Cross-cultural adaptation and validation of the Indonesian version of the Critical-care Pain Observation Tool
Luthfi Fauzy Asriyanto ,Nur Chayati
aMaster of Nursing Program,Postgraduate Program,Universitas Muhammadiyah Yogyakarta,Indonesia
b School of Nursing,Faculty of Medicine and Health Sciences,Universitas Muhammadiyah Yogyakarta,Indonesia
Keywords:
ABSTRACT Objective:The Critical-care Pain Observation Tool (CPOT) is one of the most accurate methods for assessing pain in ICU patients with critical illness and/or a decreased level of consciousness (LOC).This study aimed to determine the validity and reliability of the Indonesian version of the CPOT.Methods:The English version of CPOT was translated into the Indonesian version following five steps:initial translation,synthesis of instrument translation results,back translation,validation of the instrument by an expert committee,and testing of the Indonesian instrument.Between September and December 2022,a total of 52 ICU patients from four hospitals in Indonesia were evaluated for pain at rest,during body-turning procedure,and 15 minutes after the procedure using the CPOT.The researcher used the verbal Faces Pain Thermometer (FPT) instrument as a gold standard to assess the CPOT’s criteria validity.Validity assessments included content and criterion validity.Reliability was evaluated using Cronbach’s α coefficient and interrater reliability.Results:Higher CPOT scores were found during the body-turning procedure than at rest and after the procedure.The instrument’s item-content validity index(I-CVI)ranged from 0.75 to 1.00,and the overall instrument’s average scale-level content validity index (S-CVI/Ave) was 0.93.The statistical analysis revealed a positive correlation(r)between the CPOT and the patient’s FPT scores(0.877-0.983,P <0.01).The significant agreement amongst raters (κ) revealed the inter-rater reliability of the CPOT (0.739 -0.834,P <0.01).Conclusion:The Indonesian version of the CPOT has been proven valid and reliable in assessing pain in patients with critical illness and/or decreased LOC.
What is known?
· Effective pain management is a crucial element of quality care for patients in the ICU.These actions consist of the identification of pain,the implementation of pain therapies,and the repeated evaluation of pain.
· Pain assessment in patients in the ICU is more accurate using pain assessment instruments based on patient behavior.
· The Critical-care Pain Observation Tool (CPOT) is one of the finest behavioral observation-based pain assessment instruments for psychometric analysis and clinical feasibility testing.
What is new?
· This study translated the CPOT into Indonesian and verified its reliability and validity.
· Nurses can use the Indonesian version of the CPOT to assess pain in patients with a decreased level of consciousness in the ICU.
1.Introduction
Pain is an irritating sensory experience that is frequently the major cause of a person’s visit to a healthcare facility [1,2].A research study states that approximately 80% of patients receiving treatment in the intensive care unit(ICU)indicate signs of pain[3].The experience of pain is often a bad memory for patients being treated in the ICU until it continues when the patient is discharged from the hospital [4].Pain impairs the patient’s physiological and psychological functions,hinders the healing process,and even poses a threat to their life[5].The patient’s physiological responses to pain include instability of hemodynamic function,impaired immune system function,hyperglycemia,and increased secretion of catecholamine and cortisol hormones.Uncontrolled pain also results in various psychological problems,including sleep deprivation,anxiety,and mental condition changes [6,7].
Effective pain management is a crucial element of quality care for patients in the ICU [8,9].These actions begin with the identification of pain,followed by the implementation of pain therapies and the repeated evaluation of pain[7].The most valid approach for assessing pain is the patient’s verbal report [6,10];however,pain instruments based on verbal reports are frequently inapplicable to critically ill patients in the ICU.Unstable hemodynamic conditions,mechanical ventilation devices,and various types of sedative therapies affect the patient’s ability to communicate verbally or change the level of consciousness (LOC) [6,11].The inability of the patient to report pain presents challenges in the process of assessing pain,making patients susceptible to obtaining inadequate pain treatment [12,13].
The Society of Critical Care Medicine (SCCM) and the Pain Agitation/Sedation,Delirium,Immobility,and Sleep Disruption clinical practice guidelines state that the first element of a pain management strategy in patients in the ICU is adequate pain assessment[8,14].Nurses play a vital role in figuring out how much pain a patient is in using their intuition,knowledge,and clinical experience [10,15].To identify pain in ICU patients,nurses may utilize various alternative methods,such as observation of patient behavior and physiological indicators [5,16].The patient’s nonverbal behavior,which can be recognized as a manifestation of pain,is expressed through facial expressions,body movements,activities,and changes in interpersonal interactions and mental states[13].Pain causes disturbances in the body’s physiological and hemodynamic functions;therefore,reflex dilation of the pupil,skin conductance index,heart rate variability,and electrical brain activity,especially the delta waves,can be important indicators in recognizing pain [17,18].
The research results of Khanna et al.[19]and Lin et al.[18]stated that using certain physiological indicators as pain markers still requires further validation studies.Empirical evidence suggests that numerous medications can cause changes in patients’physiological function and pathophysiological states [16];therefore,physiological markers,such as vital signs,cannot be utilized as the sole indicator in evaluating pain [4,8].Various research studies have supported behavioral observation techniques as a valid approach for measuring pain in patients unable to express their pain vocally [13,20],as Asriyanto and Chayati’s literature review analysis demonstrates that the Critical-care Pain Observation Tool (CPOT) has greater validity than different physiological indicators [21].
The CPOT is a pain assessment instrument developed byetal.to assess pain in adult patients in the ICU [22].This instrument evaluated the patient’s nonverbal behavior,including facial expressions,body movements,adherence to the ventilator(or vocalizations for patients who were not intubated),and muscle tension during passive movements.Each behavioral indicator has a range of values between 0 and 2,hence the instrument’s total value of 8.A CPOT score ≥3 indicates significant pain [14,23].Regarding psychometric analysis and clinical feasibility testing,the CPOT is the finest tool compared to similar instruments[10].The CPOT can increase nurses’ability to detect pain and conduct pain evaluations [1,24] effectively.
Nurses have an important role in the pain management process for patients in the ICU.One of the nurses’responsibilities is to carry out continuous pain assessments using appropriate pain instruments so that the effectiveness of pain management through a multimodal analgesic approach can be achieved[10].The CPOT has been proven valid and reliable in detecting pain in patients with critical illnesses and decreasing LOC through research studies in several countries,such as Denmark[25],Italy[26],and Poland[27].Several studies in Indonesia have employed the CPOT in the Indonesian language to evaluate pain and a reduced LOC in patients with severe illness[28-30].Even though it has been used,there is a limitation in previous research studies:the process of adapting the CPOT from the original English version is less demonstrated in standardized steps in the Indonesian version.This study aimed to adapt and validate the Indonesian version of the CPOT through the cross-cultural adaptation.The researchers also intend to prove the validity and reliability of the Indonesian version of the CPOT for assessing pain in patients with critical illness and/or a decreased LOC.
2.Methods
2.1.Study design
This research is divided into two parts: the first part is the translation content,and the second part is the validity test.Researchers carried out the process of adapting CPOT based on guidelines from Beaton et al.[31,32],including the following steps:1) initial translation of the instrument;2) synthesis of instrument translation results;3)instrument back translation;4)validation of the instrument by an expert committee;and 5) testing of the Indonesian version of the CPOT.
2.2.Ethical considerations
This research has obtained permission from the Health Research Ethics Committee (Komite Etik Penelitian Kesehatan/KEPK) as follows: KEPK RS PKU Muhammadiyah Temanggung Number 1351C/III/RSMT/KET/2022;KEPK RSUD Kabupaten Temanggung Number 19/EC/KEPK_RSUD.TMG/VII/2022;and KEPK RS PKU Muhammadiyah Gamping Number 181/KEP-PKU/X/2022.This study adhered to the Belmont Report’s standards,including respect for persons,beneficence and non-maleficence,and justice.All participants,through their guardians,provided written informed consent regarding their involvement in the study.Information regarding participants’ data is guaranteed to be kept confidential,and each participant gets the same rights and treatment in the study.
2.3.Translation procedure
The entire translation process of the CPOT is carried out by paying attention to linguistic,phrasal,contextual,and cultural aspects so that the translation results have the same meaning as the original version of the CPOT [33,34].The CPOT adaptation process begins with a request for permission to use and translate the CPOT from the first authorand owner of the CPOT license for the English version: the American Association of Critical-care Nurses (AACN).The initial translation of the English version of the CPOT into Indonesian was accomplished by two independent bilingual translators with nursing (N.Purborini) and non-health profession backgrounds (I.Aristiyono).The author reviewed the translation results of the two translators and found differences in several sentence phrases,including body movements,compliance with ventilator indicators,vocalization,and muscle tension indicators.Researchers and the two translators then reached a consensus to synthesize the instrument’s initials using the standard Indonesian grammatical structure.In the subsequent step,the CPOT emerging from the synthesis was translated back into English by two different independent translators,one of whom was a lecturer in nursing (E.Rochmawati) and the other a linguist (T.W.Kartika)[35].Researchers and translators replaced several unusual sentence phrases with phrases that conform to standard Indonesian;for example,‘Contraction of the upper and lower face’ was replaced with ‘The contraction of the upper and lower facial muscles’ to indicate the specific part of the body organ that was undergoing changes.The sentence ‘Alarms not activated’ changed to ‘Alarm is not activated,’ which indicated that the output of the mechanical ventilator had changed due to patient activity.
2.4.Instrument testing and psychometric analysis
2.4.1.Study settings
This study was conducted in four hospitals that have generaltype ICUs,including PKU Muhammadiyah Temanggung Hospital,the Regional Hospital of Temanggung Regency,Ngesti Waluyo Parakan Christian Hospital,and PKU Muhammadiyah Gamping Hospital.Testing the validity and reliability of the Indonesian version of the CPOT was carried out from September 18 to December 8,2022.
2.4.2.Participants
The participants in this study were ICU patients with critical illnesses and/or decreased LOC.The study sample was selected using the following inclusion criteria:1)adult patients over the age of 18;2) the patients have a Glasgow Coma Scale (GCS) score ≥6,and 3) The patients have no constraints or contraindications to position change.The following criteria were used to exclude patients from the study: 1) the patient had paralysis of all four extremities;2) patients with intellectual impairment,epilepsy history,a psychiatric diagnosis,and chronic pain history;3) patients in a condition of deep sedation (Richmond Agitation and Sedation Scale [RASS] score ≥-4) or receiving neuromuscular blocking agents;4) patients in a state of agitation or RASS score≥+3;and 5)patients suspected of experiencing brain stem death.
Participants in this study were selected using the consecutive sampling method,while the number of research samples was established utilizing a ratio approach because there are no fixed guidelines for determining samples in validation research.Most authors use a sample size estimation method with a margin of 3-20 [36].Based on the majority (63.2%) of previously conducted validation studies,researchers utilize a ratio item-to-subject of 10:1,requiring at least 40 participants [34,37].To enable psychometric analysis of the CPOT,we used 52 participants,consisting of 13 conscious patients and 39 patients with decreased LOC.The validity and reliability of the CPOT were evaluated by the researcher and nine clinical nurses from each study site.The selection requirements for the assessment team were a bachelor’s degree and clinical experience as a level ??? nurse.
2.4.3.Measurement
2.4.3.1.Indonesian version of the CPOT.The Indonesian version of CPOT is similar to the original version but has been adapted to the structure of the Indonesian language.This instrument consists of four indicators that describe the patient’s nonverbal behavior,including facial expression,body movements,muscle tension,and compliance with ventilation for intubated patients(or the patient’s verbal response for non-intubated patients).Each item in the indicators was scored between 0 and 2,with a possible total CPOT score ranging from 0 (no pain) to 8 (maximal pain).The assessor assigns a score according to the observed patient behavior.A score of less than 3 is interpreted as mild pain,while a score of 7-8 indicates the patient is experiencing severe pain [23,38].The Indonesian version of the CPOT is presented in Appendix A.
2.4.3.2.The Faces Pain Thermometer instrument.The Faces Pain Thermometer (FPT) instrument is a pain assessment tool that can be used to identify pain intensity in adult patients with critical illnesses.This tool is illustrated as a thermometer with a scale ranging from 0(no pain)to 10(highest pain)and contains six verbal descriptions of pain,namely no pain,mild pain,moderate pain,severe pain,very severe pain,and unbearable pain.The validity of the FPT instrument has been proven through good convergent validity and discriminant validity values when testing the instrument on patients admitted to the ICU for cardiac surgery indications [39,40].
2.4.4.Data collection
The process of collecting research data begins with the activity of sharing perceptions about the Indonesian version of the CPOT by researchers with the clinical nurse in a small group discussion format for 45-60 min.An exercise followed this activity in independently assessing pain in patients treated in the ICU.The CPOT total score results of each assessor were evaluated;if there was a difference in the CPOT total score ≥2,the researcher clarified it so that each assessor could carry out an accurate and standardized assessment of pain [41].
Each hospital’s assessor coordinator selected participants based on inclusion and exclusion criteria,including age,degree of consciousness using GCS,level of sedation-agitation using RASS,drug class received,and medical history.Research data collection began with the provision of information and consent before the study and continued until 52 patients were enrolled.Pain assessment for each participant was carried out by two assessors using a nociceptive procedure:body-turning.Based on previous research,body turning is one of the ICU procedures that causes pain in critically ill patients [3,5].The assessors observed nonverbal pain behavior when the patient was at rest (not receiving any medical procedures),during the body-turning procedure,and 15 min after the body-turning procedure.The next step was for researchers to identify patients who could still express their pain,both verbally and through motion,to obtain data regarding the patient’s pain intensity.The patient then undergoes a body-turning procedure and is asked simple questions regarding the pain scale using verbal descriptions: mild,moderate,severe,very severe,or unbearable pain based on the FPT instrument.
2.4.5.Data analysis
This study utilized the Jamovi Statistics Application version 2.3.18 for data analysis.The significance value of the statistical test was set at P <0.05.The participant characteristics were presented with either means or numbers and percentages.
The validity test in this research consists of two types of validity:content validity and criterion validity.Validity can be interpreted as the ability of an instrument to carry out the measurement function precisely on the object to be measured[35].The content validity of the initial version of the CPOT was evaluated using an approach based on expert judgment.This evaluation involved eight experts,including health research methodologists (I.Permana),health professionals (A.Supriyono;E.Y.Akhmad),nursing lecturers (S.Haryatmo;Wantonoro;A.Mustofa;S.Fathonah),and language professionals(I.D.Retnowati).Experts were requested to conduct a rational analysis of the clarity and relevance of instrument items using a 4-point Likert scale.A score of 3 or 4 on each item-level content validity index (I-CVI) indicates the instrument’s item is clear(1,not clear;4,very clear)and relevant(1,not relevant;4,very relevant) [42,43].According to expert judgment,the CPOT is regarded as valid and acceptable if it obtains an average scale-level content validity index (S-CVI) ≥0.80 [44,45].
The criterion validity of the CPOT is ensured by comparing the results of the instrument assessment against standards that are considered standard values,namely the patient’s verbal report regarding pain [34,35].Researchers used the FPT instrument as a standard value to obtain participant pain scale data.Spearman’s rank correlation test was utilized to examine the validity of the correlation between the CPOT assessment and the FPT score.The assessment results are deemed legitimate and acceptable if their correlation coefficient is ≥0.60[46,47].The correlation coefficient between the results of the CPOT assessment and the FPT score also shows the construct validity of the Indonesian version of the CPOT [35].
Reliability shows the extent to which an instrument provides relatively consistent measurement results when carried out two times or more [34].In this study,the CPOT’s internal consistency reliability was evaluated using Cronbach’s α coefficient and interrater reliability,namely the consistency of measurement outcomes between raters for the same set of participants during an assessment episode.Each rater performed pain assessments on the same participant in three equal time episodes: at rest,during the body-turning procedure,and 15 min after the procedure.The Kappa statistic was utilized to check the level of correlation between the two raters across the three assessment episodes.An instrument is considered reliable if its statistical Kappa test value is ≥0.61 [35,48].
3.Results
3.1.Characteristics of the participants
This study included 52 patients aged 28-84 years and an average age of 61.65 years(SD=12.51).The mean length of stay in ICU was 2.0 days.More than half of the patients were male(51.9%),and the majority of ICU admissions were for neurological illnesses (32.7%),which included encephalitis,hemorrhagic stroke,and ischemic stroke.The majority of participants had a lowered level of consciousness;the majority of the participants were calm and lightly sedated;and the majority did not get analgesic medications (Table 1).
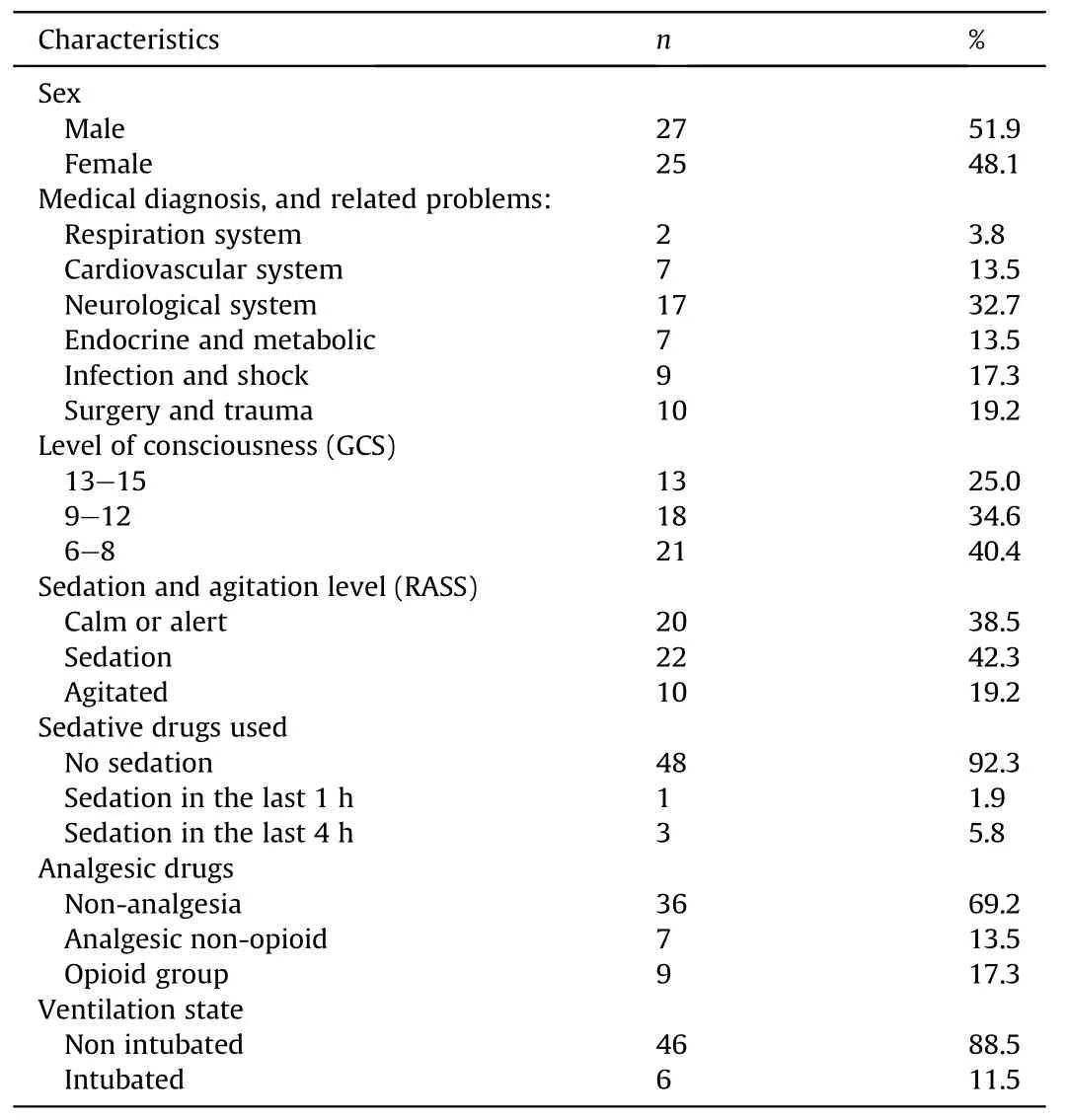
Table 1 Demographic and clinical characteristics of participants (n=52).
The results of the descriptive analysis illustrate that there was an increase in the mean value of the CPOT when participants received the body-turning procedure.The lowest mean value of the CPOT was obtained in the group of participants who received nonopioid analgesic therapy(Rater 1=2.14;Rater 2=2.29)(Table 2).
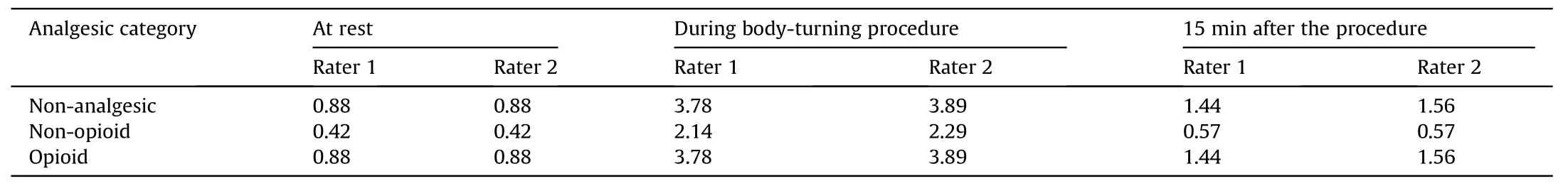
Table 2 CPOT scores in various analgesic categories (n=52).
3.2.Validity
3.2.1.Content validity
The I-CVI results show that all items in the instrument indicators scored 0.75-1.00,with the lowest I-CVI value in the‘Compliance with the Ventilator’ indicator (0.75).The expert judgment-based CVI assessment of the initial version of the CPOT by eight experts obtained an S-CVI value of 0.93,indicating valid and acceptable translational validity.
3.2.2.Criterion validity
Thirteen participants who could communicate pain verbally or by signs rated discomfort according to the following descriptors:no pain,mild pain,moderate pain,and severe pain.The researchers discovered four patients who complained of minor pain at rest,while nine others did not.During body-turning procedures,the majority of volunteers (n=11) complained of mild to severe pain.Spearman’s correlation research revealed a positive association between CPOT scores and the FPT score(at rest:r=0.983[Rater 1],r=0.916 [Rater 2];during the body-turning procedure: r=0.877[Rater 1],r=0.902 [Rater 2]) (P <0.01).
3.3.Internal and inter-rater reliability
Researchers assessed the pain of 52 participants,both of whom had a reduction in consciousness but were still able to convey pain.Cronbach’s α coefficient score was 0.82,which showed that the interrelatedness among the CPOT items showed high internal consistency.The results of the Kappa statistical analysis (Raters 2)indicated that the CPOT had a high degree of inter-rater reliability,especially when patients underwent the body-turning procedures(at rest,κ=0.746;during the body-turning procedure,κ=0.834;15 min after the procedure κ=0.739) (P <0.001).
4.Discussion
This research seeks to demonstrate the validity and reliability of the Indonesian version of the CPOT in measuring pain in patients with critical illness and decreased LOC.The study results indicate that the Indonesian version of the CPOT’s criteria validity is satisfactory.Spearman rank analysis demonstrates a strong positive correlation between the CPOT and the FPT instrument scores (r >0.80;P <0.01).This study’s findings are consistent with other prior validation studies,such as those conducted by Frandsen et al.[25]in Denmark,Sulla et al.[26]in Italy,Kotfis et al.[27]in Poland.The study shows that while evaluating pain in participants undergoing body-turning procedures,the verbal Numeric Rating Scale (NRS)and the CPOT have a moderate-to-strong positive correlation.NRS is a pain assessment instrument based on verbal reports or patient movements that is valid and feasible to apply to critically ill patients whose use is similar to the FPT instrument [13,14].
Participants with a GCS score between 13 and 15 were evaluated for the validity of the criteria for the Indonesian version of the CPOT,which indicates that the patient is conscious and able to articulate pain [49].The results of the validity evaluation of the Indonesian version of the CPOT are compatible with the findings ofseveral studies,which found that CPOT scores improve after bodyturning procedures,even in patients receiving analgesics [50-52].Most participants (53.8%) felt moderate pain during the bodyturning process.The group of patients who did not receive analgesics or opioid analgesics experienced a greater mean change in CPOT score.These results revealed that the analgesia obtained by the non-opioid group was satisfactory,although several of the opioid analgesic groups received bolus analgesic therapy for more than 4 h,causing the concentration of analgesic medications to approach their half-life rather than their peak time [6,51].Even when patients receive sedatives and analgesics,nursing operations might induce pain feelings up to 50 % of the time,according to several kinds of literature [52,53].
Spearman’s study also revealed that the association between the CPOT and the FPT instrument score was lower when individuals underwent body-turning procedures than at rest.As behaviorbased pain instruments capture different characteristics of pain experience than verbal pain instruments,the resulting pain scores are not necessarily comparable to verbal reports of pain intensity[13,26].et al.argue that the presence of patient pain can be known if the results of the assessment of painful pain instruments are interpreted by raters in the form of numbers or values based on the patient’s verbal report[39].
Consistency amongst assessors is crucial to ensuring the reliability of the CPOT,particularly in the context of joint efforts to communicate the results of pain assessment and evaluation of pain management.This study demonstrates the dependability of the Indonesian version of the CPOT among raters is high (κ >0.70;P <0.01),particularly when participants underwent body-turning procedures (κ=0.834).These findings demonstrate that nursing procedures that can trigger nociceptive pain raise CPOT scores when patients experience body rotation [26,49].According to the International Association for the Study of Pain (IASP),a patient’s inability to express pain does not rule out the possibility of its occurrence [40].
This study has several drawbacks.First,the study only covered a limited number of patients,especially those who needed intubation and mechanical ventilation.A larger sample size is still needed in future studies to improve the validity and reliability of the Indonesian version of the CPOT,even if the results of this study were obtained from a sufficient number of participants.Second,pain measurement based on behavioral observation requires clinical competence;therefore,the results of the CPOT for pain assessment are more accurate when performed by an assessor with specialized training in its use.Thirdly,researchers rely solely on body-turning techniques,prohibiting them from identifying other potential origins of discomfort.
5.Conclusion
The Indonesian version of the CPOT instrument is valid and reliable in detecting and assessing pain in patients with critical illness and/or decreased LOC.Clinical practice nurses in Indonesia can use the CPOT to assess pain in ICU patients.
CRediT authorship contribution statement
Luthfi Fauzy Asriyanto:Conceptualization,Methodology,Resources,Investigation,Data curation,Formal analysis,Writingoriginal draft,Visualization,and Project administration.Nur Chayati:Conceptualization,Methodology,Validation,Investigation,Data curation,Writing-review and editing,Supervision,and Funding acquisition.
Funding
This research received financial support from the Research and Innovation Institute Universitas Muhammadiyah Yogyakarta(UMY) given to Nur Chayati.
Data availability statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Declaration of competing interest
The authors declare that they have no competing interests.
Acknowledgments
Appendices.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2023.12.013.
 International Journal of Nursing Sciences2024年1期
International Journal of Nursing Sciences2024年1期
- International Journal of Nursing Sciences的其它文章
- Editorial Board of International Journal of Nursing Sciences
- Chinese Abstract
- Corrigendum to “Relationship between nurses’ perception of professional shared governance and their career motivation in Egypt:A cross-sectional study” [Int J Nurs Sci 10/4 (2023) 485-491]
- 《國際護理科學(英文)》進入中科院分區護理類2 區
- 關于翻譯量表使用授權的問答
- Summary of Guide for Authors
