Management and evaluation of bladder paragangliomas
Dear editor,
Extraadrenal paragangliomas are tumors composed of neuroendocrine-derived, catecholamine-secreting chromaffin cells inducing hypertension, palpitations, and diaphoresis [1].Although extraadrenal paragangliomas are found in a variety of anatomic sites that normally host paraganglia-from the carotid body to the abdominal paraaortic region-the bladder is an uncommon location for paragangliomas.Bladder paragangliomas represent approximately 6% of extraadrenal paragangliomas and only 0.05%of all bladder tumors [2,3].We present a rare case of primary paraganglioma affecting the bladder dome.
A 43-year-old African-American male presented to the emergency department with rectal bleeding and abdominal pain.His medical history was significant for hypertension.Social history was significant for tobacco use.His vital signs were within normal limits.On physical examination, the abdomen was soft, non-distended, and with mild generalized tenderness.Rectal exam was negative for hemorrhoids and positive for stool guaiac.Laboratory work-up was significant for leukocytosis of 11.5 × 103/mol composed predominantly of lymphocytes and elevated creatinine of 1.25 mg/dL.Computed tomography (CT) with contrast revealed scattered sigmoid diverticula and a bladder dome mass measuring 2.8 cm × 2.6 cm × 2.5 cm with calcifications, neovascularity, and enhancement concerning for neoplasms.No adenopathy was noted on CT.Bone scan showed a 1.6 cm sclerotic bone lesion along the right ilium,several subtle sclerotic areas on the contralateral ilium,and a small radiolucent lesion within the anterior right acetabulum (Fig.1).
The patient was referred to urology for further evaluation.Cystoscopically, the mass at the bladder dome demonstrated extravesicular architecture and was suspicious for urachal tumor.Transurethral resection of bladder tumor was performed.Histopathologic examination demonstrated features of paraganglioma, including expression of the neuroendocrine markers synaptophysin and chromogranin by immunohistochemical analysis.Urine metanephrines were elevated at 506 mg/g creatinine(normal:24-96 mg/g creatinine).Positron emission tomography with acquired CT gallium-68 DOTATATE demonstrated moderate uptake in subcentimeter bilateral external iliac, pelvic, and bilateral inguinal lymph nodes.
After presentation at multidisciplinary tumor board,partial cystectomy and pelvic lymph node dissection with adjuvant chemotherapy were recommended.Preoperatively, the patient was placed on phenoxybenzamine.At the time of surgery, we placed the patient into a supine position and used a standard robotic bladder port placement.The bladder was exposed with no notable bowel adhesions.The hypervascular nodular mass at the bladder dome was readily identified and confirmed with intraoperative cystourethroscopy.The lesion was delineated with approximately 1 cm normal bladder tissue margins and excised.After cystorrhaphy, pelvic lymph nodes were dissected,and specimens were sent to pathology.There was no evidence of hypertensive crisis during the case.
Final histopathologic examination revealed a 2.4 cm bladder wall paraganglioma with extension to the perivesicular fat and peritoneal serosa.The tumor showed classic“Zellballen” architecture, consisting of cellular nests with a surrounding delicate vascular network(Figs.2A-2D),as well as lymphovascular invasion.Synaptophysin and chromogranin immunostains were positive(Figs.2E and 2F).Tumor margins were negative.One of the seven right pelvic lymph nodes excised was positive for metastatic disease(5 mm tumor deposit) with extracapsular extension.The left pelvic lymph nodes were negative(0/4).Germline testing revealed a heterozygous variant of uncertain significance in the von Hippel-Lindau (VHL) gene (c.376G>A [p.Asp126Asn]).The patient was referred to medical oncology for further evaluation and management of metastatic bladder paragangliomas.Patient was lost to follow-up 1 year from surgery.
A rare subtype, primary bladder paragangliomas often present with painless hematuria in addition to episodic catecholamine-induced symptoms such as hypertension,diaphoresis, palpitations, dizziness, headaches, and tachycardia.Micturition and bladder contraction cantrigger hypertensive or sympathomimetic crisis events in bladder paragangliomas patients.Furthermore, there are reports of precipitated attacks related to sexual arousal,defecation,ejaculation,and bladder instrumentation[1,4].

Figure 1 Abdomen and pelvis computed tomography of bladder paraganglioma.(A) Coronal image; (B) Sagittal crosssectional image.The white arrow shows the tumor.
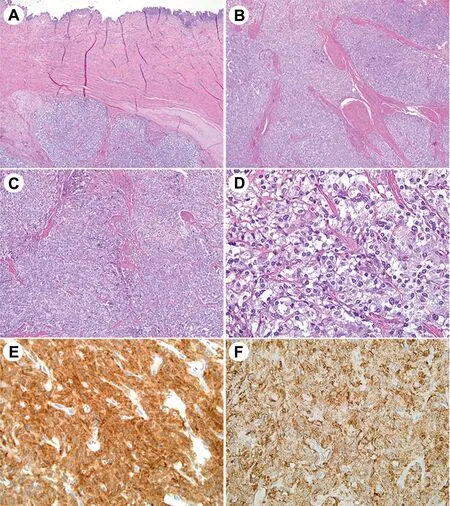
Figure 2 Histopathologic features of bladder paraganglioma.Histology images showed tumor underlying normal bladder mucosa (A, 4x original magnification) and infiltrating between detrusor muscle bundles (B, 4x).This case showed the classic zellballen or nested cellular arrangement with a surrounding delicate vascular network (C, 10x).Neoplastic cells (D, 40x)were round to polygonal and showed clear to amphophilic granular cytoplasm and strong immunoreactivity for synaptophysin (E, 40x) and chromogranin (F, 40x).
Although the majority of bladder paragangliomas are hormonally inactive,elevated levels of catecholamines have been clinically useful for biochemical profiling.Radiographically, these bladder lesions are often indistinguishable from more common bladder tumors such as urothelial carcinoma [1].Metaiodinebenzylguanidine scintigraphy with iodine-123 or -131 is useful to distinguish functional versus nonfunctional paragangliomas because these iodine analogues are utilized in the norepinephrine synthesis, a molecular pathway found in chromaffin cells.Furthermore,this imaging modality can provide information regarding tumor extension and metastatic disease with a relatively high specificity of 95%-100% [2].Histologically,paragangliomas are characterized by round to polygonal cells with granular cytoplasm arranged in a nested pattern.These tumors can often show morphologic overlap with urothelial carcinomas,granular cell tumors,neuroendocrine carcinomas, and metastatic melanoma.Therefore, careful pathologic examination, with ancillary immunohistochemical analysis for neuroendocrine markers such as neuronspecific enolase, chromogranin, and synaptophysin, and S100 (marker of the supporting sustentacular cells), are crucial to accurately diagnose bladder paragangliomas [3].
Although prognosis for benign bladder paragangliomas is excellent, about 15% of these cases are malignant, making diagnosis and treatment challenging for clinicians.Indicators for potential metastatic disease includes young age, bulky tumor, and a micturition-induced sympathomimetic attacks.Vascular invasion, invasive growth patterns,and recurrence are signs of poor prognosis [1].In patients with known metastatic disease, radical cystectomy with extensive pelvic lymphadenectomy is preferred.In contrast, in patients with localized disease, partial cystectomy with pelvic lymph node dissection is indicated.
Nearly half of paraganglioma cases are associated with hereditary conditions including VHL syndrome, Carney triad, neurofibromatosis type 1, multiple endocrine neoplasia types 2a and 2b, and familial paraganglioma.Thus, for individuals <50 years old with either a positive family history or history of bilateral, extra-adrenal, or multifocal paragangliomas,genetic testing is recommended[1].Variants in the succinate dehydrogenase subunit B(SDHB) gene and VHL have been associated with bladder paragangliomas.In a large case series of 27 patients, 17(63%) cases-14 SDHB and three VHL mutations-had germline mutations.Although SDHB mutations have been associated with higher rates of malignant behavior in pheochromocytomas, this mutation had similar rates of metastatic potential to sporadic paraganglionic tumors in the bladder, suggesting that extra-adrenal locations are independently predictive of malignancy.On the other hand, VHL mutations are uncommonly associated with malignant extraadrenal paragangliomas, with a known metastatic rate of less than 5% [5].Regardless of the underlying genetic features, bladder paragangliomas are associated with a high rate of metastatic potential compared with other disease sites; therefore, vigorous surveillance and follow-up are recommended to improve outcomes [5,6].
Author contributions
Study concept and design: Sagar Patel, Judy Hamad.
Data acquisition: Sagar Patel, Judy Hamad.
Data analysis: Sagar Patel, Judy Hamad.
Drafting of manuscript: Sagar Patel, Judy Hamad.
Critical revision of the manuscript: Mathew E.Nielson,Steven Johnson.
Conflicts of interest
The authors declare no conflict of interest.
 Asian Journal of Urology2022年1期
Asian Journal of Urology2022年1期
- Asian Journal of Urology的其它文章
- Atypical small acinar proliferation and its significance in pathological reports in modern urological times
- Subcostal artery bleeding after endoscopic combined intrarenal surgery: Signs and treatment
- Inexpensive and combined technique: Use of suction tracheal catheter and hydrogen peroxide for the evacuation of intravesical clots
- Concurrent laparoscopic management of giant adrenal myelolipoma and contralateral renal cell carcinoma
- Current insights on haemorrhagic complications in percutaneous nephrolithotomy
- Mini versus ultra-mini percutaneousnephrolithotomy in a paediatric population
