Cross-sectional survey of the relationship of symptomatology,disability and family burden among patients with schizophrenia in Sichuan, China
Zhuoqiu ZHANG, Hong DENG, Ying CHEN, Shuiying LI, Qian ZHOU, Hua LAI, Lifang LIU, Ling LIU,Wenwu SHEN*
?Original Article?
Cross-sectional survey of the relationship of symptomatology,disability and family burden among patients with schizophrenia in Sichuan, China
Zhuoqiu ZHANG, Hong DENG, Ying CHEN, Shuiying LI, Qian ZHOU, Hua LAI, Lifang LIU, Ling LIU,Wenwu SHEN*
schizophrenia, family relationships, burden of illness, disability evaluation, cross-sectional survey, China
1. Introduction
The treatment of schizophrenia has improved in the last few decades, but work still needs to be done. Symptoms can usually be controlled with treatment but the residual impairment in functioning makes it difficult for patients to return to society.[1]Schizophrenia is a chronic condition associated with a high level of disability which is a leading contributor to overall disability in the population.[2,3]According to estimates from the Global Burden of Diseases study, schizophrenia is the 8thleading cause of disability-adjusted life years worldwide in the 15 to 44 age group.[4]But these measures only consider the effect of schizophrenia on the quality of life of the individual,[2,3,5]not on the quality of life of family members who, in most societies, are the primary care-givers for persons with schizophrenia. The current study seeks to assess the associations of patients’clinical characteristics and level of disability with family functioning and family burden in patients with schizophrenia.
2. Methods
2.1 Participants
As shown in Figure 1, patients with schizophrenia were recruited from the Mental Health Center of a large (tertiary level) psychiatric hospital in Sichuan Province, China from February to March, 2013. A total of 896 patients who met the following inclusion criteria were referred to the research team by their treating psychiatrists: (a) met the diagnostic criteria of schizophrenia using the 10thedition of the International Classification of Diseases (ICD-10);[6](b) 16 years of age or older; (c) receiving regular follow-up outpatient treatment after discharge from a psychiatric hospital; (d)clinically stable for at least three months with no change in medication regimen; (e) no organic brain disorder or mental retardation; (f) both the patient and their caregivers signed informed consent forms indicating their willingness to participate. The study was approved by the Ethics Committee at Sichuan University.

Figure 1. Identification of participants
2.2 Assessments
The survey had five components: a basic demographic and illness history questionnaire; the Chinese version of the World Health Organization Disability Assessment Schedule II (WHODAS II)[7]; the Positive and Negative Syndrome Scale (PANSS)[8]; the Family Adaptation,Partnership, Growth, Affection, Resolve Index (APGAR)[8];and the Family Burden Interview Schedule (FBIS).[8]Six psychiatrists and psychiatric nurses with more than eight years of clinical experience were trained to administer the survey using a standardized protocol. After the training, WHODAS II and PANSS were administered to 12 patient volunteers twice (by two independent interviewers) and the WHODAS II was retested with these individuals after an interval of two weeks. The inter-rater reliability of evaluators for WHODAS II and PANSS were good (Kappa=0.81 and 0.93, respectively),and the test-retest reliability of WHODAS II was fair(Kappa=0.78).
The demographic and illness history form collected information about sex, age, level of education,marital status, living status (i.e., alone or with family),occupational status, types of medical insurance, history of severe physical illness and family history of mental illness. It also collected information about the psychiatric history including the age of onset of schizophrenia, the number of relapses, the number of hospitalizations,the overall duration of illness, and the co-occurrence of substance abuse disorders or other mental disorders.
Face-to-face interviews were conducted to assess current levels of disability using the WHODAS II.[7]This scale measures disability in six domains: cognition(6 items), mobility (5 items), self-care (4 items),interpersonal relationships (5 items), role functioning(8 items) and social participation (8 items). Each item is rated on a 5-point Likert scale from 1 (no difficulty)to 5 (extreme difficulty) yielding a total score ranging from 36 to 180, with a higher scores indicating greater disability. The total score is used to categorize individuals into five groups: ‘extreme disability’ (total score >116),‘severe disability’ (total score=106-115), ‘moderate disability’ (total score=96-105), ‘mild disability’ (total score=52-95), and ‘no disability’ (total score=36-51).Wang and colleagues[9]administered the Chinese version of the WHODAS II to psychiatric patients and reported that the scale has good internal consistency (Cronbach a=0.93). In the current study the WHODAS II results were dichotomized, those with total scores of less than or equal to 51 were classif i ed as ‘not disabled’ and those with total scores greater than 51 were classified as‘disabled’.
The PANSS[8]is the most commonly used scale for assessing the severity of the symptoms of schizophrenia in China. It evaluates the clinical status of patients over the prior month. The scale is subdivided into a positive symptoms subscale, a negative symptoms subscale and a global psychopathology subscale. Evaluators rate 30 items on a 1- to 7-point Likert scale (higher scores represent more severe symptoms) using information provided both by the patient and co-resident family members. Previous reports[8]indicate that the test-retest reliability of the three subscales of the Chinese version of the PANSS are fair to good (kappa=0.77-0.89).
Family APGAR[8]is a 5-item, self-rated scale developed by Smilkstein[10]that measures the degree of patients’ satisfaction with family support that focuses on the emotional, communicative and social interactive relationship between patients and their family members. Respondents rate each item from 0 to 2, yielding a total score ranging from 0 to 10, with lower scores representing poorer perceived family support.The Chinese Family APGAR has been validated,[11]using a non-mentally ill sample. In the current study the internal consistency of the 10 items was acceptable(Cronbach’s a=0.76).
The FBIS[8]is a semi-structured interview schedule that assesses the burden experienced by the family members of psychiatric patients. Face-to-face interviews using FBIS were conducted with the caregivers of the patients who brought them to the outpatient department.The FBIS has 26 items, 25 of which objectively assess family burden in six domains: financial burden, effect on the family members daily routines, effect on family members’ leisure activities, effect on interpersonal relationships within the family, self-reported effects on physical health of other family members, and selfreported effects on the mental health of other family members. The final item asks respondents about their perceived subjective burden related to having a mentally ill family member. Each item is rated on a 3-point Likert scale: 0 (no burden), 1 (medium burden)and 2 (high burden). The Chinese version of FBIS has been validated among caregivers of 21 psychiatric patients[12]: the internal validity was good (Chronbach a = 0.83), the inter-rater reliability was fair to excellent(Kappa=0.61-1.00), and the objective burden reported by the interviewer was significantly correlated with the subjective burden reported by the family members(r=0.68, p<0.001).
2.3 Statistical analysis
Data were entered in Microsoft EXCEL and analyzed using SPSS version 13.0 (SPSS Inc., Chicago IL). Crossgroup differences in the WHODAS II scores were compared using t-tests or F-tests. The characteristics of patients who were and were not classified as disabled were compared using Mann-Whitney rank tests when the variable assessed was not normally distributed and t-tests when the variable assessed was normally distributed. Spearman rank correlation coefficients were calculated to estimate the correlation between WHODAS II scores and other clinical or family variables. It is certainly possible that a non-linear relationship exists between the severity of disability and the potential predictor variables, so both stepwise binary logistic regression (with presence or absence of disability as the dependent variable) and stepwise generalized linear regression (with WHODAS II overall score as the dependent variable) were employed to identify variables that are independently associated with disability. The statistical signif i cance level was set at p<0.05.
3. Results
3.1 Characteristics ofthe sample
Only 101 of the 896 eligible patients (11.3%) agreed to participate in the survey. Among these 101 individuals,59 (58.4%) were male and 42 (41.6%) were female;their mean (sd) age was 28.8 (10.6) years; 32 had attended college, 44 were high school or technical school graduates, and 25 had a middle school education or less; 14 were currently working, 14 were current students and the remaining 73 were unemployed; 81 were single, 14 were currently married and 6 were divorced or widowed; 49 had government-sponsored Urban Residents Medical Insurance, 10 had governmentsponsored New Rural Cooperative Medical Care System(NCMS) insurance, 3 had commercial insurance, and 39 did not have any type of medical insurance; 92 were living with immediate family members, 5 were living with schoolmates, 2 were living with other relatives and 2 were living alone. The onset age of schizophrenia varied from 12 to 42 years of age (mean[sd]= 24.8 [6.1]years); the duration of illness ranged from 5 months to 31 years (median [IQR] of 5 [1.0-11.5] years); 23 had a concurrent severe physical illness (including high blood pressure, diabetes, hepatitis and epilepsy); 26 had a family history of mental disorders; the modal number of relapses was 1 (range=0-10); and the modal number of hospitalizations was 2 (range=1-7).
3.2 WHODAS II scores in patients with different demographic characteristics
The mean (sd) WHODAS score of the sample was 61.6(16.5) (skewness=0.97, p>0.05; kurtosis=1.592, p>0.05).No statistically significant differences in the WHODAS II scores were found across demographic subgroups,including sex (t=-0.80, p=0.424), family history of mental illnesses (t=0.20, p=0.842), presence of severe physical illness (t=-0.82, p=0.413), level of education (F=0.05,p=0.995), marital status (F=2.81, p=0.065), occupational status (F=0.81, p=0.562), and type of health insurance(F=0.20, p=0.900).
3.3 Clinical and family characteristics of patients with and without disability
Based on the WHODAS II total score, 74 of the 101 patients (73.3%) were disabled; among them 71 had mild disability (WHODAS II score 52-95), 2 had moderate disability (score 106-115) and one had extreme disability(score >116). The comparison of the characteristics of patients with and without disability is shown in Table 1. Compared to patients without disability, patients with disability had a younger age of onset and higher
negative symptom scores on the PANSS, and their caregivers experienced a greater burden due to the illness. However, patients’ dissatisfaction with family support was similar in the two groups.

Table 1. Clinical and family characteristics of patients with schizophrenia who has or has not disability based on the WHODAS II
3.4 Correlations between disability and other characteristics of the patients
As shown in Table 2, participants with more severe disability had a younger age of onset, a longer duration of illness and more prominent negative symptoms.Patients with higher levels of disability also reported greater dissatisfaction with family support and the family members of patients with more severe disability reported higher levels of burden in five of the six domains of burden assessed by the FBIS. However,WHODAS II scores were not significantly related with the age of the patient, number of relapses or number of hospitalizations.
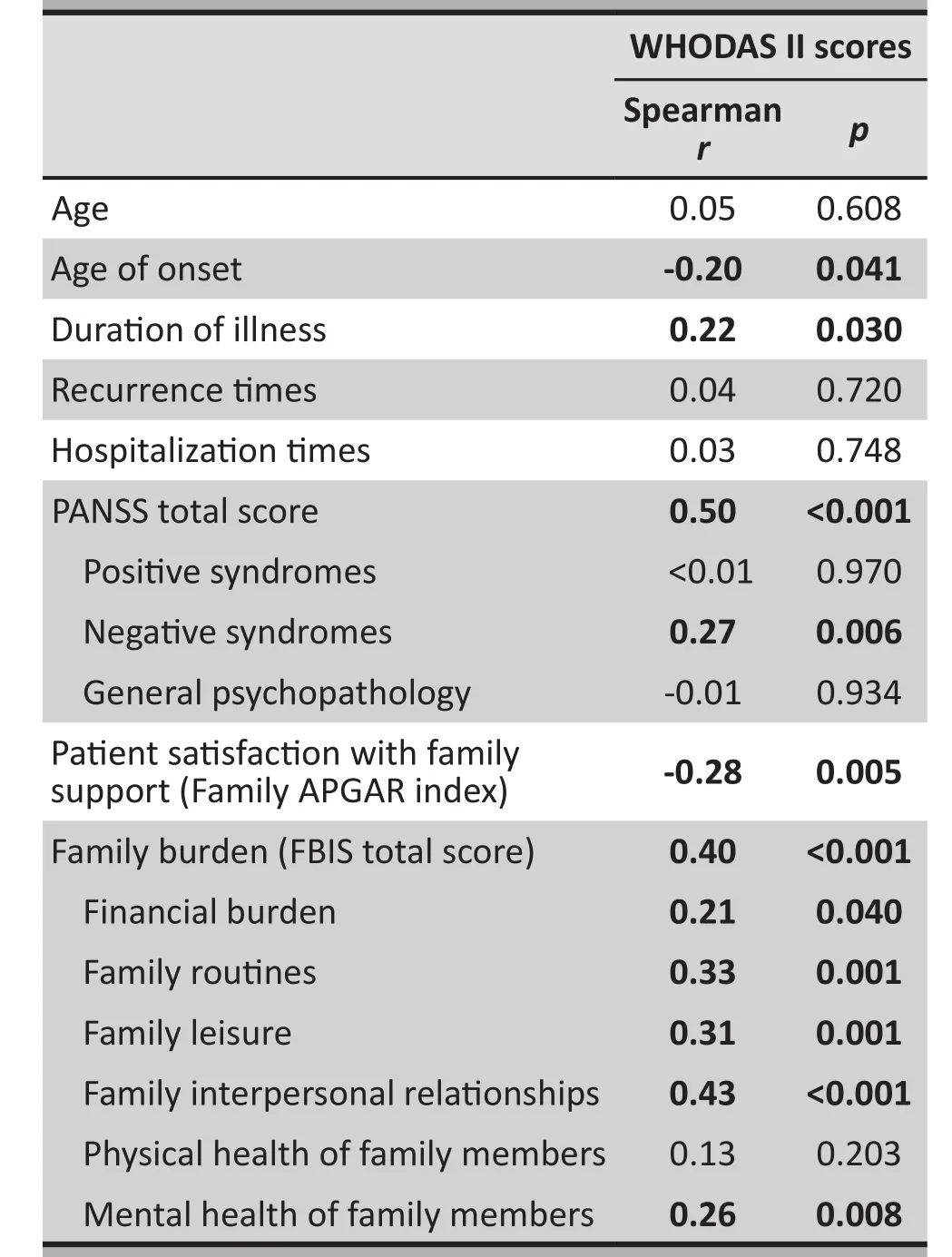
Table 2. Correlations between the WHO Disability Assessment Schedule II (WHODAS II) scores and other clinical or family characteristics among 101 patients with schizophrenia
3.5 Factors associated with the severity of disability
Multivariate analyses were used to identify factors that were independently associated with psychiatric disability. The result of the stepwise logistic regression analysis that used disability versus no disability (based on the WHODAS II cutoff score of 51) as the dependent variable and all variables that were statistically significant in the univariate analysis (Table 1) as independent variables is shown in Table 3. Compared to patients who did not meet the WHODAS II criteria for disability, those who met disability criteria had more severe clinical symptoms (i.e., higher overall PANSS scores) and their family members experienced a higher level of burden.
Considering disability as a continuous variable(instead of as a dichotomous variable), we used the total WHODAS II score as the dependent variable and all variables that were signif i cantly associated with the total score in the univariate analysis (Table 2) as independent variables in a stepwise general linear regression analysis.As shown in Table 4, four factors were retained using the backward stepwise selection method: PANSS total score,family APGAR index, FBIS total score and the duration of illness. Thus compared to patients with lower levels of disability, patients with higher levels of disability had a greater level of psychopathology, a longer duration of illness and reported greater dissatisfaction with family support; moreover, their family members reported higher levels of family burden.
4. Discussion
4.1 Main findings
Among the 101 patients with clinically stable schizophrenia recruited for the study from the outpatient department of a large psychiatric hospital in central China, 74 (73%) had clinically significant disability as assessed by an internationally standardized tool for evaluating disability – the WHODAS II. This high level of disability is consistent with previous studies in China,[2,3,5]and highlights the limitations of our current treatment regimens for schizophrenia that can control symptoms but do not rehabilitate patients. As expected,high levels of disability were positively correlated with an early age of onset (associated with more severe forms of schizophrenia), a longer duration of illness(associated with greater deterioration in functioning)and more severe clinical symptoms in the previous month (particularly the avolitional negative symptoms).Perhaps less obvious (but still understandable), higher degrees of disability in the patient were also associated with a greater burden on the family in terms of family finances (71% of the patients were unemployed),family functioning, interpersonal relationships, and the psychological wellbeing of other family members.In the univariate analysis the degree of disability was also positively correlated with patients’ level of dissatisfaction with the support provided by the family.After controlling for other variables in multivariate analyses, the current severity of symptoms (particularly negative symptoms) and the degree of family burden reported by a family member informant were the only factors that remained independently associated with the level of disability of the patient.
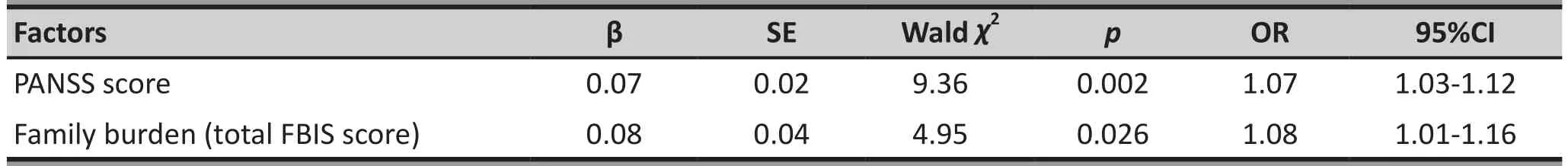
Table 3. Logistic regression analysis of factors associated with the WHO Disability Assessment Schedule II(WHODAS II) scores among patients with schizophrenia (n=101)
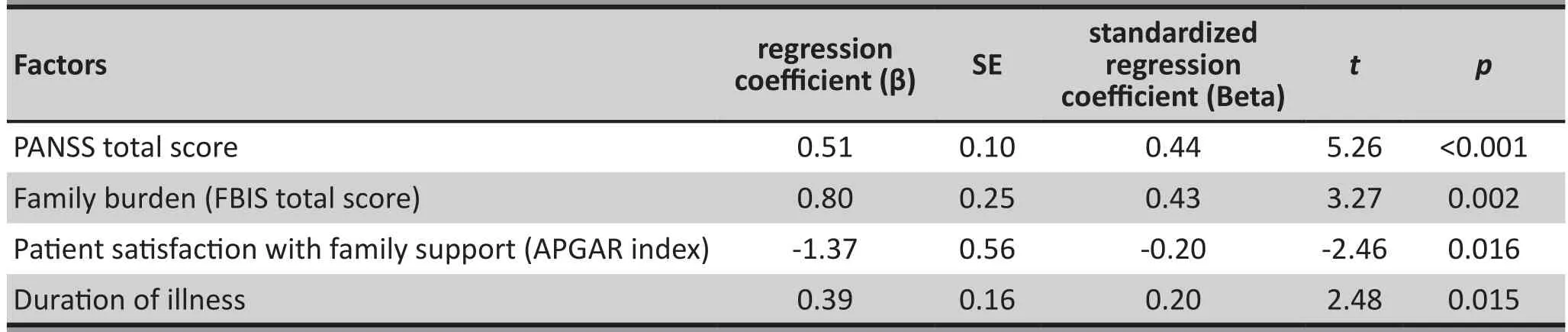
Table 4. Stepwise linear regression of factors associated with the WHO Disability Assessment Schedule II(WHODAS II) scores among 101 patients with schizophrenia
4.2 Limitations
Only 11% of eligible participants completed the survey;so the representativeness and generalizability of the results to the families of individuals with schizophrenia in treatment in China is uncertain. However, the main reason for non-participation was that patients and their family members left the outpatient clinic immediately after treatment and, thus, were not approached by the research team, so this low participation rate may not necessarily mean that the participating families were unrepresentative. A better, but more expensive,recruitment strategy would be to visit potential participants in their homes.
This is a cross-sectional study so the causal direction of the variables identified remains unknown.For example, more serious negative symptoms of schizophrenia may cause increased disability but increased disability could also increase the severity or duration of negative symptoms. The relationships of family burden, patient symptomatology, and patient disability are probably quite complex and change overtime; a cross-sectional design is not able to assess the nuances of the interactions between these variables.Prospective studies that follow patients and all their family members regularly from the time of first diagnosis are needed to clarify these issues. Ideally this line of research would start with qualitative studies to ensure that all the relevant factors that moderate the interactions of these three core constructs are included in the theoretical models and in subsequent quantitative studies.
Given the large number of potential confounding variables that could affect the relationship between family burden and patient disability, our sample size of 101 patients was insufficient to conduct the stratified analyses (e.g., by economic level of the family, urban v.rural residence, etc.) that could help generate a more comprehensive understanding of family burden and patient disability.
4.3 Implications
This study convincingly demonstrates that the level of disability experienced by patients with schizophrenia is independently associated with family burden even after adjusting for symptom severity. This highlights the importance of targeting both symptoms and disability in treatment strategies for schizophrenia. Multiple studies have shown that rehabilitation training can improve the clinical condition, treatment adherence and social functioning of patients with schizophrenia.[13,14]Based on the findings of this study, rehabilitation programs to prevent disability should prioritize patients with an early age of onset and a longer duration of illness.
We also found that patients who were dissatisfied with the support they receive from family members had higher levels of disability. The causal direction of this association is unclear – it is probably bidirectional– but this finding highlights the centrality of the family as a target for decreasing the disability associated with schizophrenia. In our study, 91% of the patients were living with their family members, so the family is the primary environment for social interaction for these patients. Previous studies have found that patients with higher levels of family support report a higher quality of life,[15,16]are less likely to have suicidal behavior,[17]and have shorter periods of untreated psychosis.[18]Many issues and difficulties exist in the interactions between family caregivers and schizophrenia patients, so training family members about the proper expression of emotions and helping them develop appropriate coping strategies are potential methods for reducing family burden and, thus, decreasing patient disability.[19,20]
This study found that the majority of clinically stable outpatients with schizophrenia were unemployed and living at home with family members. The treatment expenses and the loss of productivity of both the patient and the family caregivers pose substantial financial burdens on the family. This problem exists in both high-income and low- and middle-income countries:a survey conducted by Magliano and colleagues[21]reported that 45% of the caregivers of patients with schizophrenia reported high burden and little support from society. These problems are magnified by stigma and discrimination of patients and, often, their family members. Phillips and colleagues[22]report that in China stigma is a major source of psychological stress for both patients with schizophrenia and their family members,and it signif i cantly disturbs the daily lives of caregivers.Our results also suggest that the disability associated with schizophrenia greatly disrupts family activities and undermines the psychological wellbeing of other family members. These findings highlight the need to provide financial support to families with schizophrenic members and to provide educational and social support to family caregivers to help them assume the difficult, often life-long, task of caring for their ill family members.
In our study 92 (93%) of the patients were living with close relatives, a proportion that is much higher than that reported in Western countries but is, we believe,representative of China and, possibly, of other lowand middle-income countries. The burden experienced by these family members in terms of lost productivity and emotional turmoil are substantial components of the overall social cost of schizophrenia that are not considered in standard metrics of the burden of illness(i.e., Disability Adjusted Life Years, DALYs). This study confirms the importance of considering family burden when evaluating the social and economic importance of different health conditions, particularly severe mental disorders.
Conflict of interest
The authors report no conflict of interest related to this manuscript.
Funding
This work was funded by the Science and Technology Support Program of the Chengdu Science and Technology Bureau (No. 11PPYB055SF-027) ‘Community Rehabilitation and Life Quality of Patients with Schizophrenia project’. It was also funded by the Science and Technology Program of the Health Department of Sichuan Province (No. 130016) ‘Family Intervention and Rehabilitation of First Onset Schizophrenia Patients’project.
1. Jiang KD. [Psychiatry]. Beijing: People’s Medical Publishing House; 2006. p. 109. Chinese
2. Chen X, Huang DF, Lin AH, Li H, Liu P, Chen SZ, et al. [Causes and countermeasures study on psychiatric disabled adults in Guangdong province]. Zhongguo Kang Fu Yi Xue Za Zhi. 2009;24(10): 938-941. Chinese. doi: http://dx.doi.org/10.3969/j.issn.1001-1242.2009.10.021
3. Li CL, Zhao ZQ, Zhou B. [Analysis of the investigation results of mental disability in Ningxia]. Ningxia Yi Xue Za Zhi. 2008;30(11): 1041-1042. Chinese. doi: http://dx.doi.org/10.3969/j.issn.1001-5949.2008.11.050
4. R?ssler W, Salize HJ, van Os J, Riecher-R?ssler A. Size of burden of schizophrenia and psychotic disorders. Eur Neuropsychopharmacol. 2005;15(4): 399-409. doi: http://dx.doi.org/10.1016/j.euroneuro.2005.04.009
5. Hu MY, Shen TY. [An investigation of mental disability in schizophrenia and its risk factors related]. Zhonghua Xing Wei Yi Xue Yu Nao Ke Xue Za Zhi. 2005;14(10):899-900. Chinese. doi: http://dx.doi.org/10.3760/cma.j.issn.1674-6554.2005.10.014
6. World Health Organization. International Statistical Classif i cation of Disease and Related Health Problems, 10thRevision. Geneva: World Health Organization, 1992.
7. Zhang AM, Cai FM, Lu YH, Sun T. [The WHO Disability Assessment Schedule (WHO-DAS II) and its relation with ICF]. Zhongguo Kang Fu Li Lun Yu Shi Jian. 2003;9(1): 15-17. Chinese. doi: http://dx.doi.org/10.3969/j.issn.1006-9771.2003.01.007
8. Zhang ZJ. [Handbook of Behavioral Medical Scales]. Beijing:Chinese Medical Electronic and Audio-visual Publishing House 2005: 355-359. Chinese
9. Wang LE, Zhou J, Jin H. [Reliability and validity of the Chinese version of WHO Disability Assessment Schedule 2.0 in mental disability assessment]. Zhongguo Xin Li Wei Sheng Za Zhi. 2013;27(2): 121-125. Chinese. doi: http://dx.doi.org/10.3969/j.issn.1000-6729.2013.02.008
10. Smilkstein G. The family APGAR: a proposal for a family function test and its use by physicians. J Fam Pract. 1978;6:1231-1239.
11. Chau TT, Hsiao TM, Huang CT, Liu HW. [A preliminary study of family APGAR index in the Chinese]. Gaoxiong Yi Xue Ke Xue Za Zhi. 1991;7: 27-31. Chinese
12. Li J, Xiang MZ, Gao DJ, He J. [The reliability and validity test report of psychiatric patient’s family burden scale]. Hua Xi Yi Xue. 1997;12(1): 11-13. Chinese
13. Ma Y, Li ZJ, Xu ZY, Guo ZH, Qu Y, Wang XQ. [Effects of cognitive behavioral therapy on quality of life in patients with schizophrenia: A single blind randomized controlled study]. Zhongguo Xin Li Wei Sheng Za Zhi. 2012;6(11):801-807. Chinese. doi: http://dx.doi.org/10.3969/j.issn.1000-6729.2012.11.001
14. Guan LL, Du LZ, Ma H. [Burden of schizophrenia: A review].Zhongguo Xin Li Wei Sheng Za Zhi. 2012;26(12): 913-918.Chinese
15. Sun Y, Chen HC, Xu X. [Influence of family nursing intervention on prognosis of schizophrenia]. Hu Shi Jing Xiu Za Zhi. 2008;23(6): 560-562. Chinese. doi: http://dx.doi.org/10.3969/j.issn.1002-6975.2008.06.038
16. Liu L, Li CP, Zeng ZX, Fu FZ. [The influence of family caring and self-efficacy on the quality of life in patients with schizophrenia during recovery period]. Guo Ji Hu Li Xue Za Zhi. 2012;31(6): 975-977. Chinese. doi: http://dx.doi.org/10.3760/cma.j.issn.1673-4351.2012.06.006
17. Chen YR, Chen PZ, Liu SW. [A study on suicide behaviors of community patients with schizophrenia]. Zhongguo Min Kang Yi Xue. 2009;21(11): 1226-1230. Chinese. doi: http://dx.doi.org/10.3969/j.issn.1672-0369.2009.11.009
18. Long B, Yi ZH, Zhu LP, Wang JJ. [Analysis on correlation of DUP with family function and psychiatric symptom in schizophrenics with psychosis relapse]. Shen Jing Ke Xue Yu Jing Shen Wei Sheng Za Zhi. 2010;10(2): 162-164. Chinese
19. Hou YZ, Xiang YT, Li WY, Gao L, Chen GL, Weng YZ.[Family adaptability and cohesion and social functioning of 70 community outpatients with schizophrenia in Beijing]. Zhongguo Lin Chuang Kang Fu. 2003;7(21):2946-2947. Chinese. doi: http://dx.doi.org/10.3321/j.issn:1673-8225.2003.21.008
20. Zhang L, Ju K, Zhang L, Shen ZH. [Investigation of family care and coping style of the inpatients with schizophrenia].Shanghai Jing Shen Yi Xue. 2008;20(6): 346-362. Chinese
21. Magliano L, Fiorillo A, De Rosa C. Family burden in long-term diseases: a comparative study in schizophrenia vs. physical disorders. Soc Sci Med. 2005;61(2): 313-322. doi: http://dx.doi.org/10.1016/j.socscimed.2004.11.064
22. Phillips MR, Yang GH, Li S, Li Y. Suicide and the unique prevalence pattern of schizophrenia in mainland China: a retrospective observational study. Lancet. 2004;364(9439):1062-1068. doi: http://dx.doi.org/10.1016/S0140-6736(04)17061-X
對中國四川精神分裂癥患者癥狀、殘疾及家庭負擔之間關系的橫斷面調查
張倬秋, 鄧紅, 陳穎, 李水英, 周茜, 賴華, 劉麗芳, 劉玲, 申文武
數據監測委員會、臨床試驗、中期分析、生物統計學
Background:Schizophrenia is a chronic condition that leads to high rates of disability and high levels of family burden but the interactive relationship between these variables remains unclear, particularly in low- and middle-income countries where the vast majority of patients live with their families.Aim:Assess the symptom severity, level of disability, and family burden among clinically stable outpatients with schizophrenia in Sichuan, China.Methods:A total of 101 clinically stable outpatients with schizophrenia who had a median duration of illness of five years were assessed using the World Health Organization Disability Assessment Scale 2.0 (WHODAS II), the Positive and Negative Syndrome Scale (PANSS) and the Family Adaptation, Partnership, Growth, Affection and Resolve Index scale (APGAR); and their caregivers were surveyed using the Family Burden Interview Schedule(FBIS).Results:Among the 101 patients, 92 lived with their immediate family members, 74 had clinically significant disability, and 73 were unemployed. The level of disability was associated with the severity of symptoms(r=0.50, p<0.001), duration of illnesses (r=0.22, p=0.028), age of onset (r=-0.22, p=0.024) and patients’ level of satisfaction with family support (r=-0.30, p=0.020). Disability was also associated with the overall level of family burden (r=0.40, p<0.001), and with several subtypes of family burden: financial burden (r=0.21, p=0.040), the degree of disruption in family routines (r=0.33, p=0.001), the effect on family leisure activities (r=0.31, p=0.001)and the quality of family interactions (r=0.43, p<0.001). Four variables remained significantly associated with the level of disability in the stepwise multivariate linear regression: duration of illness, severity of symptoms,patient satisfaction with family support, and the overall burden of the illness on the family.Conclusions:Even after adjusting for the severity of patients’ symptoms, patient disability is independently associated with family burden. This highlights the importance of targeting both symptoms and disability in treatment strategies for this severe, often lifelong, condition. In countries like China where most individuals with schizophrenia live with their families, family burden is an important component of the impact of the illness on the community that should be included in measures of the relative social and economic importance of the condition.
http://dx.doi.org/10.3969/j.issn.1002-0829.2014.01.004
The Mental Health Center of West China Hospital, Sichuan University, Chengdu, Sichuan Province, China
*correspondence: wenwu_shen@163.com
A full-text Chinese translation will be available at www.saponline.org from April 15, 2014.
背景:精神分裂癥是一種慢性疾病,其致殘率高、家庭負擔重,但這些因素之間的相互關系仍不清楚,尤其是在絕大多數患者與家人同住的中低等收入國家。目標:評估中國四川省定期門診精神分裂癥患者的癥狀嚴重程度、傷殘等級與家庭負擔情況。方法:共有101例定期門診的精神分裂癥患者納入研究患者病程中位數為5年。研究采用世界衛生組織殘疾評定量表2.0(WHODAS II),陽性和陰性癥狀量表(PANSS)以及家庭適應、共處、成長、情感和解決指數量表(APGAR)進行評估,對患者的照顧者采用家庭負擔會談量表(FBIS)進行調查。結果:101例患者中,92例與他們的直系親屬住在一起,74例有顯著臨床殘疾, 73例失業。殘疾等級與癥狀嚴重程度(r=0.50,p<0.001)、病程(r=0.22,p=0.028)、發病年齡(r=-0.22,p=0.024)以及患者對家庭支持的滿意度(r=-0.30,p=0.020)相關。殘疾等級也與家庭總體負擔相關(r=0.40,p<0.001),包括家庭負擔的幾種亞型:財政負擔(r=0.21,p=0.040)、家庭日常的破壞程度(r=0.33,p=0.001)、家庭休閑活動的影響(r=0.31,p=0.001)和家庭互動的質量(r=0.43,p<0.001)。逐步多元線性回歸分析后有四個因素與殘疾等級顯著相關:病程、癥狀嚴重程度、病人對家庭支持的滿意度以及疾病對家庭的總體負擔。結論:即使在調整了患者癥狀嚴重程度后,患者殘疾仍然與家庭負擔獨立相關。這突出表明了對于精神分裂癥這種往往伴隨終身的嚴重的疾病制定治療方案時不僅要針對癥狀還應關注殘疾情況。在像中國這樣的國家,大多數精神分裂癥患者與家人同住,家庭負擔成為該疾病對社會影響的一個重要組成部分,因此在評估精神分裂癥的社會經濟影響時應同時測量患者帶來的家庭負擔。
(received: 2013-09-23; accepted: 2013-11-14)

Zhouqiu Zhang obtained her bachelor’s degree in Nursing from the Nursing School of West China Medical University in 1987. She has worked in the Mental Health Center of West China Hospital, Sichuan University since graduation. She is currently head nurse of a psychiatric ward and teaches psychiatric nursing at Sichuan University. Her research interest is the integration of hospital rehabilitation and community rehabilitation for persons with severe mental disorders.
- 上海精神醫學的其它文章
- Establishing a data monitoring committee for clinical trials
- Challenges in the diagnosis and treatment of transsexualism in contemporary China
- Case report of refractory tardive dystonia induced by olanzapine
- Duration of untreated psychosis and clinical outcomes of firstepisode schizophrenia: a 4-year follow-up study
- Five-year follow-up study of multi-domain cognitive training for healthy elderly community members
- Randomized controlled trial of four protocols of repetitive transcranial magnetic stimulation for treating the negative symptoms of schizophrenia