Mid-term results of patterned laser trabeculoplasty for uncontrolled ocular hypertension and primary open angle glaucoma
Gustavo Espinoza, Yuly Andrea Castellanos-Castellanos, Angelica Pedraza-Concha,3,Ignacio Rodrguez-Una, Maria Fernanda Acua, Juan Camilo Parra
1Centro Oftalmológico Virgilio Galvis, Bucaramanga,Santander 681004, Colombia
2Fundación Oftalmológica de Santander, Bucaramanga,Santander 681004, Colombia
3Universidad Industrial de Santander, Bucaramanga, Santander 680002, Colombia
4Instituto Oftalmológico Fernández-Vega, Universidad de Oviedo, Oviedo 33012, Spain
Abstract
INTRODUCTION
Glaucoma represents a main public health problem and the foremost cause of irretrievable blindness in the world. This disease produces progressive injury to the optic nerve, resulting in visual loss[1]. Prevalence of primary open angle glaucoma (POAG) is about 2% in people over 40 years of age[2]. The disease degenerates retinal ganglion cells, leading to changes in the optic nerve head and progressive loss of visual field[1].
Αt the time, the only modifiable and most important risk factor for developing POAG is an elevated intraocular pressure(IOP). Though, not every patient with high IOP is categorized as glaucoma, therefore a patient with elevated IOP and no signs of POAG on standard clinical tests is categorized into an ocular hypertension (OHT) diagnosis[3]. In this group of patients, decreasing IOP reduces the risk of developing POAG[4].
Medical treatment is predominantly used as first‐line therapy to lower IOP in patients with POAG and OHT. Long-term therapy induces several adverse events such as inflammation of the conjunctiva with a consequent lower success rate for any filtration surgery[5-6].
The laser therapy was introduced by Wise and Witter[7]in 1979 using argon laser trabeculoplasty (ALT), demonstrating that IOP decreased when changes in the structure of the trabecular meshwork occurred and the aqueous humour flow was facilitated. However, it was found that it could cause damage and scarring of the trabecular meshwork. Subsequently, in 1995, selective laser trabeculoplasty (SLT) was introduced,generating less damage and inflammation by targeting pigmented cells of the trabecular meshwork[8].
Subthreshold pattern scanning laser (Pascal Streamline 577,Topcon Inc., Tokyo, Japan) was first described in 2006 to perform panretinal photocoagulation in a grid pattern with shorter pulses (10-20ms) generating less pain, less thermal damage of the tissue and achieving the complete treatment in a smaller number of sessions[9]. In recent studies, patterned laser trabeculoplasty (PLT) has also been described for open angle glaucoma (OAG) and OHT management. Results demonstrated both short and long term efficacy and safety of PLT comparable to ALT and SLT[10-16]. However, to date,no study has evaluated PLT IOP-lowering effect after 12mo follow-up in a non-Caucasian population. Therefore, the objective of this study was to describe the efficacy and safety of PLT as an adjunctive treatment in POAG and OHT after 18-month follow-up in Hispanic population.
SUBJECTS AND METHODS
Ethical ApprovalThis was a retrospective analysis of clinical data drawn from records of patients with POAG and OHT undergoing PLT from June 2016 to August 2016 at Fundación Oftalmólogica de Santander (FOSCAL; Santander, Colombia)with the aim of evaluating 18mo of follow-up. All procedures were in accordance with ethical standards of the Institutional Research Committee and with the Declaration of Helsinki.The study was conducted under a waiver of informed consent following review of the Research Ethics Committee of FOSCAL.
Patients with age ≥18y with POΑG or OHT and uncontrolled by medical therapy were included. Eyes were excluded if there was presence of advanced glaucoma, history of glaucoma surgery (prior laser peripheral iridotomy was allowed) and treatment with systemic or topical corticosteroids.
After the procedure, follow-up visits were scheduled at 1wk,1, 3, 6, 12, and 18mo. Data collected at baseline were age,sex, best-corrected visual acuity (BCVA) in logMAR, IOP measured with Goldmann applanation tonometer, gonioscopy and number of glaucoma medications. Data collected at each follow-up visit were IOP, adverse events, BCVA, and number of IOP-lowering medications.
Αll eyes received a single session of 360° laser treatment with the PASCAL laser (Pascal Streamline 577, Topcon Inc., Tokyo,Japan). The full details of the laser procedure were describedelsewhere[13]. Postoperatively, patients were treated with topical steroids for a week. The adjustment of glaucoma medications was based on the IOP at each follow-up visit at the discretion of the surgeon.
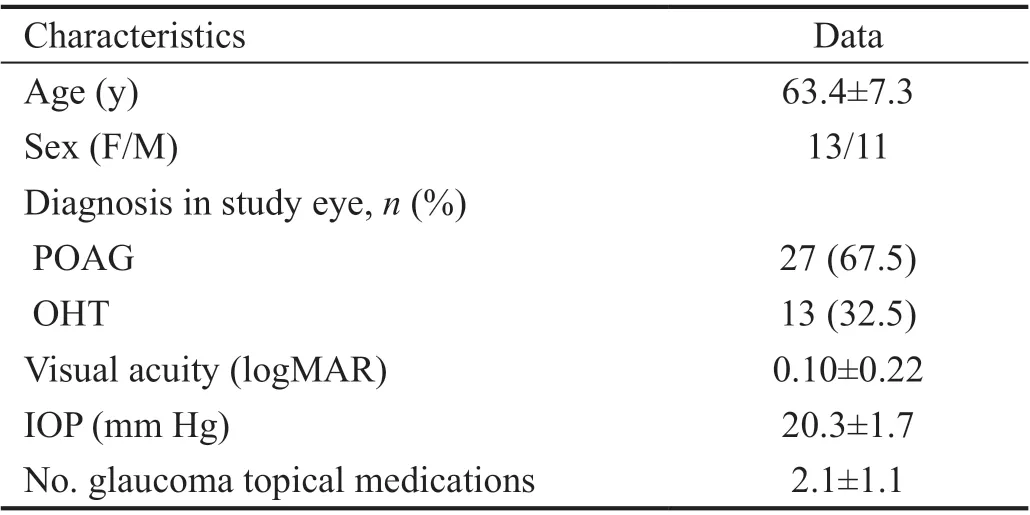
Table 1 Demographics and baseline clinical characteristics mean±SD
Statistical AnalysisAll statistical analysis was performed using Stata software 13.0 (Stata Corp LLC, TX, USA). The mean IOP measured before laser treatmentwas compared at each follow-up visit respectively at 1wk, 1, 3, 6, 12, and 18mo. The proportional IOP reduction from baseline was assessed. The normal distribution of the data was evaluated by the Shapiro-Wilk test. Quantitative data were described as mean±standard deviation (SD) for most of the parameters.Qualitative data were presented as frequencies and proportions.Absolute IOP and proportional IOP reduction from baseline(IOP reduction rate) as well as the differences in the number of glaucoma medications were statistically analyzed using Student’st-test for normally distributed data. Statistical significance was set atP<0.05. The data were also graphically presented by box plots to show the IOP trends at each post-PLT visit. Primary efficacy outcome measures were the proportion of eyes achieving an IOP reduction ≥20% at 18mo versus baseline medicated IOP; or a reduction in the number of medications while maintaining IOP values. Other secondary outcome measures included mean IOP change from baseline to each follow-up visit and reduction in the number of glaucoma medications. The safety of the procedure was assessed using descriptive analysis of adverse events.
RESULTS
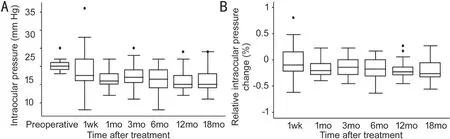
Figure 1 IOP follow-up throughout the first 18mo A: Average absolute IOP over time; B: Average relative changes in the IOP over time. Boxplots display the median as center line, 25th and 75th percentiles as a box, 5th and 95th percentiles as whiskers.

Table 2 Mean intraocular pressure and topical medications at each time point mean±SD
PLT was successfully performed in 40 eyes of 24 patients with diagnosis of POAG and OHT (54.2% were women) with a mean age of 63.4±7.3y. Most subjects were on treatment with prostaglandin analogues (75%), β‐blockers (60%) or carbonic anhydrase inhibitors (60%), and a smaller number of cases used an alpha 2-adrenergic agonists (17.5%). Baseline preoperative characteristics are illustrated in Table 1. After 18mo, the initial sample of 40 eyes was reduced to 34 eyes due to difficulty in monitoring.PLT was performed in 360° of the trabecular meshwork of all the patients in a single session with an exposure time of 5ms and mean power of 670±77.2 mW. The average number of shots applied on the trabecular meshwork were 1048.4±207.6.Success rate after 18-month follow-up was 61.7%. IOP reduction was statistically significant from the first month. Mean IOP and IOP-lowering medication data are given in Table 2. The mean IOP reduction from baseline across visits (months 1, 3,6, 9, 12 and 18) ranged from 14.1% to 20.8% (Figure 1). Mean medicated IOP at baseline was 20.3±1.7 mm Hg and 16±3.2 mm Hg at 18mo (P<0.001), with a mean IOP reduction of 20%.The decrease in medications was not statistically significant compared to the last follow-up, changing from 2.1±1.1 to 2.3±1.1 (P=0.86). Eight eyes (23.5%) suspended at least one topical medication and of those, two eyes (5.8%) suspended all the topical medication at the end of the follow-up period.Six eyes (17.6%) require additional topical medications to control their IOP. No patient required additional surgery for the management of glaucoma.
Visual acuity remained stable, from an initial BCVA of 0.10±0.22 logMAR to a final BCVA at 18mo of 0.11±0.22 logMAR (P=0.42).
Postoperative adverse events through the 18mo were mild,without major repercussions on the evolution of the patients.Among the complications, four eyes (10%) presented IOP spikes after the procedure that were controlled with topical medication (brimonidine 0.20%). Seven eyes (17.5%)developed peripheral anterior synechiae (PAS), no greater than 90o in extension.
DISCUSSION
This study demonstrates that efficacy of PLT as an adjuvant treatment might be sustained after 6-month follow up. Mean IOP after PLT was clinically and statistically significantly reduced from the first month (P<0.001). Nevertheless, no decrease in the number of IOP-lowering medications was achieved.
In our first report on the results of PLT after 6‐month follow‐up we found an IOP reduction of 18.3% (P<0.001), with a success rate of 48.78%[13]similar to previous reports from Turatiet al[10]and Mansouriet al[11](67% and 37%, respectively). However,for this study we considered the reduction of medications while maintaining IOP as a criterion for success. This increased PLT success at 6mo by 50%. Al Zubi and Alsalem[14]evaluated the efficacy of PLT after 6mo of follow‐up with 180° laser treatment. They evaluated each eye separately finding an average IOP reduction from the pre-treatment level of 22.1 to 18.8 mm Hg in the right eyes (representing an average IOP reduction of 14.9%) and from 22.7 to 19.2 mm Hg in the left eyes (representing an IOP reduction of 15.4%). Recently, Elahiet al[15]compared long term safety and efficacy of PLT and SLT in a Caucasian population using the same criteria of our study for success definition. Their results were comparable to our findings, with a success rate of 60.5% after 24-month follow-up in the PLT group, suggesting that IOP reduction may remain stable for more than 6mo. Furthermore, a randomized clinical trial conducted by Wonget al[16]compared the IOP decreasing effect of PLT and SLT after 12-month follow-up.Complete success (without glaucoma topical medications) and partial success (with or without glaucoma topical medications)was 15.4% and 35.4%, respectively, in the PLT group. These rates were lower to our findings.
In 1979, ALT was first introduced for the management of glaucoma patients[11,17-18]. ALT increases the outflow of aqueous humor by means of photocoagulation in the trabecular meshwork, thus reducing the IOP[11]. Nevertheless, ALT had various adverse events, most frequently elevated IOP and uveitis. Coagulation of the trabecular meshwork was also described, resulting in PAS[19]. Tuulonen[20]evaluated safety and efficacy of ALT after 18mo of follow-up in 54 patients.The mean IOP reduction of all eyes was 28% in POAG and 37% in pseudoexfoliative glaucoma. This IOP reduction was a greater of the results we found with PLT. Five out of 63 eyes showed transient IOP spikes, and one patient developed minor PAS.
In 1998 SLT was introduced by Latinaet al[21]. This therapy induces biological changes that increase aqueous outflow across the trabecular meshwork (including cytokine secretion, changes in gene expression, induction of matrix metalloproteinases and remodeling of the trabecular meshwork)[21-22]. It has been described that SLT achieves an IOP reduction ≥20% in 66.7%-75% at 6mo, 58%-94% at 12mo, 40%-85% at 2y of follow-up, 38%-74% at 3y and 11.1%-31% at 5y of followup[23-24]. Αlthough there is substantial difference in the reported IOP-lowering ability of SLT, our results with PLT are in agreement with the general reported results on the majority of eyes regarding IOP reduction with SLT. Other authors compared SLT to PLT, showing no statistical differences regarding safety and efficacy in the short and long term follow‐up[11,15-16]. The effect of IOP reduction with SLT decreases over time and an average survival time of about 2y has been described. Notably, we did not find a reduction in IOP lowering effect after 18mo of follow-up with PLT. Although SLT is considered less traumatic than ALT, complications can still occur, including IOP spikes (increase of ≥5 mm Hg in up to 28% of eyes), transient inflammation and PAS (2.86% of cases, with a higher incidence after a second SLT session)[23-24].Recently, the Laser in Glaucoma and Ocular Hypertension trial(LiGHT) compared initial SLT with initial topical medication for treatment na?ve patients with POAG or OHT. In this randomized controlled trial conducted in 718 patients, 356 patients were treated with SLT and 362 patients with topical medical management. At 24mo of follow-up, 79.2% of patients in the SLT group did not need topical hypotensive management to maintain the target IOP. None of the patients in the laser trabeculoplasty group required filtering surgery compared to 11 patients in the medical management group[25-26]. These findings are in agreement with our study on the fact that none of our patients needed additional surgery. Nevertheless, our study considered topical medical escalation as a treatment for IOP control compared to LiGHT trial, where repeat SLT was also considered.
In the present study no significant decrease in the number of antiglaucoma topical medications was found. However, the number of medications did not increase either. In a randomized clinical trial conducted by De Keyseret al[27]on 143 medically controlled glaucoma patients, patients were randomized to receive either SLT or to a control group that continued on IOP lowering medications. Full replacement of medications by SLT was achieved in 43 eyes (74.1%) after 18mo. These results support the fact that SLT can replace medication. Still,it is impossible to compare this group of patients with ours since they were medically controlled. Real-world outcomes of SLT in the United Kingdom found a noteworthy increase of 0.13 from baseline in the mean number of IOP-lowering medications received per year after 12 to 18mo of follow-up.They reported that the number of patients receiving one or more glaucoma medication increased from 268 (61%) before SLT, to 285 (64.9%) at 12 to 18mo after SLT[28]. Shibataet al[29]evaluated efficacy of SLT as adjunctive therapy in OΑG patients with 180° and 360° treatment. The number of medications before laser were 3.0 for the 180° group and 2.8 for the 360° group. The average follow‐up was 19.5mo for 180° group and 17.9mo for 360° group. Success rates were superior in the 360° groups at 1 and 2y after SLT than in the 180° group (46% and 29%vs25% and 22%, respectively).Results of the 360° group are in accordance with our results at least for the 12-month follow-up control. Nevertheless, even though medical escalation and additional glaucoma surgery were considered as failure, they did not report mean number of medications after the procedure or patients requiring surgery.There are new laser trabeculoplasty modalities in clinical practice, comprising micropulse laser trabeculoplasty (MLT)and titanium-sapphire laser trabeculoplasty (TSLT). Several studies reported a 20% and 24% IOP reduction with MLT at 1 and 2y of follow-up respectively[18], with minimal ocular pain during laser, minimal ocular inflammation after the procedure and without reported complications (including PAS and IOP spikes). Regarding the TSLT, an IOP reduction of 32% at 15mo of follow-up has been reported. IOP spikes were the only complication reported at 2y of follow-up[18]. In our study IOP spikes were observed in 9.8% of cases, and PAS in 17.1%. None of the patients developed PAS greater than 2 clock hours or 90° in extension. Αs mentioned before in our previous report, we believe that the learning curve with the device, borderline open angles and location of the titration area with total power delivered to it might be considered as risk factors for developing PAS[13]. Wonget al[30]noted as published in their Meta-analysis, that only 2.86% of cases with SLT treatment developed PAS with increased occurrence after repeated SLT. This can also be considered as a risk factor.However, none of our patients repeat PLT. Limitations from the present study are the retrospective design and the small sample size. Also, the indications and decision of prescribing additional medications or indicating surgery after PLT was made by the treating physician based on the overall status of each patient. Furthermore, visual fields report after PLT were not considered in the last follow-up data, which could have been interesting for the analysis. In conclusion, results suggest that 360° PLT is a safe and effective procedure in patients with medically uncontrolled POAG and OHT. Although the results appear to be promising, long-term may provide further knowledge regarding this technique.
ACKNOWLEDGEMENTS
Authors’ contributions:Study concept and design (Espinoza G, Castellanos-Castellanos YA, Parra JC); data collection(Espinoza G); analysis and interpretation of data (Espinoza G, Castellanos-Castellanos YA, Rodriguez-Una I); drafting of the manuscript (Espinoza G, Pedraza-Concha A, Acu?a MF);critical revision of the manuscript (Espinoza G, Castellanos-Castellanos YA, Rodriguez-Una I, Parra JC); supervision(Espinoza G, Castellanos-Castellanos YA, Rodriguez-Una I,Parra JC).
Conflicts of Interest:Espinoza G,None;Castellanos-Castellanos YA,None;Pedraza-Concha A,None;Rodriguez-Una I,None;Acu?a MF,None;Parra JC,None.
 International Journal of Ophthalmology2021年8期
International Journal of Ophthalmology2021年8期
- International Journal of Ophthalmology的其它文章
- Macular density alterations in myopic choroidal neovascularization and the effect of anti-VEGF on it
- Combined ab-interno trabeculectomy and cataract surgery induces comparable intraocular pressure reduction in supine and sitting positions
- Comparison of the SlTA Faster–a new visual field strategy with SlTA Fast strategy
- Evaluating newer generation intraocular lens calculation formulas in manual versus femtosecond laser-assisted cataract surgery
- Conjunctival flap with auricular cartilage grafting: a modified Hughes procedure for large full thickness upper and lower eyelid defect reconstruction
- Improvement of human embryonic stem cell-derived retinal pigment epithelium cell adhesion, maturation, and function through coating with truncated recombinant human vitronectin
