術前應用氯胺酮對乳腺癌患者術后慢性疼痛發生率的影響
周煦燕,孔敏,姜黎珊,沈徐,陸雅萍,姚明,黃兵
(浙江嘉興市第一醫院麻醉科,314000)
·論著·
術前應用氯胺酮對乳腺癌患者術后慢性疼痛發生率的影響
周煦燕,孔敏,姜黎珊,沈徐,陸雅萍,姚明,黃兵
(浙江嘉興市第一醫院麻醉科,314000)
目的觀察超前應用NMDA受體拮抗劑氯胺酮對乳腺癌術后慢性疼痛發生率的影響。方法ASA I或Ⅱ級全身麻醉下乳腺癌改良根治手術患者160例,采用隨機數字表法將患者隨機均分為N組(單純全身麻醉組)和K組(全身麻醉+氯胺酮組)。記錄患者術前1天、麻醉蘇醒后即刻、術后24 h、48 h機械痛敏程度;采用視覺模擬評分法(VAS)評估患者術前1天、麻醉蘇醒后即刻、術后24 h、48 h、2個月疼痛程度并統計兩組慢性疼痛發生率;根據患者自行按壓的患者自控鎮痛(PCA)次數,計算術后芬太尼需要量。結果術前兩組健患側痛閾及VAS評分測定差異無統計學意義,N組蘇醒即刻健側及患側痛閾較術前明顯降低,術后24 h及48 h健側痛閾與術前無顯著差異,K組健側術后各時間點痛閾較術前無明顯差異,兩組患者蘇醒即刻及術后24 h患側痛閾雖然較術前都降低,但K組痛閾明顯比N組高,差異有統計學意義(Plt;0.05),術后48 h兩組患側痛閾差異無統計學意義(Pgt;0.05);患者術前VAS 評分均為0分,術后即刻及術后24 h K組比N組低,差異有統計學意義(Plt;0.05),術后PCIA的按壓次數及芬太尼使用量K組比N組明顯減少,差異有統計學意義(Plt;0.05);術后K組慢性疼痛發生率比N組明顯降低,差異有統計學意義(Plt;0.05)。結論麻醉誘導期給予氯胺酮能有效提高術中應用瑞芬太尼乳腺癌改良根治患者術后痛閾,降低了乳腺癌患者的慢性疼痛的發生率。
乳腺腫瘤;氯胺酮;慢性疼痛;痛閾
慢性疼痛是一個世界范圍的惡性疾病。是慢性病患者自殺和致殘的主要原因之一[1-3]。盡管近年來鎮痛藥物和方法都在不斷改進,但乳腺癌根治術后一年內慢性疼痛的發生率仍高達30%~55%。此外還伴隨麻木,肢體僵硬無力等其他癥狀。術后慢性疼痛所致的應激與負性情緒反應可對患者造成嚴重的身心傷害,但目前其發生機制尚不清楚,治療效果亦不理想,因此改善術后慢性疼痛的治療現狀,對于改善預后、提高患者術后的生活質量具有積極意義。
1 對象與方法
1.1 研究對象 連續納入2014年6 月1 日至2016年11月30 日在我院行擇期乳腺癌改良根治手術患者160例作為研究對象,采用隨機數字表法將患者平均分為兩組:單純全身麻醉組(N組)、全身麻醉+氯胺酮組(K組)。納入標準:全身麻醉下行擇期手術患者,年齡18~60歲,ASA分級Ⅰ-Ⅱ級。排除標準為:術前檢查發現肝、胰腺、腎功能異常;體質量指數gt;28 kg/m2的肥胖患者;合并糖尿病、甲亢等代謝性疾病;有嚴重的心血管病史;酗酒或吸毒史以及精神疾病或癲癇史;近1個月內接受過全身麻醉者;無法根據患者提供的聯系方式與之取得聯系的患者;未獲得知情同意患者;認知功能異常患者;無法用語言準確溝通患者;惡性腫瘤術后已明確診斷復發或轉移者,不能充分理解問卷內容致調查不能完成及病歷資料不全者。本研究經醫院倫理委員會批準同意。
1.2 方法 所有患者術前禁飲食8 h,入手術室后常規監測無創血壓、血氧飽和度、心電圖、脈搏與腦電雙頻指數(BIS)。開放靜脈后,靜脈注射丙泊酚(江蘇海慈生物藥業有限公司生產)2 mg/kg,瑞芬太尼(江蘇恩華藥業股份有限公司生產)1.5 μg/kg,羅庫溴銨(浙江仙琚制藥股份有限公司生產)0.6 mg/kg。靜脈注射羅庫溴銨1.5 min后行氣管插管。插管后FiO250%機械通氣,維持ETCO235~45 mm Hg,行橈動脈或足背動脈穿刺監測血流動力學指標。術中持續輸注瑞芬太尼與吸入七氟烷(上海恒瑞醫藥有限公司生產)維持麻醉。七氟烷初始呼氣末濃度為2%,根據BIS值與血流動力學參數調節七氟烷吸入濃度,當BIS值大于60、平均動脈壓較誘導前升高超過20%或心率上升超過15%提高七氟烷吸入濃度,每次調節幅度為0.5%;當平均動脈壓低于70 mm Hg或BIS值小于30時降低七氟烷吸入濃度;當出現持續低血壓降低七氟烷濃度無法糾正或BIS值大于60時給予去氧腎上腺素維持循環穩定。每間隔40 min追加羅庫溴銨0.1 mg/kg維持肌松。術中靜滴乳酸鈉林格液(陜西濟生制藥有限公司生產)與羥乙基淀粉130/0.4氯化鈉注射液(連云港潤眾制藥有限公司生產)補充血容量,血紅蛋白含量小于80 g/L時輸注濃縮紅細胞。K組在全身麻醉誘導前靜脈注射氯胺酮(江蘇恒瑞醫藥股份有限公司生產)1 mg/kg,其余K組與N組相同。手術結束時停用瑞芬太尼與七氟烷,送麻醉恢復室,術后常規使用電子泵,行枸櫞酸芬太尼(江蘇恩華藥業股份有限公司生產)PCIA(10 μg/mL,100 mL),待患者清醒后拔除氣管導管送返病房。
1.3 觀察指標 采用電刺激儀(日本光電公司,MEB-5100型)測定記錄患者術前1 d、麻醉蘇醒后即刻、術后24 h、48 h機械痛敏程度;測定部位:手術切口旁3 cm與手術切口對側胸壁。采用視覺模擬評分法(VAS)評估患者術前1 d、麻醉蘇醒后即刻、術后24 h、48 h、2個月疼痛程度與慢性疼痛發生率。根據患者自行按壓的患者自控鎮痛(PCA)次數,計算術后芬太尼需要量。

2 結果
本研究由于部分病例收集資料不全,實際共納入150例患者,N組77例,K組73例,兩組患者性別、年齡、身高、體質量和ASA分級等一般資料差異均無統計學意義。結果顯示術前兩組健患側痛閾及VAS評分測定差異無統計學意義,N組蘇醒即刻健側及患側痛閾較術前明顯降低,術后24 h及48 h健側痛閾與術前差異無統計學意義,K組健側術后各時間點痛閾較術前差異無統計學意義,兩組患者蘇醒即刻及術后24 h患側痛閾雖然較術前都降低,但K組痛閾明顯比N組高,差異有統計學意義(Plt;0.05),術后48 h兩組患側痛閾差異無統計學意義(Pgt;0.05)(見表1);患者術前VAS 評分均為0分,術后即刻及術后24 h K組評分比N組低,差異有統計學意義(Plt;0.05)(見表2),術后PCIA的按壓次數及芬太尼使用量K組比N組明顯減少,差異有統計學意義(Plt;0.05)(見表2);術后兩組患者慢性疼痛發生率,差異有統計學意義(Plt;0.05)(見表3)。

表1 兩組電刺激痛閾測定結果
注:與組內術前同側比較,aPlt;0.05

表2 兩組術后VAS評分、PCIA按壓次數及芬太尼用量
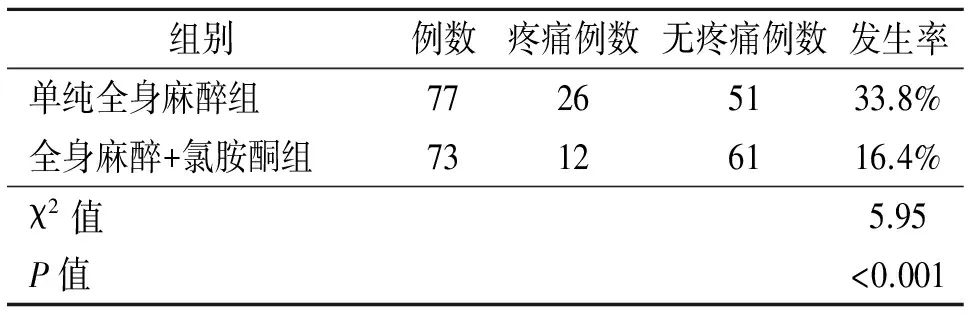
表3 兩組術后2個月慢性疼痛發生例數及發生率
3 討論
阿片類藥物已成為現代麻醉中必不可少的組成部分,但在臨床中,患者使用該類藥物一段時間后,有時會出現痛閾下降、疼痛范圍擴大甚至出現接觸痛的情況,這就是近年來被藥理和麻醉專家廣泛關注的阿片誘發痛覺過敏(OIH)現象,該現象可出現在術中應用阿片類藥物瑞芬太尼的圍手術期[4-6]。
OIH涉及的分子生物學機制復雜,尚無明確定論。現比較公認的機制包括中樞谷氨酸通路激活、脊髓下行易化、脊髓強啡肽濃度增加和遺傳因素等。氯胺酮作為谷氨酸受體通道亞型N-甲基-D-天門冬氨酸(NMDA)受體拮抗劑,具有超前鎮痛的作用[7-8],可減輕急性術后痛,減少術后鎮痛藥用量[9],本研究通過麻醉誘導給予氯胺酮與常規麻醉用藥相比較,結果顯示術前兩組健患側痛閾及VAS評分測定差異無統計學意義,N組蘇醒即刻健測及患測痛閾較術前明顯降低,術后24 h及48 h健側痛閾與術前差異無統計學意義,這與以往研究[10-11]基本相似,瑞芬太尼引起的痛覺過敏一般發生在術后12 h內,K組健側術后各時間點痛閾較術前差異無統計學意義,兩組患者蘇醒即刻及術后24 h患側痛閾雖然較術前都降低,但K組痛閾明顯比N組高,差異有統計學意義,這可能與氯胺酮可以阻斷中樞谷氨酸能誘發OIH通路的激活有關[12-14],術后48 h兩組患側痛閾差異無統計學意義。患者術前VAS 評分均為0分,術后即刻及術后24 h K組評分比N組低,差異有統計學意義,此結果與痛閾測定結果一致,同時同時也發現,術后48 h K組VAS評分比N組低,差異有統計學意義,但術后48 h痛閾測定兩者差異無統計學意義,存在主觀與客觀數據的矛盾,本研究可能由于病例數還不充足導致數據分析誤差,除此以外,影響患者對疼痛認知的能力受多種因素的影響,如遺傳因素、社會經歷、教育水平、精神狀態等。術后PCIA的按壓次數及芬太尼使用量K組比N組明顯減少,差異有統計學意義,與術后VAS評分結果一致,也能發現本研究術后疼痛管理及用藥的不足,尚需改進。術后慢性疼痛發生率,K組較N組明顯降低,這可能與氯胺酮提高了患者術后痛閾,以及作為NMDA受體拮抗劑能阻斷中樞谷氨酸通路激活有關,尚需更多數據進行論證。
綜上所述,麻醉誘導期給予氯胺酮能有效提高術中應用瑞芬太尼乳腺癌改良根治患者術后痛閾,從而降低了乳腺癌患者術后慢性疼痛的發生率。
[1] AMORE M,PSYD MI,VITTORIO CD,et al.Suicide attempts in major depressed patients with personality disorder[J].Suicide Life Threat Behav,2014,44(2):155-166.
[2] YANG G,WANG Y,ZENG Y,et al.Rapid health transition in China,1990-2010:findings from the Global Burden of Disease Study 2010[J].Lancet,2013,381(9882):1987-2015.
[3] SESSLE BJ.Unrelieved pain:A crisis[J].Pain Res Manag,2011,16(6):416-420.
[4] SONG YK,LEE C,SEO DH,et al.Interaction between postoperative shivering and hyperalgesia caused by high-dose remifentanil[J].Korean J Anesthesiol,2014,66(1):44-51.
[5] KANERIA A.Opioid-induced hyperalgesia:when pain killers make pain worse[J/OL].Bmj Case Rep,2014[2017-05-20].http://xueshu.baidu.com/s?wd=paperuri%3A%280bc4346d9051ba0629f683bbb2a73d30%29amp;filter=sc_long_signamp;tn=SE_xueshusource_2kduw22vamp;sc_vurl=http%3A%2F%2Fwww.ncbi.nlm.nih.gov%2Fpubmed%2F24899014amp;ie=utf-8amp;sc_us=12617887108611450792
[6] LEE HJ,YEOMANS DC.Opioid induced hyperalgesia in anesthetic settings[J].Korean J Anesthesiol,2014,67(5):299-304.
[7] KWOK RF,LIM J,CHAN MT,et al.Preoperative ketamine improves postoperative analgesia after gynecologic laparoscopic surgery[J].Anesth Analg,2004,98(4):1044-1049.
[8] LAUNO C,BASSI C,SPAGNOLO L,et al.Preemptive ketamine during general anesthesia for postoperative analgesia in patients undergoing laparoscopic cholecystectomy[J].Minerva Anestesiol,2004,70(10):727-734.
[9] MCCARTNEY CJ,SINHA A,KATZ J.A qualitative systematic review of the role of N-methyl-D-aspartate receptor antagonists in preventive analgesia[J].Anesth Analg,2004,98(5):1385-1400.
[10] HOOD DD,CURRY R,EISENACH JC.Intravenous remifentanil produces withdrawal hyperalgesia in volunteers with capsaicin-induced hyperalgesia[J].Anesth Analg,2003,97(3):810-815.
[11] ANGST MS.Intraoperative use of remifentanil for TIVA:postoperative pain,acute tolerance,and opioid-induced hyperalgesia[J].J Cardiothorac Vasc Anesth,2015,29(Suppl 1):16-22.
[12] ABREU M,AGUADO D,BENITO J,et al.Hyperalgesia and increased sevoflurane minimum alveolar concentration induced by opioids in the rat:a randomised experimental study[J].Eur J Anaesthesiol,2015,32(4):232-241.
[13] WU L,HUANG X,SUN L.The efficacy of N-methyl-D-aspartate receptor antagonists on improving the postoperative pain intensity and satisfaction after remifentanil-based anesthesia in adults:a meta-analysis[J].J Clin Anesth,2015,27(4):311-324.
[14] ZHANG C,LI SS,ZHAO N,et al.Phosphorylation of the GluN1 subunit in dorsal horn neurons by remifentanil:a mechanism for opioid-induced hyperalgesia[J].Genet Mol Res,2015,14(1):1846-1854.
EffectofpreoperaionuseofNMDAreceptorantagonistketamineontheincidenceofchronicpainafterbreastcancersurgery
ZhouXuyan,KongMin,JiangLishan,ShenXu,LuYaping,YaoMing,HuangBing
(DepartmentofAnesthesiology,JiaxingFirstHospital,Jiaxing314000,China)
KongMin,Email:sdjx10666@163.com
ObjectiveTo observe the effect of preoperaion use of NMDA receptor antagonist ketamine on the incidence of chronic pain after breast cancer surgery.Methods160 cases of patients with modified radical mastectomy for breast cancer under ASA Ⅰ or Ⅱ general anesthesia were randomly divided into group N (named as general anesthesia group) and group K (named as general anesthesia + ketamine group) by random number table.Record the mechanical hyperalgesia of postoperative 1 days before anesthesia,immediately after,24 hours and 48 hours after the operation;to evaluate the degree of chronic pain of patients before 1 days,immediately after anesthesia,after 24 hours and 48 hours by the VAS score,and the incidence of two groups patients by February statistics;to calculate the postoperative fentanyl requirement according to press the number of PCA.ResultsThe preoperative health ipsilateral pain threshold and VAS score was no significant difference between the two groups,the immediate ipsilateral and contralateral pain threshold in N group were significantly lower than their preoperative index,the contralateral preoperative pain threshold at postoperative 24 hours and 48 hours had no significant difference compared with operation before.The healthy side at each time point after operation in K group had no obvious differences compared with operation before,the ipsilateral pain threshold after the surgery while and 24 hours decreased compared with preoperative,but pain threshold was higher in the K group than that of N group,the difference was statistically significant (Plt;0.05),lateral pain threshold after 48 hours of operation in the two groups had no significant difference between (Pgt;0.05);the VAS score postoperative in patients was 0,it was lower at immediately after operation and 24 hours after operation in K group than in N group,the difference was statistically significant (Plt;0.05),postoperative PCIA Press Number and fentanyl use in K group was obviously lower than that of N group,the difference was statistically significant (Plt;0.05);the incidence of postoperative pain chronic in K group was statistically significant lower than that of the N group (Plt;0.05).ConclusionKetamine can improve the pain threshold in patients undergoing modified radical mastectomy and reduce the incidence of chronic pain in patients with breast cancer.
Breast neoplasms;Ketamine;Chronic pain;Pain threshold
浙江嘉興市科學技術局計劃(2014AY21024)
周煦燕,主任醫師,Email:zxy43529@163.com
孔敏,主治醫師,Email:sdjx10666@163.com
R737.9
A
10.3969/J.issn.1672-6790.2017.06.024
2017-08-10)

