Hand-assisted laparoscopic splenectomy is a useful surgical treatment method for patients with excessive splenomegaly: A metaanalysis
Yong Huang, Xiao-Yun Wang, Kai Wang
Abstract BACKGROUND Hand-assisted laparoscopic splenectomy (HALS) can help overcome the drawbacks of laparoscopic splenectomy (LS) while maintaining its advantages.AIM To evaluate the efficacy and advantages of HALS for splenomegaly.METHODS The relevant literature was reviewed using the PubMed, EMBASE, Cochrane,Ovid Medline, and Wanfang databases to compare the clinical outcomes of HALS and LS. Odds ratios or mean differences were calculated with 95% confidence intervals for fixed-effects and random-effects models. Overall, 754 patients from 16 trials who met the inclusion criteria were selected.RESULTS In pure splenectomy, blood loss volume (P < 0.001) and conversion rate (P =0.008) were significantly lower in the HALS group than in the LS group.Conversely, for splenomegaly, the operative time (P = 0.04) was shorter and blood loss volume (P < 0.001) and conversion rate (P = 0.001) were significantly lower in the HALS group than in the LS group. However, no significant difference was observed in hospital stay length, blood transfusion, time to food intake, complications, or mortality rate between the two groups. Moreover, in splenectomy and devascularization of the upper stomach (DUS), the operative time (P = 0.04) was significantly shorter and blood loss volume (P < 0.001) and conversion rate (P = 0.05) were significantly lower in the HALS + DUS group than in the LS + DUS group. However, no significant difference was observed in hospital stay length, timing of diet, and complications between the two groups.CONCLUSION HALS is an ideal surgical treatment method for splenomegaly because it can maximize the benefits for patients while maintaining the advantages of LS.
Key words: Hand-assisted; Laparoscopic; Splenectomy; Splenomegaly; Devascularization
INTRODUCTION
With the high incidence of chronic hepatitis B and C infections worldwide, portal hypertension secondary to liver cirrhosis is common[1-3]. Hypersplenism and splenomegaly, which are common major complications of liver cirrhosis, occur in approximately 24%-80% of cases[4,5]. Splenomegaly is associated with a great challenge in spleen retrieval during splenectomy due to dense adhesions and increased tissue vascularity, which often suggests a need for longer incision to retrieve the specimen.With rapid technological advancement in laparoscopic surgery, laparoscopic splenectomy (LS) has been proven safe and effective[6-8]. The advantages of LS over open splenectomy (OS) include less trauma, quicker recovery, and less postoperative pain[9-11]. However, patients with splenomegaly often exhibit a combination of signs and symptoms, such as hypersplenism, frequent coexistence of varices and thickening, perisplenic collateral vessel distortions, splenomegaly due to limited space of abdominal cavity, and thrombocytopenia, all of which can increase the risk of intraoperative hemorrhage and lead to conversion to open splenectomy[12,13]. Not all patients who need splenectomy benefit from LS owing to the disadvantages of laparotomy, including limited operating field, tactile feedback, and hand-eye coordination[14]. Moreover, with the increasing demand for safe and effective surgical treatment, hand-assisted LS (HALS) is preferred by most people because it has the advantages of both laparotomy and laparoscopy.
Because of these various contradictions, selecting an ideal surgical approach and maximizing its benefits for patients with splenomegaly are essential. However,previous studies have presented inconsistent results[11,14-16]due to the lack of data and group discussions during meta-analysis[16]. Additionally, some surgeons do not prefer HALS because they believe that it is a regressive surgical technique. Therefore, the present study was conducted to further divide pure splenectomy, splenomegaly, and splenectomy plus devascularization of the upper stomach (DUS) into three subgroups and evaluate the safety and feasibility of HALS compared to LS.
MATERIALS AND METHODS
Literature search
A systematic search of the literature was conducted in the PubMed, EMBASE,Cochrane, Ovid Medline, and Wanfang databases using the following keywords:hand assisted, hand port, laparoscopic, and splenectomy. The search included articles published between the dates of the creation of the electronic resources and January 20,2018. In addition, the reference lists of selected papers and systematic reviews were searched for potentially relevant studies missed out during the original search.Eligible studies were independently selected by two reviewers and any disagreements on article inclusion between the two were resolved by discussion with a third reviewer. This study protocol followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement and the Cochrane Handbook for Diagnostic Test Accuracy Reviews. Institutional review board approval and patient consent were waived because of the nature of this study. The Newcastle-Ottawa Scale was used to assess the quality of studies[17], and a star system (range, 0-9 stars) was developed for the evaluation (Table 1). The study was approved by the Ethics Committee.
Inclusion and exclusion criteria
All case-control studies that compared HALS and LS were selected. The inclusion criteria were patients with no requirement of additional procedures, no history of upper laparotomy, and a history of splenectomy (including malignant, benign, and normal results). In addition, the included studies must have reported data on sex,spleen weight (in kg), body mass index (BMI), maximum diameter (in cm),malignancy, blood transfusion, conversion rate, mortality rate, total morbidity,operative time (in min), hospital stay length (in days), blood loss volume (in ml), or the time to food intake (in days).
We excluded the following articles: articles that did not report outcomes, editorials,review studies, and animal studies. Neither authorship nor publisher information influenced the inclusion of articles.
Statistical analysis
Statistical analyses were performed using Review Manager version 5.1 (RevMan,Cochrane Collaboration, Oxford, United Kingdom). The results of this meta-analysis are expressed as the odds ratios (ORs) for dichotomous data and mean differences(MDs) for continuous data, with 95% confidence intervals (CIs) for both. The inverse variance method was used for continuous variables, whereas the Mantel-Haenszel method was used for dichotomous variables. Statistical heterogeneity was evaluated using the χ2test. P < 0.05 was considered statistically significant. If heterogeneity was significant, we used the random-effects model; otherwise, we used the fixed-effects model. If data were reported as median and range rather than mean and SD, the mean and SD were estimated as previously described[18,19].
RESULTS
Study selection and characteristics
The search process and the selection of relevant studies are presented in Figure 1. In total, 16 trials were analyzed[11,14,20-33](Table 1) involving 754 patients who met the criteria. There were 11 trials for pure splenectomy[11,14,20-28]involving 573 patients that compared HALS and LS, 9 trials for splenomegaly[11,14,20-22,24-26,28]involving 486 patients that compared HALS and LS, and 5 trials[29-33]involving 181 patients that compared HALS + DUS and LS + DUS.
HALS vs LS for pure splenectomy
There were 11 trials for splenectomy involving 573 patients that compared HALS and LS. The splenic weight in the HALS group was significantly greater than that in the LS group (MD: 0.82, 95%CI: 0.18-1.47; P = 0.01; Figure 2D). In addition, the maximum diameter of the spleen (MD: 2.68, 95%CI: 0.94-4.42; P = 0.002; Figure 2F) in the HALS group was significantly greater than that in the LS group. However, no significant difference was observed in the BMI (MD: 0.45, 95%CI: -0.32 to 1.22; P = 0.25; Figure 2A) between the two groups.
Blood loss volume (MD: -63.07, 95%CI: -86.23 to -39.90; P < 0.001; Figure 2B) and conversion rate (OR: 0.34, 95%CI: 0.15-0.75; P = 0.008; Figure 3D) were significantly lower in the HALS group than in the LS group. However, no significant difference was observed in the operative time (MD: -22.12, 95%CI: -52.33 to 8.09; P = 0.15; Figure 2E), hospital stay length (MD: 0.04, 95%CI: -1.28 to 1.35; P = 0.96; Figure 2G), blood transfusion (OR: 0.82, 95%CI: 0.44-1.54; P = 0.54; Figure 3B), time to food intake (MD: -0.09, 95%CI: -0.21 to 0.04; P = 0.18; Figure 2C), complications (OR: 0.95, 95%CI: 0.45-1.99; P = 0.88; Figure 3A), or mortality rate (OR: 0.65, 95%CI: 0.21-1.542.07; P = 0.47;Figure 3C) between the two groups.
HALS vs LS for splenomegaly

Table 1 Description of included studies
There were 9 trials for splenectomy involving 486 patients that compared HALS and LS. There was no significant difference in the splenic weight (MD: 0.60, 95%CI: -0.12 to 1.32; P = 0.1; Figure 4C) or BMI (MD: 0.71, 95%CI: -0.16 to 1.58; P = 0.11; Figure 4A)between the two groups.
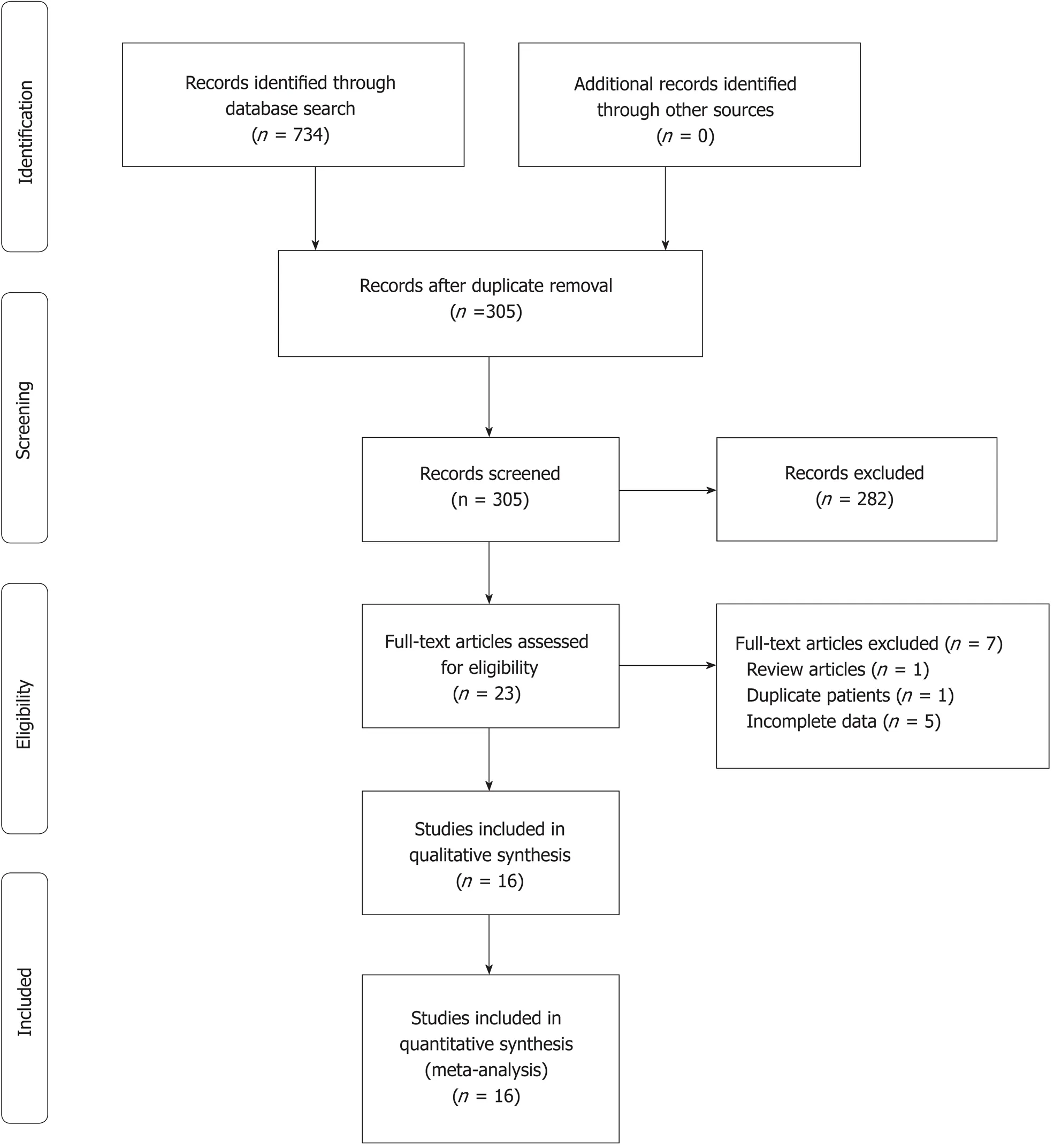
Figure 1 Flow diagram of study selection.
The operative time (MD: -32.74, 95%CI: -63.32 to -2.17; P = 0.04; Figure 4E) was significantly shorter and blood loss volume (MD: -65.13, 95%CI: -88.36 to -41.89; P <0.001; Figure 4D) and conversion rate (OR: 0.23, 95%CI: 0.09-0.56; P = 0.001; Figure 5D) were significantly lower in the HALS group than in the LS group. However, no significant difference was observed in hospital stay length (MD: -0.39, 95%CI: -1.69 to 0.9; P = 0.55; Figure 4G), blood transfusion (OR: 0.51, 95%CI: 0.24-1.12; P = 0.09; Figure 5B), time to food intake (MD: -0.1, 95%CI: -0.23 to 0.02; P = 0.11; Figure 4B),complications (OR: 0.76, 95%CI: 0.31-1.88; P = 0.55; Figure 5A), or mortality rate (OR:0.54, 95%CI: 0.20-2.02; P = 0.45; Figure 5C) between the two groups.
HALS + DUS vs LS + DUS
There were 5 trials for splenectomy involving 181 patients that compared HALS +DUS and LS + DUS. No significant difference was observed in the splenic weight(MD: 139.51, 95%CI: -37.35 to 316.36; P = 0.12; Figure 6F) between the two groups.
The operative time (MD: -36.56, 95%CI: -72.24 to -0.88; P = 0.04; Figure 6D) was significantly shorter and blood loss volume (MD: -85.77, 95%CI: -127.31 to -44.22; P <0.001; Figure 6B) and conversion rate (OR: 0.12, 95%CI: 0.01-1.02; P = 0.05; Figure 6E)were significantly lower in the HALS + DUS group than in the LS + DUS group.However, no significant difference was observed in hospital stay length (MD: 0.35,95%CI: -0.32 to 1.02; P = 0.31; Figure 6G), time to food intake (MD: -0.02, 95%CI: -0.54 to 0.5; P = 0.94; Figure 6C), or complications (OR: 0.73, 95%CI: 0.30-1.75; P = 0.48;Figure 6A) between the two groups.
Publication bias

Figure 2 Forest plots of meta-analysis for pure splenectomy. The BMI (A), blood loss volume (B), time to food intake (C), splenic weight (D), operative time (E),maximum diameter (F), and hospital stay length (G). HALS: Hand-assisted laparoscopic splenectomy; LS: Laparoscopic splenectomy.
Significant heterogeneity was found with regard to splenic weight and blood loss volume. However, no significant heterogeneity was found with regard to operative time and conversion rate. There was no significant publication bias. The combined results are highly reliable.
DISCUSSION
With the high incidence of chronic hepatitis B and C infections worldwide, a large number of patients develop portal hypertension secondary to liver cirrhosis, which indicates a need for splenectomy treatment[1-3]. There is an increasing concern about the safety of the operation while ensuring minimally invasive surgery. LS is considered a standard treatment and has numerous advantages[6-8]; however, it presents greater risks, such as longer operative time, more blood loss, and higher conversion rate owing to the lack of haptic feedback and impaired hand-eye coordination, particularly for splenomegaly[16,20,24]. Fortunately, HALS, first described in 1995[34], can overcome these drawbacks and has become an alternative to LS while maintaining the advantages of LS and OS[16,35]. Because HALS has not been widely recognized and accepted, this study was conducted. The results revealed that HALS should be the preferred choice of treatment for splenectomy or splenectomy + DUS despite the presence of splenomegaly.
This study demonstrated that either with pure splenectomy or splenomegaly,HALS exhibited better advantages than LS. Moreover, for splenectomy + DUS, the operative time was significantly shorter and blood loss volume and conversion rate were significantly lower in the HALS + DUS group than in the LS + DUS group. No significant difference was observed in hospital stay length, time to food intake, or complications between the two groups. HALS requires the chief surgeon to place one hand in the abdominal cavity while maintaining the pneumoperitoneum to improve the accuracy of manipulation by direct tactile sense. By maintaining tactile feedback and hand-eye coordination, the surgeon can bluntly dissect adhesion around the spleen and encircle the splenic pedicle and the space beneath the tail of the pancreas with the hand in the abdominal cavity[36]. This step, together with the preventive ligation of the splenic artery, will limit the result of any possible injury that might occur during the operation because the surgeon would be able to control the splenic pedicle with his or her fingers at any time[36]. Bagging these enlarged spleens is easy with hand, thus reducing operative time. After all, the surgeon’s hand is more reliable than any laparoscopic instrument. The results from this study demonstrated that for pure splenectomy, blood loss volume and conversion rate were significantly lower in the HALS group than in the LS group even though the splenic weight and maximum diameter were significantly greater in the HALS group than in the LS group. For patients with splenomegaly, the operative time was significantly shorter and blood loss and conversion rate were significantly lower in the HALS group than in the LS group, whereas no significant difference was observed in the splenic weight between the two groups. As the splenic weight or size increases, the laparoscopic approach gets more difficult. With the aid of the hand in the abdominal cavity, HALS is facilitated and can be accomplished faster and more safely. Therefore, it was not surprising for patients undergoing HALS to have shorter operative time and lower blood loss volume than patients undergoing LS, as shown in the present study. For open conversion patients, massive intraoperative hemorrhage was the main concern based on the first-hand experience. When uncontrolled bleeding occurred, all operations focused more on the rapid control of bleeding, disregarding other problems, which causes a potential threat to patients. However, in HALS, this surgical uncertainty is reduced. Bleeding is easily controlled through the compression of the splenic vascular pedicle by the left hand, thereby reducing blood loss and conversion rate. In addition, HALS has a shorter learning curve[37]and was performed with fewer trocars and less assistance compared with LS. These advantages have greatly reduced the patient’s financial burden.
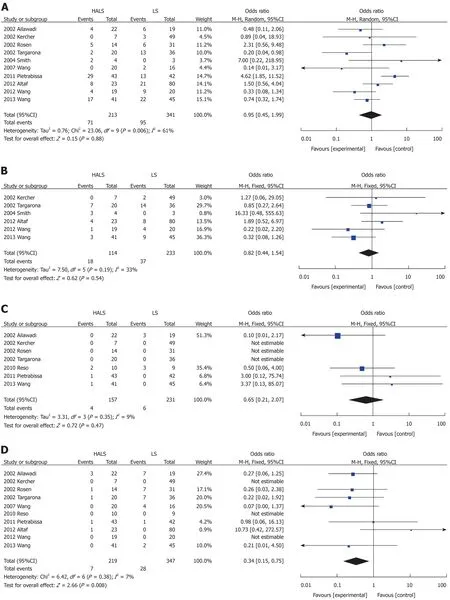
Figure 3 Forest plots of meta-analysis for pure splenectomy. Complications (A), blood transfusion (B), mortality rate (C), and conversion rate (D). HALS: Handassisted laparoscopic splenectomy; LS: Laparoscopic splenectomy.
Despite these advantages, the results from this study also show that no significant difference was observed in hospital stay length, blood transfusion, timing of diet,complications, or mortality rate between the two groups. These indicated that there was no difference in the recovery speed between the two groups. Both the HALS and LS groups have a 5-cm length accessory incision; however, the incidence of surgical trauma is lower in the HALS group than in the LS group. In the LS group, the incision was made at the end of the operation for spleen retrieval. However, in the HALS group, the incision was made at the beginning of the operation for hand-assisted port placement. Based on the above results, HALS not only maintained the advantages of LS and OS but also overcame the disadvantages of LS and OS, resulting in the perfect combination of minimally invasive surgery and surgical safety.

Figure 4 Forest plots of meta-analysis for splenomegaly. The BMI (A), time to food intake (B), splenic weight (C), blood loss volume (D), operative time (E),maximum diameter (F), and hospital stay length (G). HALS: Hand-assisted laparoscopic splenectomy; LS: Laparoscopic splenectomy.
From a technical point of view, the main challenges of HALS are as follows: (1) the hand-assisted incision should be chosen based on the criteria, such as well-exposed tissue, easy operation, minimal tissue trauma, and easy-to-convey laparotomy; (2)hand-assisted device incision and position of puncture design must be considered. It is necessary to avoid piercing using a hand-puncturing device and also to provide a space for the left hand; (3) the nondominant hand of the surgeon is easily fatigued during long-term surgical operation. The spleen and stomach ligament should be separated from top to bottom. This method easily prevents hand fatigue and provides a good field of vision at the same time; (4) in regard to splenic blood vessel treatment,prevention of bleeding is the focus of splenectomy. The main vessels, including splenic vessels of the lower pole and short gastric vessels of the upper edge of the spleen, and splenic pedicles need to be treated. If the splenic pedicle is close to the hand-assisted incision, it is blocked and double-tied with Sadin’s forceps after removing the hand-assisted device; and (5) LigaSure, ultrasonic scalpel, Endo GIA,and other equipment are used to simplify the operation, reduce intraoperative bleeding, reduce the difficulty of surgery, shorten the operative time, and improve the safety of the surgery. Hand-assisted laparoscopic technique can be implemented for a difficult laparoscopic procedure and has been verified in various complicated laparoscopic operations[38], including gastrointestinal cancer surgeries[39,40],pancreatectomies[41,42], nephrectomies[43,44], and hepatectomies[45]. In the case of splenomegaly, the spleen was difficult and sometimes impossible to dissociate using complete laparoscopy due to limited visualization of this area owing to the large spleen size. For HALS, these attachments can usually be severed by blunt finger dissection even in areas that are hidden from the endoscopic view because of the retained tactile feedback[28].
In conclusion, this study demonstrates that HALS can significantly benefit patients with splenomegaly while maintaining the advantages of LS and tactile sense of OS.Moreover, it improves the safety of surgery and is thus considered as a good alternative.
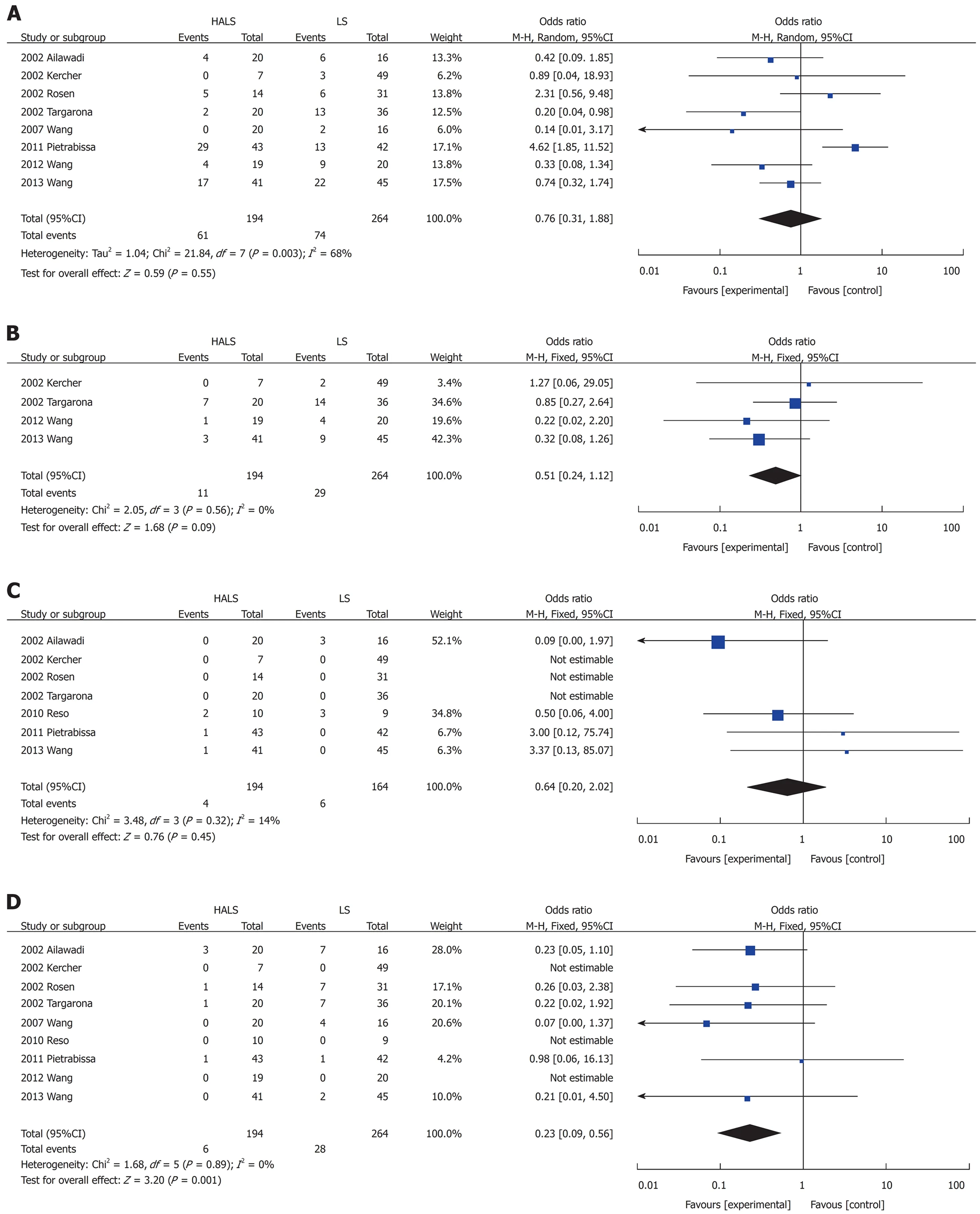
Figure 5 Forest plots of meta-analysis for splenomegaly. Complications (A), blood transfusion (B), mortality (C), and conversion rate (D). HALS: Hand-assisted laparoscopic splenectomy; LS: Laparoscopic splenectomy.
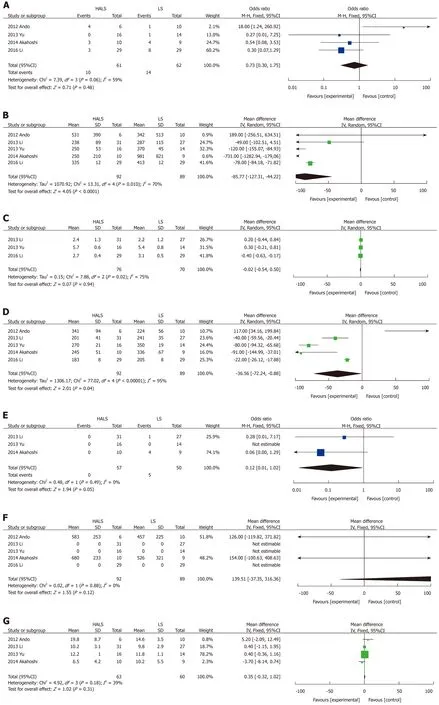
Figure 6 Forest plots of meta-analysis for splenectomy and devascularization of the upper stomach. Complications (A), blood loss volume (B), time to food intake (C), operative time (D), conversion rate (E), splenic weight (F), and hospital stay length (G). HALS: Hand-assisted laparoscopic splenectomy; LS: Laparoscopic splenectomy.
ARTICLE HIGHLIGHTS
Research background
Hand-assisted laparoscopic splenectomy (HALS) can help overcome the drawbacks of laparoscopic splenectomy (LS) while maintaining its advantages, but it has not been widely accepted.
Research motivation
To compare the advantages and disadvantages of HALS and LS.
Research objectives
This study evaluated the efficacy and advantages of HALS for splenomegaly.
Research methods
The relevant literature was reviewed using the PubMed, EMBASE, Cochrane, Ovid Medline, and Wanfang databases to compare the clinical outcomes of HALS and LS. Odds ratios or mean differences were calculated with 95% confidence intervals for fixed-effects and random-effects models.
Research results
In pure splenectomy, blood loss volume and conversion rate were significantly lower in the HALS group than in the LS group. Conversely, for splenomegaly, the operative time was significantly shorter and blood loss volume and conversion rate were significantly lower in the HALS group than in the LS group. However, no significant difference was observed in hospital stay length, blood transfusion, time to food intake, complications, or mortality rate between the two groups. In addition, in splenectomy and devascularization of the upper stomach (DUS), the operative time was significantly shorter and blood loss volume and conversion rate were significantly lower in the HALS + DUS group than in the LS + DUS group. However, no significant difference was observed in hospital stay length, time to food intake, or complications between the two groups.
Research conclusions
HALS is an ideal surgical treatment for splenomegaly because it can maximize the benefits for patients while maintaining the advantages of LS.
Research perspectives
Definite protocol or guidelines should be established using reliable studies with good design. In the future, a well-designed prospective randomized study or multicenter cohort study is mandatory to elucidate the safety and feasibility of HALS.
 World Journal of Clinical Cases2019年3期
World Journal of Clinical Cases2019年3期
- World Journal of Clinical Cases的其它文章
- Biventricular pacing for treating heart failure in children: A case report and review of the literature
- Gerstmann-Str?ussler-Scheinker disease: A case report
- Considerations for routine coagulation monitoring with rivaroxaban:A case report and review of the literature
- Castleman disease presenting with jaundice: A case report and review of literature
- Papillary cystadenoma of the parotid gland: A case report
- Ghost cell odontogenic carcinoma of the jaws: Report of two cases and a literature review
