唾液腺腺樣囊性癌頸淋巴結(jié)轉(zhuǎn)移規(guī)律的臨床研究*
黃擎韓楠男劉勝文王麗珍阮敏楊雯君張陳平
·臨床研究與應用·
唾液腺腺樣囊性癌頸淋巴結(jié)轉(zhuǎn)移規(guī)律的臨床研究*
黃擎①②韓楠男①劉勝文①王麗珍③阮敏①楊雯君①張陳平①
目的:本研究旨在回顧性分析頭頸部腺樣囊性癌的頸部淋巴結(jié)的臨床轉(zhuǎn)移規(guī)律。方法:回顧性分析1995年1月至2008年12月就診于上海交通大學醫(yī)學院附屬第九人民醫(yī)院口腔頜面-頭頸腫瘤科的616例腺樣囊性癌患者的臨床資料,對其中62例腺樣囊性癌合并頸部淋巴結(jié)轉(zhuǎn)移的患者進行臨床統(tǒng)計學分析。結(jié)果:頭頸部腺樣囊性癌的頸淋巴結(jié)轉(zhuǎn)移的發(fā)生率約為10%,原發(fā)于舌根、舌體及口底部的腺樣囊性癌較其他部位更易發(fā)生頸部淋巴結(jié)轉(zhuǎn)移,分別為19.2%、17.6%和15.3%,轉(zhuǎn)移部位多發(fā)生在Ⅰb區(qū)與Ⅱ區(qū)。淋巴結(jié)轉(zhuǎn)移的方式以經(jīng)典的管道性轉(zhuǎn)移為主,直接浸潤型轉(zhuǎn)移僅常見于下頜下腺的腺樣囊性癌累及頜下淋巴結(jié)。原發(fā)部位及瘤周淋巴血管浸潤與頸部淋巴結(jié)轉(zhuǎn)移的發(fā)生密切相關(guān)。出現(xiàn)頸部淋巴結(jié)轉(zhuǎn)移的患者其臨床預后明顯較差(P<0.01)。結(jié)論:舌-口底復合體為頭頸部腺樣囊性癌發(fā)生淋巴結(jié)轉(zhuǎn)移的常見原發(fā)部位,在臨床治療及隨訪上應得到更多關(guān)注。
唾液腺腺樣囊性癌淋巴結(jié)轉(zhuǎn)移預后
唾液腺腺樣囊性癌(adenoid cystic carcinoma,ACC)是來源于唾液腺上皮的惡性腫瘤[1-2],具有臨床進展緩慢、嗜神經(jīng)侵襲、極易復發(fā)和遠處轉(zhuǎn)移等生物學特性。依據(jù)上海交通大學醫(yī)學院附屬第九人民醫(yī)院口腔病理科數(shù)據(jù),腺樣囊性癌在唾液腺上皮性惡性腫瘤中居首位[3]。腺樣囊性癌的遠處轉(zhuǎn)移主要發(fā)生在肺部,研究表明腺樣囊性癌遠處轉(zhuǎn)移的概率約為35%~50%,是腺樣囊性癌患者死亡的主要原因[4-7],而發(fā)生淋巴結(jié)轉(zhuǎn)移的病例較為少見。為獲取腺樣囊性癌頸部淋巴結(jié)轉(zhuǎn)移的臨床規(guī)律,本研究通過大樣本回顧性研究,分析ACC頸部淋巴結(jié)轉(zhuǎn)移的發(fā)生率、轉(zhuǎn)移淋巴結(jié)的區(qū)域分布,探討轉(zhuǎn)移淋巴結(jié)與原發(fā)部位、臨床分期、病理類型及轉(zhuǎn)移模式的相關(guān)性,為ACC頸部淋巴結(jié)轉(zhuǎn)移的早期發(fā)現(xiàn)和臨床干預提供理論依據(jù)。
1 材料與方法
1.1 病例資料
回顧性分析1995年1月至2008年12月上海交通大學醫(yī)學院附屬第九人民醫(yī)院口腔頜面-頭頸腫瘤科收治的616例腺樣囊性癌患者的病例資料。符合納入標準的患者共616例。其中男性302例,女性314例,中位年齡為51.6(11~89)歲。病例納入標準為:1)ACC患者;2)有明確的手術(shù)治療史;3)有完整的臨床病理及隨訪資料;4)告知患者并征得患者同意。本研究已獲得被研究對象或其家屬知情同意并得到醫(yī)院倫理委員會批準。
1.2 方法
病例資料的基本信息包括患者的發(fā)病年齡、性別、病程、發(fā)病部位、臨床癥狀和臨床分期。由兩名經(jīng)驗豐富的病理學專家通過病理組織切片獲取腫瘤的生長模式、組織學分級、手術(shù)切緣、淋巴結(jié)轉(zhuǎn)移、血管及神經(jīng)侵犯等臨床病理學指標。通過術(shù)后長期隨訪并定期影像學檢查獲取ACC患者預后各項指標并監(jiān)測頸部淋巴結(jié)狀態(tài)。
1.3 統(tǒng)計學分析
采用SPSS 19.0軟件進行統(tǒng)計學分析。通過配對樣本t檢驗和χ2檢驗分析測定臨床病理特征和淋巴結(jié)轉(zhuǎn)移之間的顯著差異,應用Kaplan-Meier法計算術(shù)后生存率,使用邏輯回歸分析來確定淋巴結(jié)轉(zhuǎn)移與預后的相關(guān)性。以P<0.05為差異具有統(tǒng)計學意義。
2 結(jié)果
2.1 淋巴結(jié)轉(zhuǎn)移的發(fā)生率
符合納入標準的共616例腺樣囊性癌患者,其中男性302例,女性314例,男女比例約為1:1,中位年齡為51.6(11~89)歲,發(fā)生于大、小唾液腺的病例分別為194例(31.5%)和422例(68.5%),小唾液腺中以腭部最常見(軟腭及硬腭),占39.3%(166/422),大唾液腺中以下頜下腺最常見,占41.2%(80/194)。見表1。
616例腺樣囊性癌患者中,62例發(fā)生頸部淋巴結(jié)轉(zhuǎn)移,發(fā)生率約為10%。38例患者術(shù)中發(fā)現(xiàn)淋巴結(jié)轉(zhuǎn)移,24例患者在原發(fā)腫瘤切除術(shù)后出現(xiàn)淋巴結(jié)轉(zhuǎn)移。舌根、舌體和口底區(qū)域是腺樣囊性癌發(fā)生頸部淋巴結(jié)轉(zhuǎn)移最為常見的3個原發(fā)部位,發(fā)生率分別為19.2%、17.6%和15.3%(圖1)。
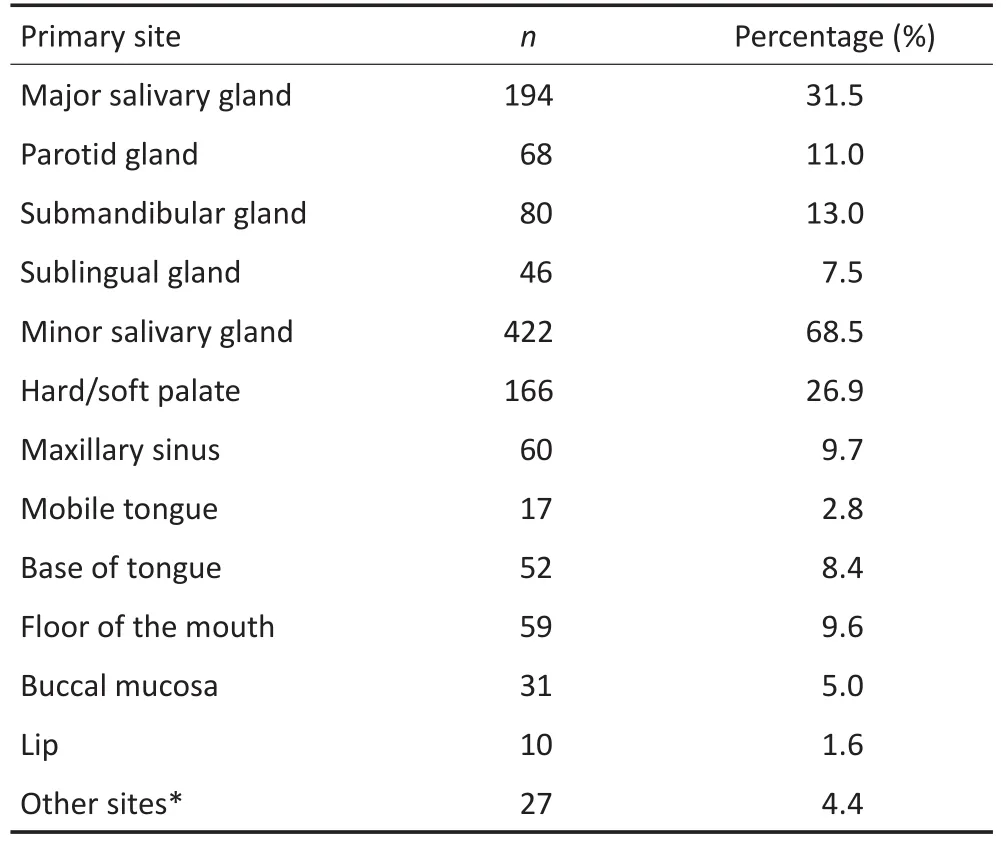
表1 ACC原發(fā)部位分布(n=616)Table 1Distribution of the primary sites(n=616)

圖1 ACC患者腫瘤原發(fā)部位與頸淋巴結(jié)轉(zhuǎn)移發(fā)生率關(guān)系Figure 1Incidence of lymph node metastasis in ACC patients according to the primary site locations
2.2 淋巴結(jié)轉(zhuǎn)移與臨床病理指標的相關(guān)性
ACC頸部淋巴結(jié)轉(zhuǎn)移與腫瘤原發(fā)部位、腫瘤周圍淋巴/血管浸潤密切相關(guān)。其他指標包括年齡、性別、腫瘤大小及生長模式,與頸部淋巴結(jié)轉(zhuǎn)移均無顯著相關(guān)性。在神經(jīng)侵犯這一指標上,有神經(jīng)侵犯患者的頸部淋巴結(jié)轉(zhuǎn)移率較無神經(jīng)侵犯者高,但差異無統(tǒng)計學意義(P=0.06),有待進一步的大樣本研究確認(表2)。
2.3 轉(zhuǎn)移淋巴結(jié)的區(qū)域分布及轉(zhuǎn)移模式
出現(xiàn)淋巴結(jié)轉(zhuǎn)移局限于一個區(qū)域的病例占74%(46/62),同時發(fā)生2個或2個以上區(qū)域淋巴結(jié)轉(zhuǎn)移的病例占26%(16/62)。其中,Ⅰb區(qū)和Ⅱ區(qū)是最常見的轉(zhuǎn)移區(qū)域,分別為27例(44%)和37例(60%)。僅14例(23%)發(fā)生Ⅲ區(qū)和Ⅳ區(qū)頸部淋巴結(jié)轉(zhuǎn)移(圖2)。根據(jù)臨床病史、影像學檢查和組織病理學檢測,本研究綜合分析ACC頸部轉(zhuǎn)移淋巴結(jié)的轉(zhuǎn)移模式,結(jié)果表明,大多數(shù)情況下原發(fā)腫瘤發(fā)生淋巴結(jié)轉(zhuǎn)移的方式以沿淋巴管轉(zhuǎn)移或血管通路經(jīng)典的管道性轉(zhuǎn)移為主(圖3,4)。原發(fā)于下頜下腺的腺樣囊性癌,其頸部淋巴結(jié)轉(zhuǎn)移大都由腫瘤直接侵犯下頜下淋巴結(jié)(圖5)。

表2 臨床病理指標與頸淋巴結(jié)轉(zhuǎn)移率的關(guān)系Table 2Clinicopathological variables affecting lymph node metastasis
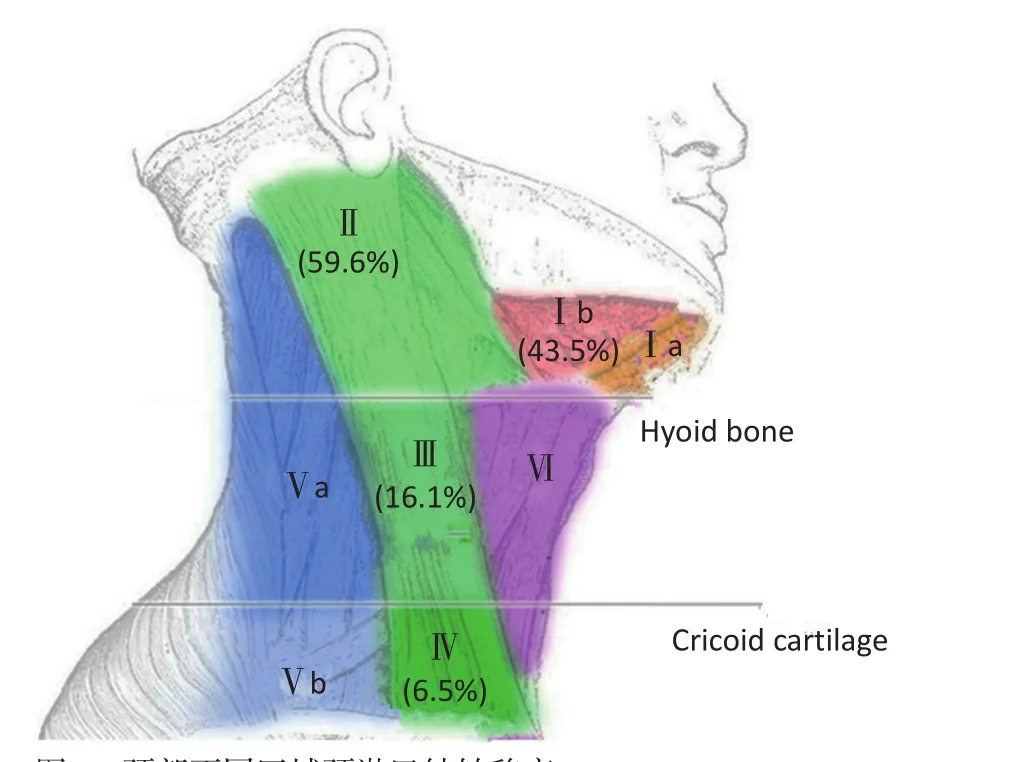
圖2 頸部不同區(qū)域頸淋巴結(jié)轉(zhuǎn)移率Figure 2Distribution of cervical lymph node metastasis in ACC patients
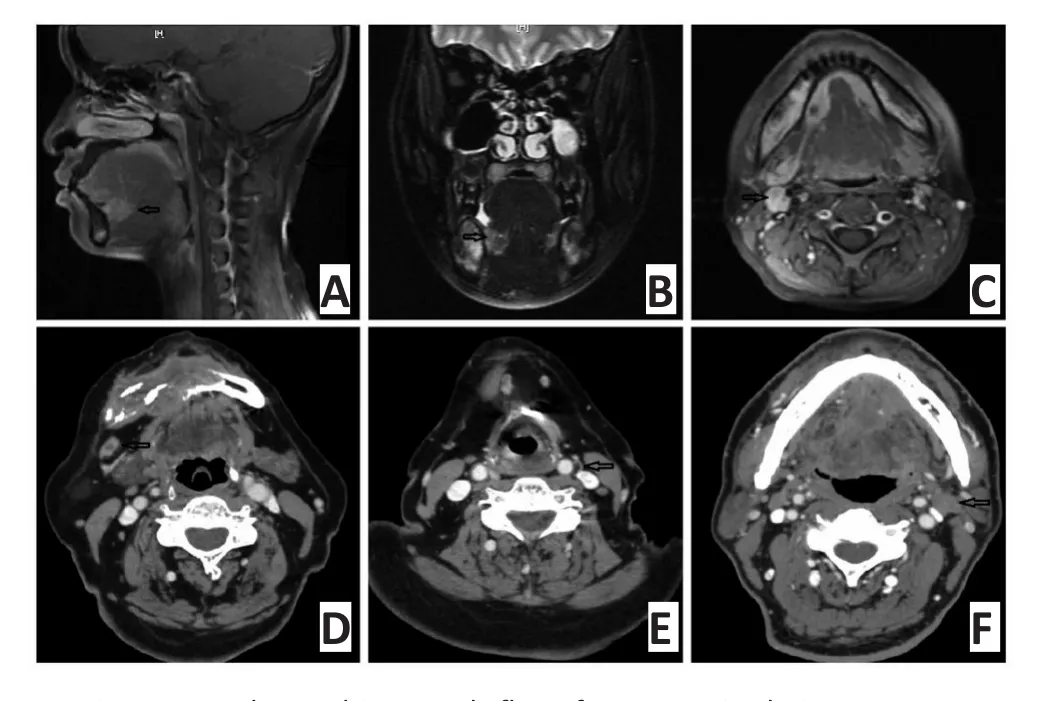
A.Primary ACC located in mouth floor from a sagittal view;B-F.Metastatic lymph nodes at levelⅡregion show an anastomosis圖3原發(fā)于口底的ACC頸部Ⅱ區(qū)轉(zhuǎn)移示意圖(如圖中箭頭所示)Figure 3A diagram showing a levelⅡlymph node metastasis of primary site ACC in the mouth floor(arrow shown)

A.Perversion of tumor cell(cribriform pattern)in the metastatic lymph node,with few lymphocytes inside the integrated envelope(H&E×10); B.Tumor cells(cribriform pattern)invading the envelope starting from the inside to the outside area(H&E×100);C.Metastatic lymph node filled with tumor cells with no remaining lymphocytes(H&E×200);D. Multiple metastases distributed sporadically in the metastatic lymph node with integrated envelope(H&E×4);E.Isolated metastasis(solid pattern)emerging just beside the node envelope(H&E×200);F.Metastatic ACC cells(solid pattern)beside the node envelope(H&E×400)圖4經(jīng)典管道轉(zhuǎn)移途徑受累淋巴結(jié)的病理特征Figure 4Pathological features of metastatic lymph nodes invading mostly through a"lymphatic vessel and/or blood vessel"pathway
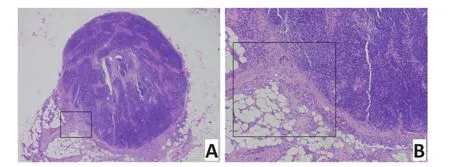
A.Tumor cells from the submandibular gland invading directly the lymph node in the submandibular region(H&E×4);B.Tumor cells invading the lymph node starting from the extra-to the intracapsular area (H&E×400)圖5原發(fā)于下頜下腺的ACC瘤細胞直接浸潤轉(zhuǎn)移累及頜下淋巴結(jié)示意圖Figure 5Metastatic lymph node in the submandibular region caused by the direct invasion of tumor cells from the submandibular gland
2.4 淋巴結(jié)轉(zhuǎn)移與預后
手術(shù)治療是目前最主要的治療方式,術(shù)前臨床診斷為cN(+)的患者在徹底切除原發(fā)性腫瘤的同時需行頸部淋巴結(jié)清掃術(shù),同時術(shù)后應補充放療。術(shù)后平均隨訪時間為56.2(6~128)個月,隨訪結(jié)果表明62例出現(xiàn)頸部淋巴結(jié)轉(zhuǎn)移的腺樣囊性癌患者其5年生存率為48%,遠遠低于本研究隨機選擇設(shè)立的對照組的生存率(77%)(圖6)。
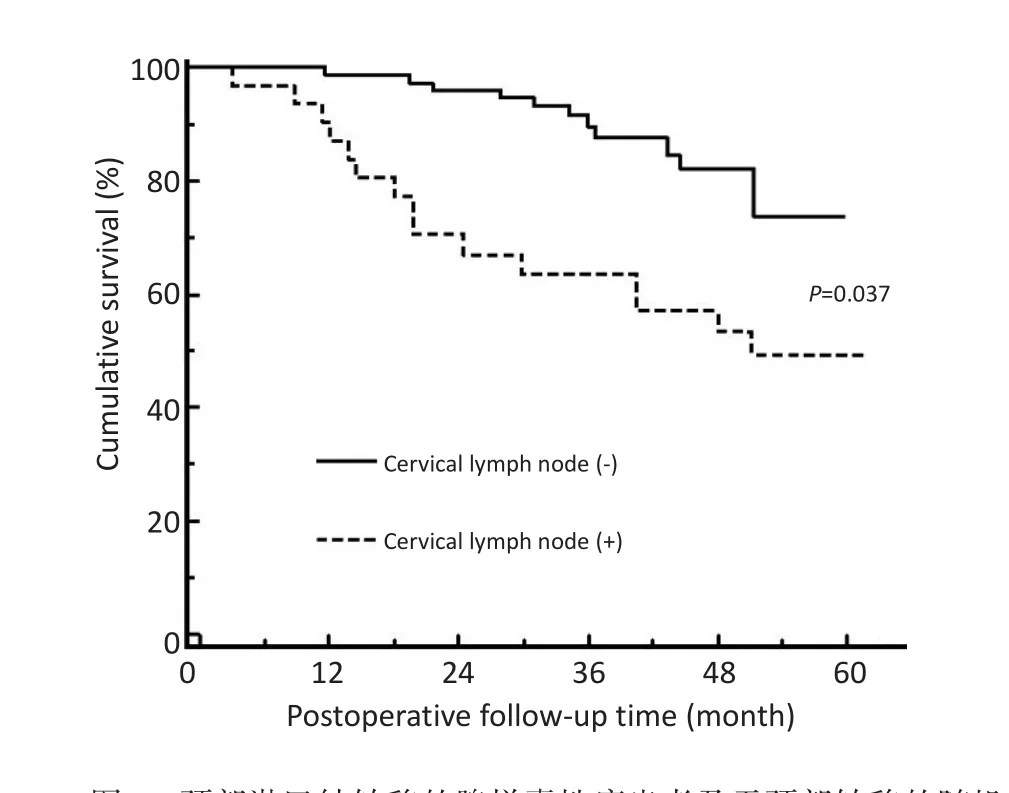
圖6 頸部淋巴結(jié)轉(zhuǎn)移的腺樣囊性癌患者及無頸部轉(zhuǎn)移的隨機對照組術(shù)后生存率對比Figure 6Kaplan-Meier analysis of the overall survival of ACC patients according to the extent of lymph node metastasis
3 討論
肺部是腺樣囊性癌最為常見的遠處轉(zhuǎn)移部位[8],原發(fā)性腺樣囊性癌出現(xiàn)頸部淋巴結(jié)轉(zhuǎn)移的病例較為少見[9]。既往研究中,報道了600余例ACC病例[3],本研究進一步聚焦伴有頸部淋巴結(jié)轉(zhuǎn)移的62例患者,對其轉(zhuǎn)移規(guī)律進行臨床研究分析,數(shù)據(jù)表明其發(fā)生約為10%。由于ACC多見于腮腺和腭部,而這些區(qū)域出現(xiàn)頸部淋巴結(jié)轉(zhuǎn)移的概率相對較低,因此可能是ACC伴有頸部淋巴結(jié)轉(zhuǎn)移病例總體上較少的原因之一。本研究中舌根、舌體和口底區(qū)域是腺樣囊性癌發(fā)生淋巴結(jié)轉(zhuǎn)移最常見的3個原發(fā)部位,發(fā)生率分別為19.2%、17.6%和15.3%,提示在臨床治療和隨訪過程中,對原發(fā)于上述3個部位的腺樣囊性癌患者應密切監(jiān)測頸部淋巴結(jié)變化。本研究對于舌根部腺樣囊性癌發(fā)生淋巴結(jié)轉(zhuǎn)移概率最高的臨床現(xiàn)象分析可能的原因包括以下3個方面:1)位于舌根的ACC,通常在黏膜下生長,患者無明顯癥狀,難以早期發(fā)現(xiàn)并治療;2)在解剖結(jié)構(gòu)上,舌根部存在豐富的血管和淋巴管系統(tǒng),有利于癌細胞的運動轉(zhuǎn)移;3)舌根的頻繁運動增加轉(zhuǎn)移的可能性。
既往基于小樣本的國外研究發(fā)現(xiàn)腺樣囊性癌頸部淋巴結(jié)轉(zhuǎn)移最常見的原發(fā)部位是下頜下腺[10],轉(zhuǎn)移的淋巴結(jié)都是下頜下淋巴結(jié),其周圍軟組織有腫瘤細胞浸潤,而淋巴結(jié)內(nèi)未見瘤栓[11]。因此,上述研究認為所謂的腺樣囊性癌淋巴結(jié)轉(zhuǎn)移均為腫瘤直接侵犯淋巴結(jié)所致。在本研究中,大多數(shù)轉(zhuǎn)移淋巴結(jié)的位置都遠離原發(fā)病灶,如原發(fā)于腭部/舌部的腺樣囊性癌同時伴有Ⅱ區(qū)的淋巴結(jié)轉(zhuǎn)移,顯然直接侵犯這一途徑無法合理解釋。在這些病例中,腫瘤可能通過脈管系統(tǒng)(淋巴系統(tǒng)和/或血管系統(tǒng))遷移并定植于頸部淋巴結(jié),在其內(nèi)部增殖并最終突破淋巴結(jié)包膜浸潤至結(jié)外軟組織。基于此,本研究提出唾液腺ACC的頸部淋巴結(jié)轉(zhuǎn)移主要模式是通過血管和(或)淋巴管轉(zhuǎn)移;次要的轉(zhuǎn)移模式為原發(fā)性腫瘤直接侵襲導致頸部淋巴結(jié)轉(zhuǎn)移,且多出現(xiàn)于下頜下腺這一特殊的部位。
對于ACC的預后評估,既往的研究將發(fā)病部位、病理類型、臨床分期、神經(jīng)侵犯、術(shù)后復發(fā)、遠處轉(zhuǎn)移及治療方法作為候選影響因素并進行相關(guān)性分析[12-13]。受限于樣本量,鮮有研究關(guān)注淋巴結(jié)轉(zhuǎn)移與腺樣囊性癌患者預后之間的關(guān)系。本研究結(jié)果表明淋巴結(jié)轉(zhuǎn)移與腺樣囊性癌患者的生存率呈負相關(guān)。因此,本研究認為早期cN0患者在多數(shù)情況下不建議行頸部淋巴結(jié)清掃術(shù),但對于腫瘤發(fā)生在舌根、舌體和口底區(qū)域較大的cN0患者應考慮到存在淋巴管浸潤及后期淋巴結(jié)轉(zhuǎn)移的風險,在治療和隨訪過程中應密切監(jiān)測頸部淋巴結(jié)情況;對于原發(fā)或復發(fā)的cN(+)患者,本研究推薦的治療方案為針對原發(fā)或復發(fā)腫瘤的徹底切除,聯(lián)合區(qū)域性或根治性頸部淋巴結(jié)清掃,術(shù)后配合放射治療,有助于局部復發(fā)和遠處轉(zhuǎn)移的控制[14]。
綜上所述,本研究發(fā)現(xiàn)舌-口底復合體及下頜下腺區(qū)域的腺樣囊性癌患者發(fā)生頸部淋巴結(jié)轉(zhuǎn)移的風險最高,臨床應密切監(jiān)測。頸部淋巴結(jié)轉(zhuǎn)移的主要方式為管道性轉(zhuǎn)移,即通過淋巴管或者血管轉(zhuǎn)移,而并非區(qū)域性侵犯。頸部淋巴結(jié)轉(zhuǎn)移是腺樣囊性癌患者不良預后的重要指標之一。因此,本研究將致力于探討腺樣囊性癌淋巴結(jié)轉(zhuǎn)移過程中的關(guān)鍵分子標記物和潛在的治療靶點[15],為提高腺樣囊性癌患者尤其是伴有淋巴結(jié)轉(zhuǎn)移的患者生存率提供新的思路。
[1]da Cruz Perez DE,de Abreu Alves F,Nobuko Nishimoto I,et al.Prognostic factors in head and neck adenoid cystic carcinoma[J].Oral Oncol,2006,42(2):139-146.
[2]Oplatek A,Ozer E,Agrawal A,et al.Patterns of recurrence and survival of head and neck adenoid cystic carcinoma after definitive resection[J].Laryngoscope,2010,120(1):65-70.
[3]Tian Z,Li L,Wang L,et al.Salivary gland neoplasms in oral and maxillofacial regions:a 23-year retrospective study of 6 982 cases in aneastern Chinese population[J].Int J Oral Maxillofac Surg,2010,39 (3):235-242.
[4]van der Wal JE,Becking AG,Snow GB,et al.Distant metastases of adenoid cystic carcinoma of the salivary glands and the value of diagnostic examinations during follow-up[J].Head Neck,2002,24(8): 779-783.
[5]Fordice J,Kershaw C,el-Naggar A,et al.Adenoid cystic carcinoma of the head and neck,Predictors of morbidity and mortality[J]. Arch Otolaryngol Head Neck Surg,1999,125(2):149-152.
[6]Spiro RH.Distant metastasis in adenoid cystic carcinoma of salivary origin[J].Am J Surg,1997,174(5):495-498.
[7]Bradley PJ.Adenoid cystic carcinoma of the head and neck:a review[J].Curr Opin Otolaryngol Head Neck Surg,2004,12(2):127-132.
[8]Papaspyrou G,Hoch S,Rinaldo A,et al.Chemotherapy and targeted therapy in adenoid cystic carcinoma of the head and neck:a review[J].Head Neck,2011,33(6):905-911.
[9]Kokemueller H,Eckardt A,Brachvogel P,et al.Adenoid cystic carcinoma of the head and neck-a 20 years experience[J].Int J Oral Maxillofac Surg,2004,33(1):25-31.
[10]Allen Jr MS,Marsh Jr WL.Lymph node involvement by direct extension in adenoid cystic carcinoma:Absence of classic embolic lymph node metastasis[J].Cancer,1976,38(5):2017-2021.
[11]Zhang M,Xu ZF,Tao Y,et al.Clinical analysis of 25 patients with glossaladenoid cystic carcinoma[J].Int J Stomt,2009,36(2):148-151.[張梅,徐忠法,陶陽,等.25例舌部腺樣囊性癌的臨床分析[J].國際口腔醫(yī)學雜志,2009,36(2):148-151.]
[12]Reziya A,DilinuerA,Sun ZZ,et al.Factors related to local recurrence and distant metastasis of the salivary gland adenoid cystic carcinoma[J].J Prac Stom,2011,27(5):649-652.[熱孜亞·艾尼,迪麗努爾·阿西木,孫振柱,等.涎腺腺樣囊性癌的局部復發(fā)及遠處轉(zhuǎn)移因素分析[J].實用口腔醫(yī)學雜志,2011,27(5):649-652.]
[13]Zheng G,Guo CB,Yu GY,et al.Development of a predicting model of survival rates for patients with salivary adenoid cystic carcinoma [J].Chin J Stom,2006,41(6):350-353.[鄭剛,郭傳瑸,俞光巖,等.腺樣囊性癌患者生存預測模型的建立[J].中華口腔醫(yī)學雜志, 2006,41(6):350-353.]
[14]Silverman DA,Carlson TP,Deepak K,et al.Role for postoperative radiation therapy in adenoid cystic carcinoma of the head and neck [J].Laryngoscope,2004,114(7):1194-1199.
[15]Vila L,Liu H,Al-Quran SZ,et al.Identification of c-kit gene mutations in primary adenoid cystic carcinoma of the salivary gland[J]. Mod Pathol,2009,22(10):1296-1302.
(2016-09-26收稿)
(2016-11-08修回)
(編輯:孫喜佳 校對:張抿)
A clinical study of the characteristics of the cervical lymph node metastasis in patients with salivary gland adenoid cystic carcinoma
Qing HUANG1,2,Nannan HAN1,Shengwen LIU1,Lizhen WANG3,Min RUAN1,Wenjun YANG1,Chenping ZHANG1
Min RUAN;E-mail:doctorruanmin@hotmail.com
1Department of Oral&Maxillofacial Surgery,Ninth People's Hospital,Shanghai Jiao Tong University School of Medicine,Shanghai Key Laboratory of Stomatology,Shanghai 200011,China;2The Second People's Hospital of Hefei,Hefei,230011,China;3Department of Oral Pathology,Ninth People's Hospital,Shanghai Jiao Tong University School of Medicine,Shanghai Key Laboratory of Stomatology,Shanghai 200011,China
This work was supported by the National Natural Science Foundation of China(No.81102049,81472517),Shanghai Pujiang Program (No.15PJD024),SMC of Shanghai Jiao Tong University and Shanghai Summit&Plateau Disciplines
Objective:Adenoid cystic carcinoma(ACC)is an uncommon malignant neoplasm,which mostly originates from the major and minor salivary glands of the head and neck region.This study aims to provide new information on head and neck ACC with cervical lymph node metastasis.Methods:Out of the 616 patients who underwent primary tumor resection from 1995 to 2008 in the authors' hospital,62 cases with cervical lymph node metastasis were analyzed.Results:The general incidence rate of cervical lymph node metastasis in ACC was approximately 10%.The base of the tongue,mobile tongue,and mouth floor were the most frequent sites of lymph node metastasis with incidence rates of 19.2%,17.6%,and 15.3%,respectively.Most cases exhibited the classic"tunnel-style" metastatic pattern of occurrence,and the levelⅠb andⅡregions were the most frequently involved areas.Primary site and lymphovascular invasions were significantly associated with lymph node metastasis.High patient mortality rate was also significantly correlated with a high number of lymph node positive cases.Conclusion:Cervical lymph node metastasis has a high tendency of occurrence in the tongue-mouth floor complex,following the classic"tunnel-style"metastatic pattern.Peritumoral lymphovascular invasion could be taken as a strong predictor for the occurrence of lymph node metastasis,which ultimately leads to poor prognosis of ACC patients.A selective neck dissection should be considered as a management in such patients.
salivary gland,adenoid cystic carcinoma,cervical lymph node metastasis,prognosis
10.3969/j.issn.1000-8179.2016.24.125

①上海交通大學醫(yī)學院附屬第九人民醫(yī)院口腔頜面-頭頸腫瘤科,上海市口腔醫(yī)學重點實驗室(上海市200011);②安徽省合肥市第二人民醫(yī)院口腔頜面外科;③上海交通大學醫(yī)學院附屬第九人民醫(yī)院口腔病理科,上海市口腔醫(yī)學重點實驗室
*本文課題受國家自然科學基金項目(編號:81102049,81472517),上海市浦江人才計劃項目(編號:15PJD024),上海交通大學晨星學者計劃和上海高校高峰高原學科(口腔醫(yī)學)建設(shè)項目資助
阮敏doctorruanmin@hotmail.com
黃擎專業(yè)方向為口腔頜面及頭頸部腫瘤的臨床診治。
E-mail:6743919@qq.com