Does Liquorice Root, Hawthorn Fruit and Chinese Plum Tea Improve Quality of Life in Head and Neck Cancer Patients after Primary or Adjuvant Radiotherapy?
Ulana Kotowski Muhammad Faisal Yan Ma Inamaria Erovic Boban M. Erovic

Abstract:Objectives:Radiation induced side effects in head and neck cancers have life changing impact after treatment.We conducted a study to evaluate the effectiveness of traditional Chinese medicine tea in these patients.Methods: A randomized double-blinded pilot study was performed in head and neck cancer patients treated with radiotherapy. The study group received gargles of tea made from liquorice root, hawthorn fruit and Chinese plum. The quality of life was evaluated using the University of Washington Quality of life questionnaire Version 4 (UW-QOL).Results:The intervention group showed marginally significant outcome (p=0.075) in improved saliva production and reduced anxiety. Bitter taste was one of the major reasons for not continuing the trial.Conclusions:The proposed tea seems to provide a promising impact on the quality of life in head and neck cancer patients after adjuvant or primary radiotherapy. However, taste is a major concern and has to be adjusted to reduce patients′ dropout rate. Future trial with large samples are required to declare significant benefits.
Keywords:Head and neck neoplasms; Quality of life; Traditional Chinese medicine; Radiotherapy
1. Introduction
Head and neck cancer is the 6th leading cancer with more than 630,000 cases diagnosed annually and comprise tumours of the nasal cavity, paranasal sinuses, oral cavity, pharynx, larynx, salivary glands and thyroid [1]. Treatment options for early stage tumours include surgery or radiotherapy. However, due to nonspecific symptoms at the onset of the disease, diagnosis is often made at an advanced stage. Then multimodal therapy with surgery, radiotherapy and chemotherapy or target therapy is required. This aggressive treatment has significant side effects. Surgical as well as non-surgical treatment options lead to lifelong impairments in quality of life and have an enormous impact on physical, functional and emotional well-being of the patients [2-4]. In particular, radiotherapy, both the primary and the adjuvant form, have numerous long-term effects such as xerostomia, dysphagia, changes in taste, skin reactions, osteonecrosis of jaw, radiation induced caries and hypothyroidism [5-7]. The severity of side effects is dependent on the cumulative radiation dose applied to the head and neck region.
Quality of life encompasses the physical, psychological, and social dimensions of a person’s life. In recent times, the poor quality of life of head and neck cancer patients has come into focus. Treating cancer patients is no longer just about survival only, long-term quality of life is also taken into account [2]. Both pharmacologic and non-pharmacologic interventions are available to address the issues associated with radiotherapy. Alternative and complementary medicine applications has gained popularity due to lesser side effects associated with them [8]. Some systematic reviews have demonstrated their effectiveness in decreasing the sequelae of radiotherapy [4,9].
Traditional Chinese medicine (TCM) is a widely accepted form of alternative medicine therapy, used in Asia for thousands of years. The most common application form of TCM is Chinese herbal medicine. Patients use TCM because of its effectiveness and the lack of serious side effects [10,11]. In addition, TCM has beneficial effects in treatment of cancer [12]. Studies have shown that TCM as an adjuvant therapy for non-small cell lung cancer (NSCLC) offers an improved quality of life, is associated with less toxic side effects and improves the Karnofsky performance score [13].
The theory of TCM states that the occurrence of an illness is due to the disturbance of two opposing energy forces, namely yin and yang. In order to heal a disorder, the harmony of Ying and Yang has to be restored. Thus, TCM therapy seems to be something mysterious to many people. However, several reviews has described the use of TCM in the treatment of cancer [10,14,15]. Furthermore, several TCM herbs contain phytochemicals such as resveratrol, curcumin and quercetin. These substances have been studied in detail for years and show many anticancer effects such as antiproliferative, pro-apoptotic and anti-metastatic effects [11].
So far there are few studies on the effectiveness of TCM treatment in patients with head and neck cancer. Therefore, we have performed this randomized double-blinded study to investigate the impact of a TCM-based preparation made of liquorice root, hawthorn fruit and Chinese plum, on patient’s symptoms after radiotherapy. The aim was to reduce the side effects caused by conventional cancer treatment and to provide an improved quality of life.
2. Methods
Thirty eight patients (both male and female) were enrolled in this prospective double blinded randomized study. The sample size was calculated based on a two sided t-test at a significance level of 0.05 with 80% power of study. The number was sufficient to detect an effect size of one standard deviation. The study was conducted in accordance with the guidelines of the Declaration of Helsinki (1964) including current revisions. Ethical approval was granted by the Ethics Committee, Medical University of Vienna. All the patients have given the informed consent for enrolment in the trial. The patients were assigned to intervention (n=19) and placebo (n=19) groups by block randomization in 1:1 setting using online randomization software (Randomizer; Institute for Medical Informatics, Statistics and Documentation, Medical University of Graz, Austria; available at http://www.randomizer.at/. We have used the University of Washington Quality of Life Questionnaire, Version 4 (Head and neck disease specific tool) which is well validated, simple, brief and explanatory in providing sufficient clinical information. The self-administrative mode was adapted to avoid potential interviewer bias. The intervention group was given a prescription of Gan Cao (Glycyrrhizae uralensis, liquorice root) 160g, Shan Zha (Crataegus pinnatifida, hawthorn fruit) 80g and Wu Mei (Prunus mume, Chinese plum) 160g to be used as a tea two times a day for a period of 3 months, the control group used placebo (Gan Cao 100g). The participants were instructed to hold 2g of the tea for a few seconds in the oral cavity, followed by gargling and drinking the tea.
The measurable variables are presented by mean± standard deviation with a confidence interval of 95% for the means of both groups. Primary endpoint was the change of University of Washington-Quality of life (UOW-QOL) score at 3 months from the baseline in both placebo and treatment groups.
Data was analysed using SPSS software (IBM SPSS Statistics for Windows, Version 22.0 ; IBM Corp., Armonk, NY, USA). Descriptive statistics (frequency with percentage (%) mean and standard deviation (M±SD) and median and interquartile ranges (IQR) were presented for participants’ age, gender, site, stage and tumour radiation doses. Missing data was excluded from the diagnosis. The comparison among the control and intervention group at baseline and 3 months was performed using paired sample t-test. The scores were calculated from the UOW-QOL questionnaire as mean ± SD. The outcome was measures in p-value which was considered significant if < 0.05.
3. Results
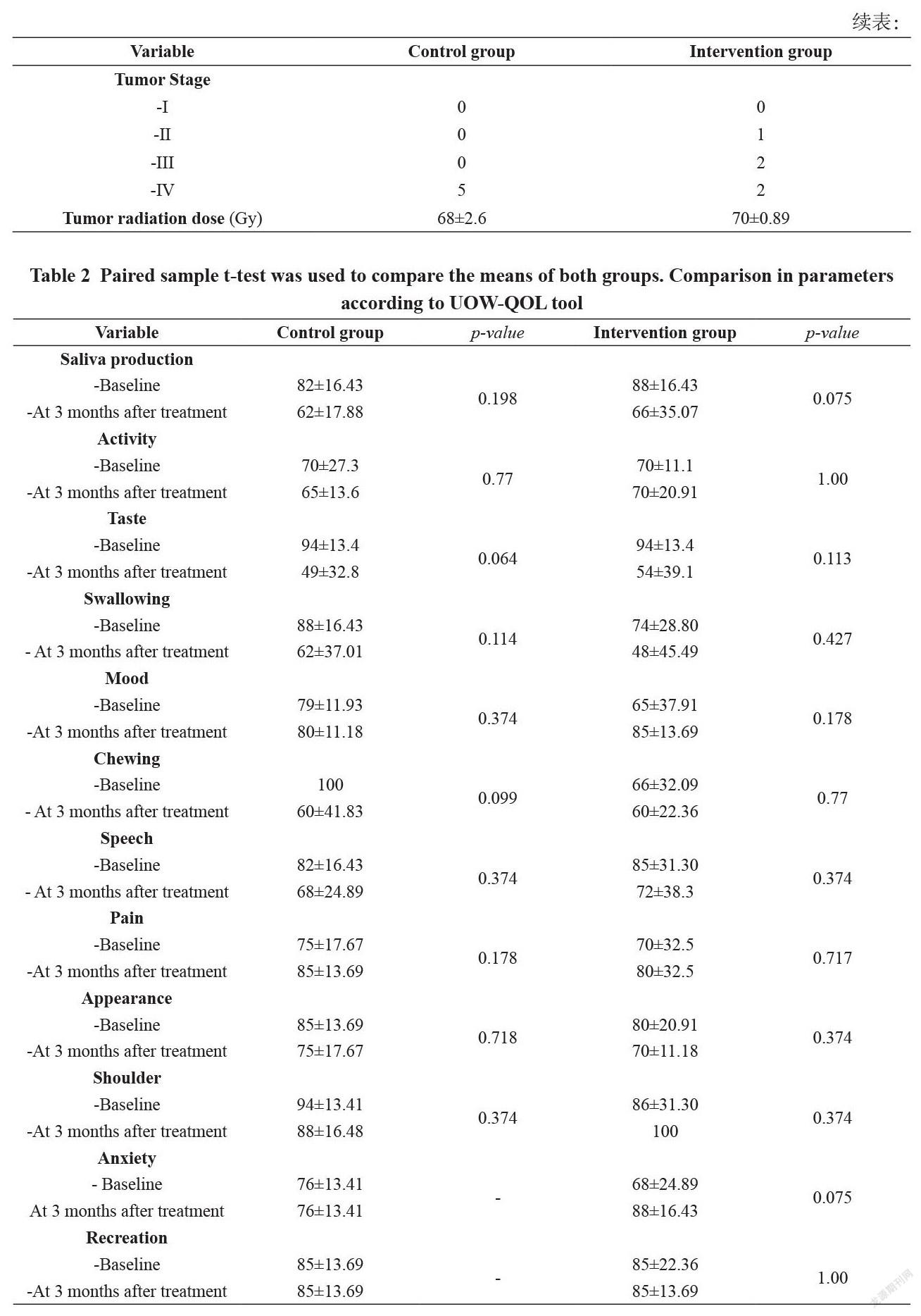
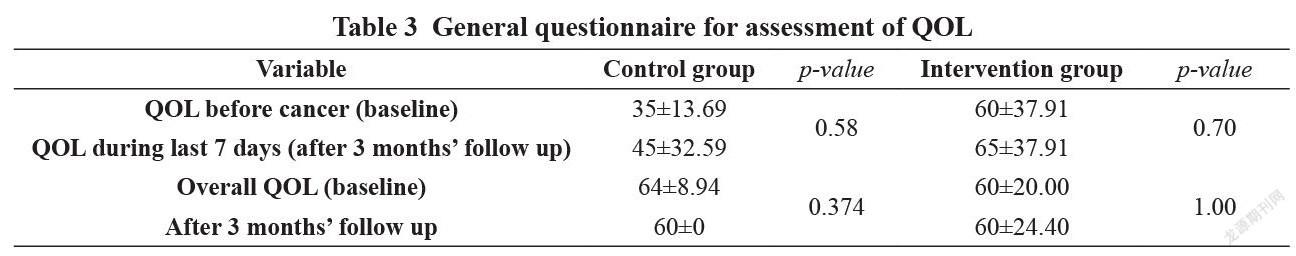
We have enrolled 38 participants in this study who were treated with radiotherapy (either in primary or adjuvant form) for squamous cell carcinoma of head and neck. However, only 10 patients (5 in control and intervention group each) were evaluated while others were excluded due to multiple reasons which include lost to follow up (9), unwillingness to participate later due to issues related to taste (9), cost (1), nausea (1), viscous saliva (1), irregular drinking (3) and ineffective response (4). The participants included 7 males and 3 females with a mean age of 59±18.4 in control group and 61±11.3 in intervention group. The sites involved were larynx (3), oropharynx (3), hypopharynx (1), tongue base (2) and parotid (1). Most of the patients were stage IV (70%) followed by stage III (20%) and stage II (10%). The intervention group received a mean dose of 70 Gray (Gy) while the control group was given 68 Gy. Further baseline characteristics are shown in Table 1. Statistics have depicted marginally better outcomes only in saliva production (p = 0.075 vs. 0.198) and anxiety level of QOL score in intervention group as compared to placebo (Table 2 and 3).
4. Discussion
Head and neck cancer leaves a lasting impression on the patients in terms of social, physical and psychological outcomes [16]. Most of the head and neck cancer patients have to undergo radiotherapy and the complications like mucositis and xerostomia lead to a significant deterioration in quality of life. The University of Washington Head and Neck Quality of Life questionnaire is a reasonably validated tool for assessment in its revised form (Version 4) by Weymuller et al. Contrary to pharmacological medicine, traditional or folk medicine is an alternative yet not a reliable form of treatment in certain spectrum [17].
Liquorice (derived from the plant root) is a flavouring and sweetening agent and also an important component of traditional Chinese medicine with antiviral, antibacterial, anti-cancer, anti-inflammatory and hepatoprotective properties [18,19]. Pre-operative use of topical liquorice has resulted in reduced sore throat in a systematic review while additional studies have reported reduced xerostomia in haemodialysis patients [20]. Another study in head and neck cancer patients showed that aqueous extract of liquorice can decrease the severity of oral mucositis post radiotherapy [21].
Hawthorn fruit, another derivative from a plant, is used in traditional Chinese medicine to improve digestion, cardiovascular function and hyperlipidaemia [22]. Additionally it has gastroprotective, antimicrobial and anti-inflammatory functions [23]. Hawthorn contains a wide variety of phytochemicals, of which polyphenols are a class of the most important and effective components. A study in breast cancer cells showed that extracts from hawthorn fruit have an antiproliferative effect and lead to apoptosis [24].
Prunus mume (Chinese plum) originates from the south of China and has been introduced in several Asian countries. In traditional medicine, it is used for a variety of symptoms such as headache, fatigue, cough, food poisoning, constipation and stomach disorders. Prunus mume extracts show anti-inflammatory, antioxidant as well as anti-cancer properties [25]. In particular, extracts of Prunus mume lead to inhibition of cell proliferation in lymphoma, lung cancer, pancreatic cancer, colon cancer, breast cancer and oesophageal cancer cell lines [25]. Studies on mouse models have shown that Prunus mume extract attenuates the epithelial destruction and mucosal infiltration of inflammatory cells in colitis [26]. In addition, intake of Chinese plum has a preventive effect on chronic atrophic gastritis by inhibiting H. pylori infection and reducing mucosal inflammation [27].
Our study has included both male and female participants. All the patients presented with head and neck cancer were above 50 years of age at the time of diagnosis. It is a known finding that salivary flow decreases with increasing age [28]. In addition to that, radiation treatment as part of the protocol usually causes an irreversible xerostomia with doses exceeding 60 Gy. The radiation dose given to head and neck cancer patients stays within the range of 50-70 Gy for most of the cases. In our series, the intervention group has received a mean dose of 70 Gy which is slightly more than the control (68 Gy). When it comes to feedback by the participants, the intervention group has shown slightly better outcome in terms of xerostomia (p = 0.075 vs 0.198) even though this group has received more dose of radiation in comparison to control. The UOW-QOL questionnaire score has remained above 60 in both groups which depicts less but enough saliva production.
An interesting finding is the reduction in anxiety levels in the intervention group although not statistically significant. The participants have reached the mean score above 80 in UOW-QOL questionnaire which means a little anxiety about having a cancer.
As far as the rest of the parameters are concerned, we did not find any significant difference between the two groups.
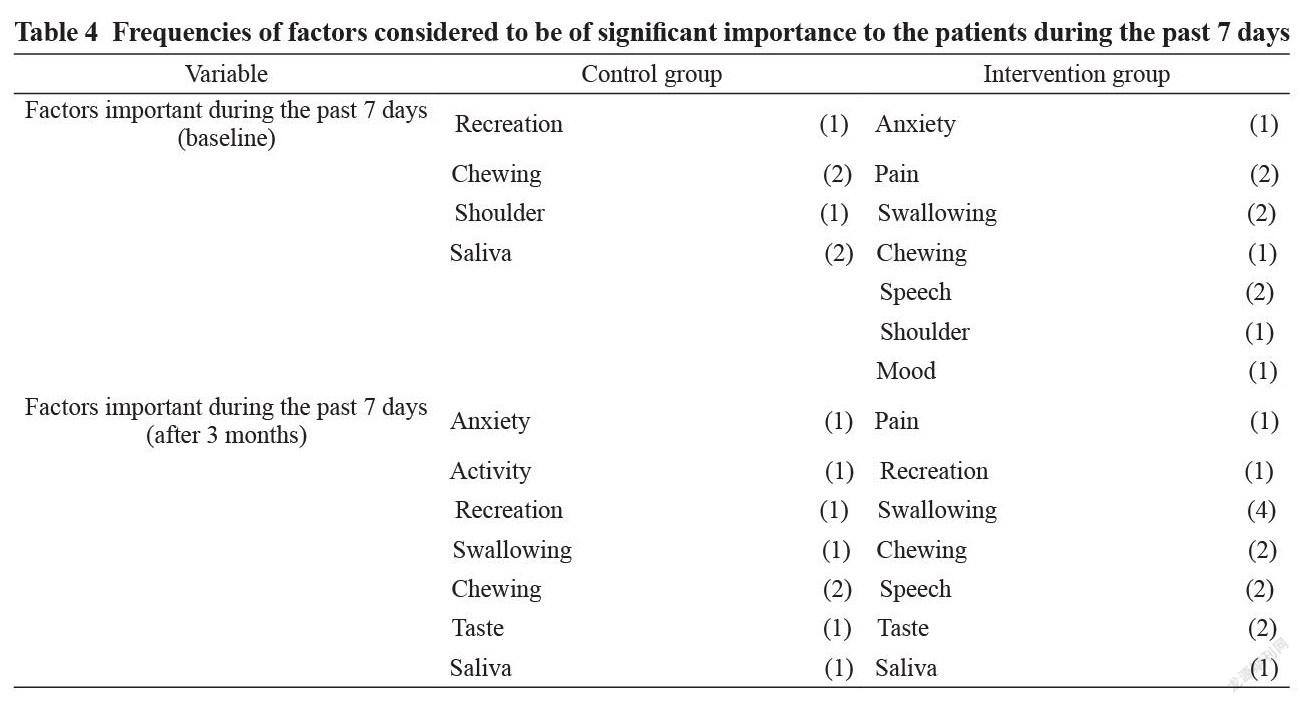
Comparing the most important factors concerning patients in the last 7 days at baseline and after 3 months follow up, our results have demonstrated the results in Table 4. In control group, the most critical factors relevant to the patients were saliva and chewing. The patients having chewing problems were the ones treated for oropharyngeal and base of tongue tumours. On the other hand, the intervention group has depicted swallowing, speech and pain as the integral factors concerning patients.
A significant number of patients have left the trial in the middle due to many factors. The prominent reasons identified were bad taste, no subjective feeling of improvement and failure to follow the protocol of drinking the tea as per protocol given to them. Bad taste has usually been attributed to the presence of TAS2R receptors which perceive bitterness at the dorsum of the tongue [29].
Our study has several limitations. Although a reasonable sample size was selected at the beginning of the trial but many patients have left it for understandable reasons. Due to small sample size, the outcomes may have not represented the significant statistics. Patients undergoing surgery followed by adjuvant radiotherapy may have profound effects in the post treatment period as compared to ones receiving radiotherapy as the primary and only treatment modality.
Conclusion
The use of alternative, non-pharmacologic or traditional Chinese medicine in alleviating the short and long term side effects of radiation therapy has been on the rise. More prospective, randomized large population based trials in future are required to declare if these medicines have any potential benefit or not.
Declarations
Funding
This study was funded by the Medical University of Vienna.
Conflicts of Interest
All authors declared that there are no conflicts of interest.
Ethical Approval
Ethical approval was granted by the Ethics Committee, Medical University of Vienna.
Consent to Participate
Not applicable
References
[1]. Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55:74–108.
[2]. Swift AC. Principles and Practice of Head and Neck Oncology. 2003.
[3]. Jones E, Lund VJ, Howard DJ, Greenberg MP, McCarthy M. Quality of life of patients treated surgically for head and neck cancer. J Laryngol Otol. 1992;106:238–42.
[4]. Rogers SN, Hannah L, Lowe D, Magennis P. Quality of life 5-10 years after primary surgery for oral and oro-pharyngeal cancer. J Craniomaxillofac Surg. 1999;27:187–91.
[5]. Chan ATC, Grégoire V, Lefebvre J-L, Licitra L, Hui EP, Leung SF, et al. Nasopharyngeal cancer: EHNS-ESMO-ESTRO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2012. pp. vii83–5.
[6]. Grégoire V, Lefebvre J-L, Licitra L, Felip E, EHNS–ESMO–ESTRO Guidelines Working Group. Squamous cell carcinoma of the head and neck: EHNS-ESMO-ESTRO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2010. pp. v184–6.
[7]. Pinna R, Campus G, Cumbo E, Mura I, Milia E. Xerostomia induced by radiotherapy: an overview of the physiopathology, clinical evidence, and management of the oral damage. Ther Clin Risk Manag. Dove Press; 2015;11:171–88.
[8]. Molassiotis A, Ozden G, Platin N, Scott JA, Pud D, Fernandez-Ortega P, et al. Complementary and alternative medicine use in patients with head and neck cancers in Europe. Eur J Cancer Care (Engl). John Wiley & Sons, Ltd; 2006;15:19–24.
[9]. Laverick S, Lowe D, Brown JS, Vaughan ED, Rogers SN. The impact of neck dissection on health-related quality of life. Arch. Otolaryngol. Head Neck Surg. American Medical Association; 2004;130:149–54.
[10]. Xiang Y, Guo Z, Zhu P, Chen J, Huang Y. Traditional Chinese medicine as a cancer treatment: Modern perspectives of ancient but advanced science. Cancer Med. John Wiley & Sons, Ltd; 2019;8:1958–75.
[11]. Liu T-G, Xiong S-Q, Yan Y, Zhu H, Yi C. Use of chinese herb medicine in cancer patients: a survey in southwestern china. Evid Based Complement Alternat Med. Hindawi; 2012;2012:769042.
[12]. Lin H-C, Lin C-L, Huang W-Y, Shangkuan W-C, Kang B-H, Chu Y-H, et al. The use of adjunctive traditional Chinese medicine therapy and survival outcome in patients with head and neck cancer: a nationwide population-based cohort study. QJM. 2015;108:959–65.
[13]. Chen S, Flower A, Ritchie A, Liu J, Molassiotis A, Yu H, et al. Oral Chinese herbal medicine (CHM) as an adjuvant treatment during chemotherapy for non-small cell lung cancer: A systematic review. Lung Cancer. 2010;68:137–45.
[14]. Nie J, Zhao C, Deng LI, Chen J, Yu B, Wu X, et al. Efficacy of traditional Chinese medicine in treating cancer. Biomed Rep. Spandidos Publications; 2016;4:3–14.
[15]. Carmady B, Smith CA. Use of Chinese medicine by cancer patients: a review of surveys. Chin Med. BioMed Central; 2011;6:22–8.
[16]. Kazi R, De Cordova J, Kanagalingam J, Venkitaraman R, Nutting CM, Clarke P, et al. Quality of life following total laryngectomy: assessment using the UW-QOL scale. ORL J. Otorhinolaryngol. Relat. Spec. 2007;69:100–6.
[17]. Weymuller EA, Alsarraf R, Yueh B, Deleyiannis FW, Coltrera MD. Analysis of the performance characteristics of the University of Washington Quality of Life instrument and its modification (UW-QOL-R). Arch. Otolaryngol. Head Neck Surg. American Medical Association; 2001;127:489–93.
[18]. Gupta VK, Fatima A, Faridi U, Negi AS, Shanker K, Kumar JK, et al. Antimicrobial potential of Glycyrrhiza glabra roots. J Ethnopharmacol. 2008;116:377–80.
[19]. Jo E-H, Hong H-D, Ahn N-C, Jung J-W, Yang S-R, Park J-S, et al. Modulations of the Bcl-2/Bax family were involved in the chemopreventive effects of licorice root (Glycyrrhiza uralensis Fisch) in MCF-7 human breast cancer cell. J. Agric. Food Chem. 2004;52:1715–9.
[20]. Kuriyama A, Maeda H. Topical application of licorice for prevention of postoperative sore throat in adults: A systematic review and meta-analysis. J Clin Anesth. 2019;54:25–32.
[21]. Najafi S, Koujan SE, Manifar S, Kharazifard MJ, Kidi S, Hajheidary S. Preventive Effect of Glycyrrhiza Glabra Extract on Oral Mucositis in Patients Under Head and Neck Radiotherapy: A Randomized Clinical Trial. J Dent (Tehran). Tehran University of Medical Sciences; 2017;14:267–74.
[22]. Chu S-M, Shih W-T, Yang Y-H, Chen P-C, Chu Y-H. Use of traditional Chinese medicine in patients with hyperlipidemia: A population-based study in Taiwan. J Ethnopharmacol. 2015;168:129–35.
[23]. Tadi? VM, Dobri? S, Markovi? GM, Dordevi? SM, Arsi? IA, Menkovi? NR, et al. Anti-inflammatory, gastroprotective, free-radical-scavenging, and antimicrobial activities of hawthorn berries ethanol extract. J. Agric. Food Chem. 2008;56:7700–9.
[24]. Li T, Zhu J, Guo L, Shi X, Liu Y, Yang X. Differential effects of polyphenols-enriched extracts from hawthorn fruit peels and fleshes on cell cycle and apoptosis in human MCF-7 breast carcinoma cells. Food Chem. 2013;141:1008–18.
[25]. Bailly C. Anticancer properties of Prunus mume extracts (Chinese plum, Japanese apricot). J Ethnopharmacol. Elsevier; 2020;246:112215.
[26]. Jin H-L, Lee B-R, Lim K-J, Debnath T, Shin H-M, Lim B-O. Anti-Inflammatory Effects of Prunus mume Mixture in Colitis Induced by Dextran Sodium Sulfate. Korean Journal of Medicinal Crop Science. The Korean Society of Medicinal Crop Science; 2011;19:16–23.
[27]. Enomoto S, Yanaoka K, Utsunomiya H, Niwa T, Inada K, Deguchi H, et al. Inhibitory effects of Japanese apricot (Prunus mume Siebold et Zucc.; Ume) on Helicobacter pylori-related chronic gastritis. Eur J Clin Nutr. Nature Publishing Group; 2010;64:714–9.
[28]. Ying Joanna ND, Thomson WM. Dry mouth - An overview. Singapore Dent J. 2015;36:12–7.
[29]. Chandrashekar J, Mueller KL, Hoon MA, Adler E, Feng L, Guo W, et al. T2Rs function as bitter taste receptors. Cell. 2000;100:703–11.

