of vascular access, favours radia, femoral, are the most relevant ones.[12]
3 Bleeding risk assessment tools
In this section, we will summarize the main available scores in the literature up to the current time. The most relevant limitations of these tools are that the average age of the patients in the referral cohorts does not exceed 70 years old, the use of different bleeding definitions, the different presentation of coronary artery disease, and the heterogeneous clinical management in the studies. As we will see some of them have been specifically studied in elderly patients.
3.1 Inhospital bleeding
As is known that hemorrhagic events increase intra-hospital mortality.[13]Current guidelines recommend the use of bleeding risk scores in ACS patients to predict in-hospital bleeding.[14]The most widespread scores are summarized in Table 2.
Ariza, et al.[15]evaluated the predictive ability of CRUSADE, MEHRAN and ACTION bleeding risk scores in 2,036 consecutive ACS patients aged ≥ 75 years old. Theyfound a consistent lower ability for all of them to predict in hospital major bleeding in this group. The vascular access was the most common location for inhospital bleedings in elderly people, followed by urinary and intracranial, instead of digestive and urinary that they are more common in younger patients. Likewise, Faustino, et al.[16]consistently observed a poor predictive ability of the CRUSADE score in a cohort of patients aged ≥ 80 years with NSTE-ACS.

Table 2. Inhospital bleeding risk scores.
Most of the previously described scores were validate in the pre ticagrelor-prasugrel era, which is not the real clinical practice nowadays. We need further investigation according actual approachess: early invasive PCI strategies, high percentages of radial vascular access, use of fondaparinux and limited glycoprotein IIb/IIIa inhibitors.
3.2 Outhospital bleeding
In recent years, there has been a growing concern about the evaluation of the hemorrhagic risk in the medium-long term. It is known that the scores created for the intrahospital bleeding risk assessment, they have low capacity when predicting bleeding in the extrahospitalary phase.[17]At the time of the newest antiplatlets treatments and last generation stents, knowing the probability of presenting a hemorrhagic event in the follow-up is of great relevance to help us to select the best therapeutic strategy including type and duration of antiplatelet therapy.
Recent DAPT guidelines recommend the use of risk scores to evaluate the benefits and risks of different DAPT durations.[18]Table 3 summarizes the main characteristics of the scores used for the hemorrhagic risk assessment at discharge. As we can see in the derivation cohorts mean and median ages (Table 2), patients older than 75 years are clearly underrepresented, which makes uncertain the application of these tools in an elderly population.
Regarding to PRECISE-DAPT score, a recent study showed no significant differences regarding the incidence of bleeding according to the recommended cutt of point ≥ 25.However, a progressive increase in the incidence of bleeding was observed across PRECISE-DAPT quartiles. These results suggest that the need for adapting of the PRECISE-DAPT score in non-selected elderly patients with ACS for an accurate assessment of bleeding risk.[19]
One recent study also assesed the predictive ability of the BleeMACS score in elderly patients.[20]They analyze 3,376 patients aged ≥ 75 years old, 5.6% presented hemorrhagic events during follow-up with a mean time to the episode shorter than younger patients (134 vs.159 days). There were no differences in the bleeding location being the most frequent gastrointestinal, genitourinary and intracranial. They found moderately-lower ability for predicting out hospital bleeding events in ≥ 75 years old group (0.652 vs. 0.691).So far there are no more studies that specifically evaluate the hemorrhagic risk in elderly patients with ACS.
4 Role of integral geriatric assessment in hemorrhagic risk stratification
Due to the specific characteristics and complexity of the elderly patients, the need of a comprehensive geriatric assessment in the ACS has been studied in the last years. The integral geriatric assessment is a dynamic and structured diagnostic process including functional, clinical, mental and social valoration in order to optimize resources and achieve the highest degree of independence and quality of life.
Nowadays, there are controversial findings about the usefulness of parameters such frailty to assess the risk of bleeding in the ACS. In the insights from the LONGEVO-SCA registry, Ariza, et al.[21]explored the role of acomprehensive geriatric assessment to predict in-hospital bleeding. Geriatric assessment included: functional capacity for basic activities of daily living (Barthel index), cognitive status (Pfeiffer test), frailty (Frail scale), comorbidity (Chalson index) and nutritional risk assessmenet (MNA-SF).They found from all of previous age-related variables, only comorbidity was significantly associated with in hospital major bleeding (MB). In the same way, White, et al.[22]in a substudy of TRILOGY ACS, they found that it is no association between frailty defined by Fried criteria and bleeding. On the other hand, Alonso Salinas, et al.[23]have done a study to determine if frailty measured by SHARE-FI index increases bleeding risk in patients with ACS. They included 190 patients ≥ 75 years old. 37.9% were categorized like frail patients. On multivariate analysis, frailty was an independent predictor for MB.
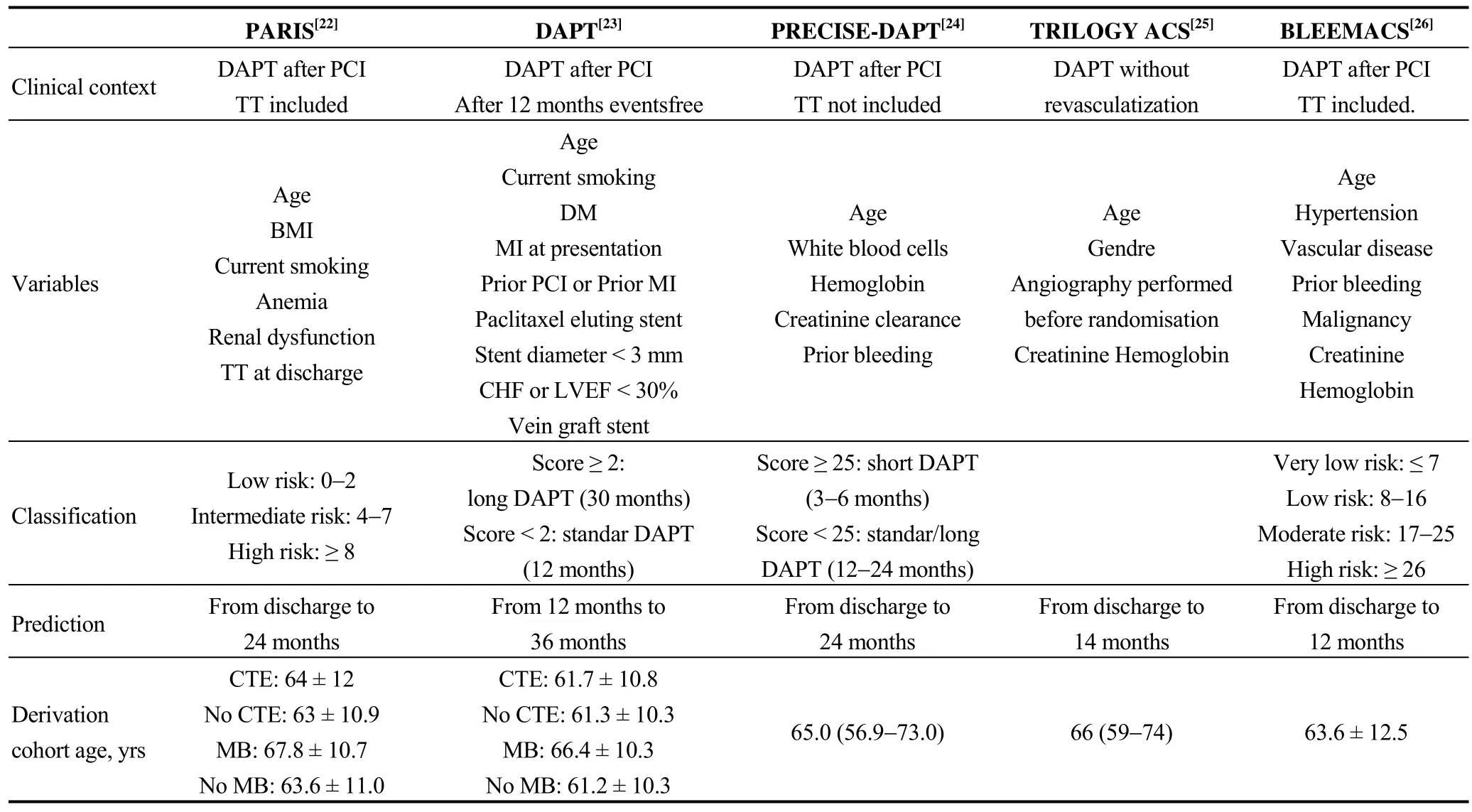
Table 3. Outhospital bleeding risk scores.
Some explanations for these different findings could be the use of different index to measure fragility and hemorrhagic events, it also maks them difficult to compare.
4.1 Antitrombotic teraphy
Current guidelines general recommend 12 months of DAPT in ACS patients but it emphasized on the importance of individualize according hemorrhagic risk, it being able to choose short patterns of DAPT(3-6 months) in patients at high bleeding risk.[24]The management of DAPT in elderly people remains challenging and we have little specific recommendations in guidelines.[25,26]Recent trials in old people using drug eluting stents with biodegradable polymers and short DAPT duration shows to reduce the risk of bleeding events with no significant increase of ischemic complications.[27,28]
Age-related organ changes affect to drug pharmacokinetics and pharmacodynamics.[29]The decrease in intestinal absorption, hepatic metabolism, body mass index, free water and muscle mass as well as the increase in fat, influences drugs efficacy and safety in this group of patients.
4.2 Chronic oral anticoagulation
Triple therapy (TT) is the standard care in patients with ACS ongoing to PCI and atrial fibrillation (AF). It is known that this strategy can triple the risk of bleeding.[30]Sambola,et al.[31]analyzed the efficacy and safety of TT in patients ≥75 years old with atrial fibrillation undergoing PCI in one study. They found lower thromboembolism rate in TT group than in DAPT one (0.6 % vs. 6.9%) but at the expense of increased MB events (11.7 % vs. 2.4%).
Current guidelines recommend different strategies depending if the main concern is the ischemic or the hemorrhagic events and propose strategies to reduce the risk in anticoagulated patients including: use of HAS-BLED score,shorten the time of DAPT considering oral anticoagulation and clopidogrel instead of triple therapy in high bleeding risk patients, use of dircet oral anticoagulants (DOACs)over vitamin K antagonists (VKA), if VKA is need consider a lower target international normalized ratio (INR), use less than 100 mg daily atomic absorption spectrometry (AAS)and routine use of proton pump inhibitors (PPIs). The DAIGA score system (DAPT continuation, age > 75 years,INR > 2.2, gastrointestinal ulcer history, Anemia) proved usefullness for predicting bleeding complications and risk stratification of AF patients after drug-eluting stent (DES)implantation with triple antithrombotic therapy (TAT). The score showed better predictive ability for bleeding complications than the HAS-BLED score in this context.[32]
In a recent meta analisis, Cavallalri, et al.[33]includes 6036 patients from four controlled randomized trials (ISAR TRIPLE, PIONER AF-PCI, RE-DUAL-PCI and WOEST)with chronic oral anticoagulation indication after PCI. They conclude that in these patients dual antithrombotic therapy compared with TT, it reduces bleeding events without significant increased in ischemic events.
5 Conclusions
Age is an independent risk factor for bleeding. The management of ACS in this group of patients is challenging because they are misrepresented in trials and the evidence is scarce. The identification of different bleeding risk factors and bleeding risk assessment tools can help the clinician to optimize the therapeutic decisions. Few bleeding scores were validated in elderly population who parodoxically constitutes one of the higher bleeding risk groups. Despite the appearance of new antiplatelet treatments as well as strategies to reduce the hemorrhagic events in high risk patients (short term DAPT or dual therapy post PCI in patients’ requirig chronic anticoagulation), further investigation is needed in all these fields for elderly population.
Acknowledgments
All authors report no conflicts of interest.
 Journal of Geriatric Cardiology
2019年2期
Journal of Geriatric Cardiology
2019年2期
- Journal of Geriatric Cardiology的其它文章
- Removal of refractory thrombus by 5F child catheter in patients with subacute myocardial infarction
- A rare case of primary well-differentiated angiosarcoma of the right atrium
- Impact of main vessel calcification on procedural and clinical outcomes of bifurcation lesion undergoing provisional single-stenting intervention:a multicenter, prospective, observational study
- Frailty and acute coronary syndrome: does gender matter?
- Frailty in patients admitted to hospital for acute coronary syndrome: when,how and why?
- Clinical and prognostic implications of delirium in elderly patients with non–ST-segment elevation acute coronary syndromes
