Posterior scleral application of a mitomycin C-soaked sponge during trabeculectomy
Kun Hu, Yun-He Song, Feng-Bin Lin, Ying-Zhe Zhang, Ling Jin, Meng-Yin Liang,Robert N.Weinreb, Xiu-Lan Zhang
1State Key Laboratory of Ophthalmology, Zhongshan Ophthalmic Center, Sun Yat-sen University, Guangdong Provincial Key Laboratory of Ophthalmology and Visual Science, Guangdong Provincial Clinical Research Center for Ocular Diseases, Guangzhou 510060, Guangdong Province,China
2Hamilton Glaucoma Center, Shiley Eye Institute, Viterbi Family Department of Ophthalmology, UC San Diego, La Jolla, CA 92093, USA
Abstract● AlM: To evaluate the safety and efficacy of posterior scleral application (a modified technique)of an antimetabolite mitomycin C-soaked sponge in trabeculectomy for patients with glaucoma.
● KEYWORDS: glaucoma; mitomycin C; posterior scleral application; trabeculectomy; bleb morphology
INTRODUCTION
Trabeculectomy remains the mainstay of glaucoma surgery since its first introduction over 50 years ago[1].Although trabeculectomy can effectively reduce intraocular pressure (IOP), postoperative surgical failure with episcleral scarring can be problematic.The use of antifibrotic drugs,particularly mitomycin C (MMC), has greatly improved the success rate of trabeculectomy[2-3].
However, there are considerable variations regarding the method of application of MMC in trabeculectomy.Previous studies have reported the following methods of application:an irregular-shaped and oversized MMC-soaked sponge[4],transverse placement of an MMC-soaked sponge[4], MMC subconjunctival injection[5], and the use of an excessively high concentration of MMC[6].In view of the lack of cell specificity of MMC[7], these methods can lead to limited reoperation area due to excessive conjunctival injury; blebrelated complications, including bleb leakage, blebitis, and bleb perforation[8-11]; and corneal conjunctivalization.
To avoid or reduce the complications or disadvantages mentioned above, we proposed a modified technique consisting of posterior scleral application of an MMC-soaked sponge, which reduced the size of the conjunctival wound in trabeculectomy.In this technique, a sponge with a dimension of 3.5×10 mm2soaked with MMC was placed vertically and posteriorly within the sub-Tenon space and under the scleral flap[12].The current study evaluated the safety and efficacy of a modified trabeculectomy in which the MMC is applied to the sclera more posteriorly than usual.
SUBJECTS AND METHODS
Ethical ApprovalThe study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the Zhongshan Ophthalmic Center (protocol code 2021KYPJ008 and 2021/03/23 of approval).Informed consent was obtained from all subjects involved in the study.Research data are not publicly available on legal or ethical grounds.A retrospective chart review was conducted for all patients who underwent trabeculectomy performed by one surgeon(Zhang XL) at the Zhongshan Ophthalmic Center of Sun Yatsen University between January 2016 and November 2021.Diagnostic criteria for primary angle-closure glaucoma were an elevated IOP of >21 mm Hg on more than three occasions,occludable angles with peripheral anterior synechiae extending over at least 180°, the presence of optic nerve cupping greater than 0.7, and corresponding glaucomatous visual field changes[13].Primary open angle glaucoma or juvenile open angle glaucoma (JOAG) was diagnosed in the presence of a chronically elevated IOP of >21 mm Hg on more than three occasions with an open angle, optic nerve cupping greater than 0.7, and corresponding glaucomatous visual field changes[14-15].JOAG was defined as a diagnosis after the age of 4y, but before the age of 40y[15].Secondary glaucomas had a chronically elevated IOP of >21 mm Hg on more than three occasions,an associated ocular or systemic cause, and optic nerve cupping greater than 0.7, and corresponding glaucomatous visual field changes, where possible[13].The patients were consecutively enrolled in the study.The inclusion criterion was trabeculectomy using the modified MMC-soaked sponge placement method from 2016 to 2021.
The exclusion criteria were trabeculectomy using other MMC application methods, previous glaucoma surgery, any history of ocular trauma, any ocular diseases that might affect visual acuity, pregnancy or lactation, and an unwillingness or inability to provide consent.

Figure 1 Key steps in the posterior scleral application of an MMCsoaked sponge A: A 3.5 mm ×10 mm piece of MMC-soaked sponge(0.2-0.5 mg/mL) is prepared for insertion into the conjunctival bed;B: The MMC-soaked sponge is vertically and posteriorly inserted into the conjunctival bed without touching the edge of the incision or the cornea; C: The MMC-soaked sponge is shown after insertion.The sponge is placed for 1-5min to form a posteriorly-directed filtering tunnel.MMC: Mitomycin C.
Surgical ProcedureAll surgeries were performed under local or general anesthesia, depending on the patient's general health status and the estimated duration of the procedure for each case.Nineteen eyes underwent general anesthesia at the anesthesiology department, and 96 eyes were treated with local anesthesia by the surgeon.The eye was sterilized with povidone-iodine, rinsed with a balanced salt solution, and covered with a sterile drape.After a lid speculum was placed,a 7-0 silk traction suture was placed through the superior clear cornea.A conjunctival flap was performed for one clock hour in the superior quadrant at the 12 o'clock position.Blunt dissection of Tenon's capsule was performed to expose sufficient sclera posteriorly.Electrocautery was used to control episcleral bleeding.A 4 mm ×3 mm superficial (12 o'clock)scleral flap of one-half or two-thirds thickness was created.A piece of 3.5 mm ×10 mm MMC-soaked sponge (0.2-0.5 mg/mL)was made by trimming the Medical Absorbent Pad (Winner,Guangdong, China)[12].The sponge was inserted vertically and posteriorly into the sub-Tenon space (Figure 1) with the long side of the sponge placed posteriorly and superiorly towards the superior rectus but without touching the rectus.Videos of the detailed surgical techniques can be viewed using the two links provided in a prior study (https://links.lww.com/APJO/A107 and https://links.lww.com/APJO/A108)[12].After 1-5min, the sponges were removed, and the scleral bed was irrigated with 150-200 mL of balanced salt solution.
A sclerotrabecular block of tissue was excised using scissors,followed by peripheral iridectomy.The scleral flap was secured with four 10-0 nylon fixed sutures or two 10-0 nylon fixed sutures and two 10-0 nylon releasable sutures.The knots were buried, and the conjunctiva was closed with two 8-0 absorbable sutures.Releasable sutures were used if the conjunctiva and Tenon's capsule were thick or opaque.Tobramycin/dexamethasone ointment was applied at the end of the surgery.
The exact concentrations and durations of MMC were individualized.If the patient had a high risk of failure(including glaucoma associated with uveitis, congenital and developmental glaucoma, and young age ≤30y) then higher concentrations of MMC and longer exposure times were used.However, for older patients and for those with conjunctival thinning, the lowest concentrations of MMC and shortest exposure times were chosen to minimize the risk of bleb leakage and hypotony.In the present study, the maximum concentration of MMC and the longest exposure time were used in almost all JOAG patients.
Postoperative management comprised topical 1% prednisolone acetate four times per day and tobramycin/dexamethasone eye ointment at night for 1mo.Suture laser lysis, releasable suture removal, or MMC injection was performed postoperatively,according to the bleb morphology and IOP.Within one month after surgery, if the patient's IOP has a tendency to increase,the IOP will decrease following massage.After the evaluation by the ophthalmologist, laser suture lysis or releasable suture removal will be considered to adjust the IOP to an appropriate degree.MMC was administered as a subconjunctival injection(0.02 mg/mL and 0.1 mL).
Data Collection and Outcome MeasurementBaseline demographic and clinical information were collected,including medical history, ocular history, number of hypotensive medications, best-corrected visual acuity (BCVA),Goldmann applanation tonometry, gonioscopy, slit-lamp examination, fundus examination, standardized automated perimetry (Humphrey visual field analyzer, model 750; Carl Zeiss Meditec, Jena, Germany), and corneal endothelial cell density (Topcon SP-2000P; Topcon, Tokyo, Japan).Data were collected on a standardized form at the final visit.The final postoperative visit included BCVA measurements, slitlamp examination, Goldmann applanation tonometry, number of hypotensive medications, corneal endothelial cell density,slit-lamp photos of blebs (Sunkingdom LS-7DE Slitlamp,Sunkingdom, Chongqing, China), complications, and required interventions.BCVA was measured using Early Treatment Diabetic Retinopathy Study visual acuity charts and converted to visual acuity logarithm of the minimum (logMAR) for analysis.The primary outcome was the safety of trabeculectomy,including complications and bleb morphology, according to the Indiana Bleb Appearance Grading Scale (IBAGS)[16].The secondary outcome was the success of trabeculectomy.Complete success was defined as a postoperative IOP between 6 and 21 mm Hg and IOP reduction of 20% or more from baseline, with no need for IOP-lowering medication[17-18].Qualified (cumulative) success was defined as a postoperative IOP between 6 and 21 mm Hg and IOP reduction of 20%or more from baseline, with or without IOP-lowering medication[17-18].Failure was defined as IOP of >21 mm Hg with maximum medications or need for reoperation or serious complications that threatened vision.
Bleb Morphology GradingBased on slit-lamp photographs,bleb morphology was graded according to the IBAGS[16],which included bleb height (H0-H3), extent (E0-E3),vascularity (V0-V4), leakage (S0-S2), and posteriority (P0-P1).The latter was added to describe the posteriority of the bleb, which was defined as the ratio of the distance from the bleb midpoint at the limbal edge to the distal border of the bleb, compared with the distance to the superior rectus (P0,ratio <1/2; P1, ratio >1/2;Figure 2).Three masked clinicians graded the photos; if the first two graders (Song YH and Lin FB) provided different scores, a third senior ophthalmologist(Zhang XL) adjudicated.
Statistical AnalysisContinuous variables are reported as means and standard deviations or medians and interquartile ranges.Categorical variables are reported as counts (percentages).IOP values pre- and post-surgery are represented using box plots, and significance was determined using the pairedt-test.The distribution of the number of medications was illustrated by a histogram, and significance was determined using the paired Wilcoxon signed-rank test.Statistical significance was set atP-values of <0.05.All statistical analyses were performed using SPSS software (SPSS Statistics for Macintosh version 26.0; IBM, Armonk, NY,USA).
RESULTS
Baseline Characteristics and Clinical InformationA total of 115 eyes of 101 patients were included in the study.The mean age was 51.9±14.9y.The study included 63 (62.4%)males.Patients were diagnosed with primary open angle glaucoma (25, 21.7%), primary angle-closure glaucoma(54, 47.0%), JOAG (29, 25.2%), pigmentary glaucoma (1,0.9%), and others (6, 5.2%).The preoperative median BCVA(logMAR) was 0.2 (0.9), the mean IOP was 30.0±9.5 mm Hg,and the median number of anti-glaucoma medications was 3 (1).The median follow-up time was 28.0 (13.0)mo.Nineteen eyes were treated with general anesthesia and 96 eyes were treated with local anesthesia.The mean MMC concentration was 0.4±0.1 mg/mL.Concentration ≤0.3 mg/mL was used in 39 eyes and >0.3 mg/mL was used in 76 eyes.The mean MMC exposure time was 3.9±0.9min (Table 1).
Surgical OutcomesThe mean IOP decreased significantly from 30.0±9.5 mm Hg at baseline to 17.3±3.3 mm Hg at the final visit (P<0.001; Figure 3).The median number of anti-glaucoma medications decreased significantly from 3 (1) preoperatively to 0 (2) postoperatively.The number of medications used by patients is shown in Figure 4.The qualified (cumulative) success rate was 93.0% and the complete success rate was 60.0%.The failure rate was 7.0%.The success rates of general and local anesthesia were 94.7%and 92.7%, respectively.There was no significant difference between the general and local anesthesia groups (P>0.05).

Figure 2 Schematic diagram of P indicator (P0-P1) A: Ratio of the distance from the bleb midpoint at the limbal edge to the distal border of the bleb, compared with the distance to the superior rectus.P0, Ratio <1/2; P1, ratio >1/2; B: Example of P0 ratio <1/2; C:Example of P1 ratio >1/2.

Figure 3 Box plots of intraocular pressure measurements The horizontal line in the middle of each box represents the median value.The top and bottom borders of the box indicate the 75th and 25th percentiles, respectively.

Figure 4 Number of medications received preoperatively and at the final postoperative visit.
Bleb Morphologic FeaturesThe morphological distributions and features of blebs are detailed in Table 2.At the final visit,most blebs were graded as flat H0 (73, 63.5%), limited E1(100, 87.0%), moderately vascularized V3 (67, 58.3%), no leak S0 (115, 100%), and posteriorly directed P1 (96, 83.5%).The mean height, extent, and vascularity grades were 0.6±0.9,1.1±0.4, and 2.4±0.9, respectively.All scores on the Seidel test were 0.The mean posteriority was 0.8±0.4.
Complications, Postoperative Interventions, and ReoperationsThe total incidence of postoperative complications was 7.0% (Table 3).One eye developed a choroidal detachment combined with a shallow anterior chamber, and another eye developed a hyphema.A shallow anterior chamber was identified in six eyes.During the first month postoperatively,44 (38.3%) eyes underwent laser suture lysis, and releasablesutures were removed in 14 (12.2%) of the 42 eyes in which releasable sutures had been used during surgery.Five (4.4%)eyes underwentMMC injections postoperatively because of the gradual increase in IOP during the early postoperative stage, considering the tendency of bleb scarring.One (0.9%)underwent needling due to the formation of an encapsulated bleb.Three (2.6%) eyes underwentsecondary surgery (FP7 Ahmed glaucoma valve) due to high IOP.

Table 1 Baseline characteristics of patients n=115 eyes

Table 2 Distribution of bleb morphology grading scores according to the Indiana Bleb Appearance Grading Scale n=115 eyes
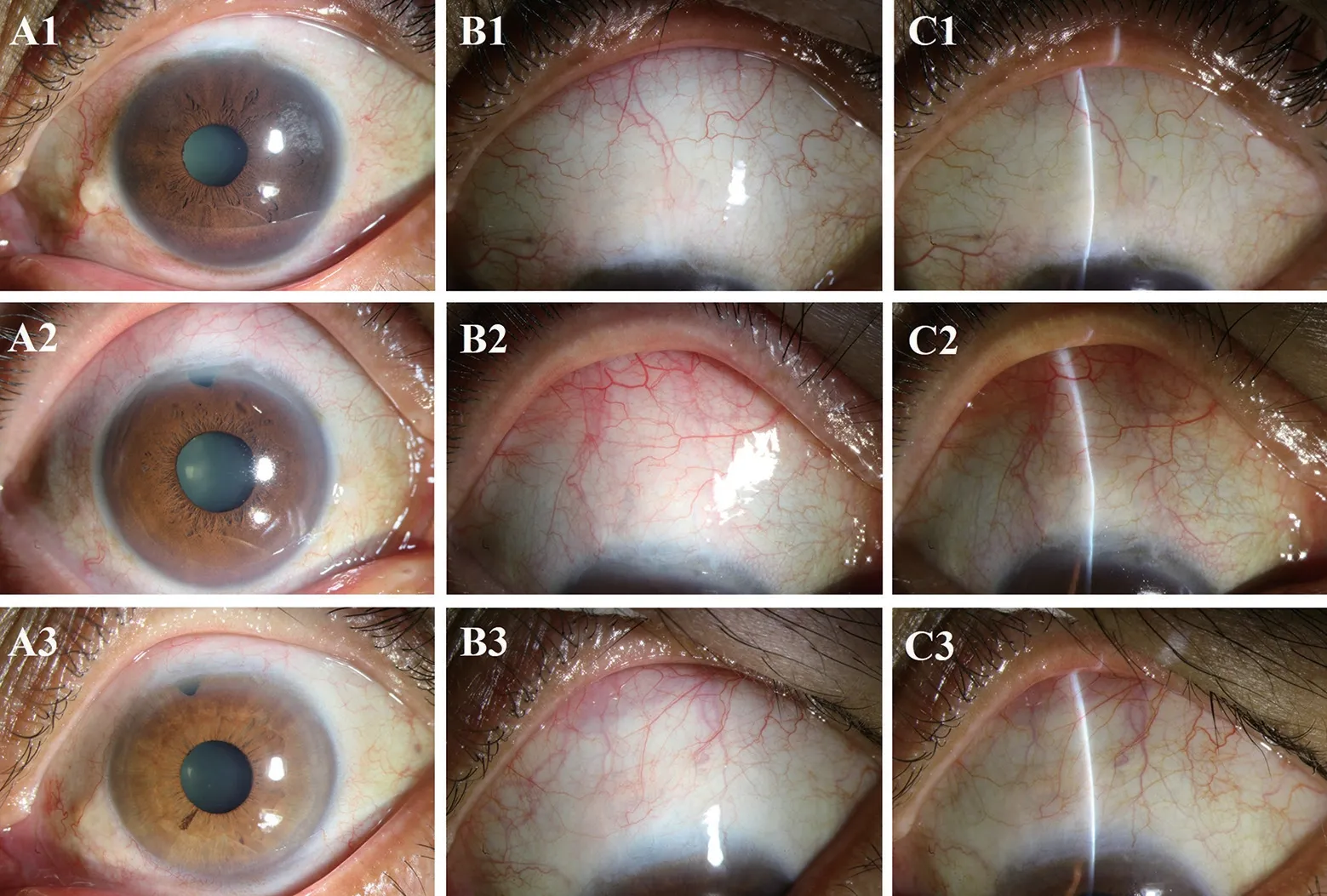
Figure 5 Bleb appearance of three typical cases using the vertical posterior MMC-soaked sponge placement method A1-A3: Diffuse illumination of the anterior segment shows bleb of horizontal extent <2 clock hours without excessive conjunctival injury, conjunctivalization, or degeneration of the cornea two years after trabeculectomy; B1-B3: Diffuse illumination of bleb shows a posteriorly directed and moderately vascularized bleb, without bleb-related complications; C1-C3: Observation under a slit lamp shows a low-lying bleb, without bleb-related complications.

Table 3 Postoperative complications and interventions n=115 eyes
DISCUSSION
Trabeculectomy with posterior scleral application of an MMCsoaked sponge was effective in reducing IOP and the number of anti-glaucoma medications at the 28-month follow-up visit.The qualified (cumulative) success rate was 93.0% and the complete success rate reached 60.0%, which is similar to or higher than those in previous studies using similar definitions of success to ours[18-23].The incidence of complications was 7%, but no bleb-related complications were observed, which is lower than previously reported[18-23].
The success rate of trabeculectomy is influenced by several factors, including the dose delivered to the tissues, volume,duration of exposure, and administration of MMC[24].It has been reported that MMC applied to a larger surface area can achieve a higher short-term decrease in IOP and a significantly lower incidence of bleb scarring compared with MMC applied to a smaller surface area; however, complications and injury to the conjunctiva were seen more often when applied to the larger surface area[25].In the current study, we delivered MMC to smaller areas than those in previous studies[18,26-27].We also placed the long side of the sponge perpendicular to the limbus,instead of parallel to preferentially enhance the posterior flow of the aqueous humor.Reducing the size of the conjunctival wound at the limbus can preserve more conjunctiva for reoperation, if required[12], particularly for patients at high risk of failure.
The bleb morphology is one of the methods for us to assess the safety and efficacy of trabeculectomy.It is closely related to surgical complications and is also a clinical indicator of the long-term success of trabeculectomy[23].The morphology of the blebs was categorized as low-lying, limited, moderately vascularized, no leak, and posteriorly directed (Figure 5);this was consistent with the ideal morphology of blebs after trabeculectomy[27-28].In addition, by adding a novel indicator,posteriority (P0-P1), based on the IBAGS[16], we found that 83.5% of blebs were posteriorly directed, thus meeting the requirements for aqueous humor drainage.
Moreover, the modified method is relatively safe.Previous studies[29-30]reported a 6% annual incidence of bleb leak and a 2% annual incidence of blebitis following trabeculectomy.However, no bleb-related complications were observed in our study.It has been reported that a cystic thin-walled bleb is often associated with an increased risk of bleb-related complications and adverse outcomes[30-31].We considered that the absence of bleb-related complications was mainly due to the low incidence (2.6%) of cystic thin-walled blebs with our modified method.In the modified method, more sclera was exposed posteriorly, and the MMC-soaked sponge covered this part of the sclera tissue; this facilitated the formation of a posteriorly directed filtering tunnel to reduce the incidence of cystic thin-walled blebs.
Although our modified method was safe and effective,postoperative complications were unavoidable.For example,one eye developed choroidal detachment combined with a shallow anterior chamber in the early postoperative period.We believe that this was mainly caused by older age and low IOP after surgery[32].After two weeks of treatment, the choroid detachment and shallow anterior chamber improved.Six eyes with a shallow anterior chamber also improved after a month.We considered several factors, including excessive filtering function and choroidal detachment[33].Further, one eye had a hyphema during the early postoperative period,due to the patient's combined hypertension[34], but it resolved spontaneously within a week without specific treatment.
Our study has several limitations.First, as we did not use a fixed concentration of MMC, it is possible that varying doses and exposure times of MMC could have impacted efficacy and safety.Further studies are required to determine the optimal concentration and exposure time for MMC.Second, this was a single-arm study with no control group for comparison.Another study comparing the standard and modified method applications of MMC is underway.
In conclusion, trabeculectomy using posterior scleral application of the antimetabolite MMC is safe and effective.This method is innovative and novel, with minimal complications and minimal injury to the conjunctiva, which provides the opportunity for reoperation if needed.
ACKNOWLEDGEMENTS
Foundations:Supported by the National Natural Science Foundation of China (No.82070955); the Science and Technology Program of Guangzhou (2022), China(No.202201020362); the High-level Hospital Construction Project, Zhongshan Ophthalmic Center, Sun Yat-sen University(No.303020104).
Conflicts of Interest: Hu K,None;Song YH,None;Lin FB,None;Zhang YZ,None;Jin L,None;Liang MY,None;Weinreb RN,None;Zhang XL,None.
 International Journal of Ophthalmology
2023年7期
International Journal of Ophthalmology
2023年7期
- International Journal of Ophthalmology的其它文章
- Chickenpox followed streaky multifocal choroiditis with prednison treatment in a girl with asthma
- Pneumonia and ocular disease as the primary presentations of Takayasu arteritis: a case report
- Unilateral blurred vision in pediatric patient associated with cavum velum interpositum cyst
- Highly cited publication performance in the ophthalmology category in the Web of Science database:a bibliometric analysis
- Comparison of efficacy of conbercept, aflibercept, and ranibizumab ophthalmic injection in the treatment of macular edema caused by retinal vein occlusion: a Metaanalysis
- Ocular manifestations and quality of life in patients after hematopoietic stem cell transplantation
