Hemorrhagic transformation of ischemic cerebral proliferative angiopathy: A case report
Yu Xia, Xian-Feng Yu, Zhen-Juan Ma, Zhong-Wu Sun
Yu Xia, Xian-Feng Yu, Zhen-Juan Ma, Zhong-Wu Sun, Department of Neurology, The First Affiliated Hospital of Anhui Medical University, Hefei 230022, Anhui Province, China
Abstract BACKGROUND Cerebral proliferative angiopathy (CPA) is a rare vascular disease characterized by the presence of diffuse vascular proliferation, progressive vascular hyperflow and vasodilation of multiple vessels in the normal brain parenchyma. Unlike cerebral arteriovenous malformations, CPA has a mixed appearance between that of lesions with cell proliferation and endothelial proliferation. To date, the pathogenesis of CPA is unclear, in which changes induced by cortical ischemia in the elastic layer of the blood supply artery and smooth muscle cells may be involved.CASE SUMMARY In this article, we retrospectively analyzed a case of hemorrhagic transformation of ischemic CPA diagnosed by digital subtraction angiography and reviewed the related literature for further exploration of its pathogenesis, diagnosis and treatment.CONCLUSION The information in the present case report may facilitate further clinical research on this cerebrovascular disease.
Key Words: Hemorrhagic transformation; Cerebral proliferative angiopathy; Pathogenesis;Diagnosis; Treatment; Case report
INTRODUCTION
Cerebral proliferative angiopathy (CPA) is defined as an atypically chronic ischemic cerebrovascular disease that appears to be significantly different from normal arteriovenous malformation (AVM) in epidemiology, clinical manifestations, angiographic and histopathological features, natural history and management[1]. In CPA, a large and sparse lesion caused by progressive angiogenesis can be seen in the normal brain parenchyma. Ischemia induced by hypoperfusion around the lesion is considered to lead to that excessive proliferation[2]. CPA is less common than AVM, and hemorrhagic transformation of ischemic CPA is much rarer.
CASE PRESENTATION
Chief complaints
Our patient was a 76-year-old male with dizziness, headache and left hemiparesis and numbness.
History of present illness
The patient was diagnosed with hemorrhagic cerebral infarction and was treated with mannitol and glycerol fructose to reduce intracranial pressure.
History of past illness
The patient had a history of hypertension, and no oral medications were applied.
Personal and family history
The patient smoked for decades and presently quit smoking. In addition, he occasionally drank alcohol. No family hereditary diseases and tumors were reported.
Physical examination
At the time of admission, the main clinical positive signs of this patient were as follows: positive horizontal nystagmus; both eyes were blurred to the left; the left limb muscle strength was grade IV; the left limbs’ shallow sensations were decreasing; and the left pathological sign was positive.
Laboratory examinations
Cerebrospinal fluid routine, biochemistry and serum paraneoplastic neurological syndrome test results were negative. Additionally, there were no significant abnormalities in blood examinations.
Imaging examinations
A magnetic resonance imaging (MRI) scan was performed, which revealed a massive cerebral infarction in the right temporal lobe, parietal lobe, occipital lobe and the corpus callosum accompanied by minor bleeding and gliosis within. In addition, brain enhanced MRI showed irregular ring enhancement in the right temporo-occipital junction area and corpus callosum compression, and the posterior horn of the right lateral ventricle was compressed (Figure 1). Brain computed tomography angiography revealed intracranial artery stenosis and hyperplasia (Figure 2).
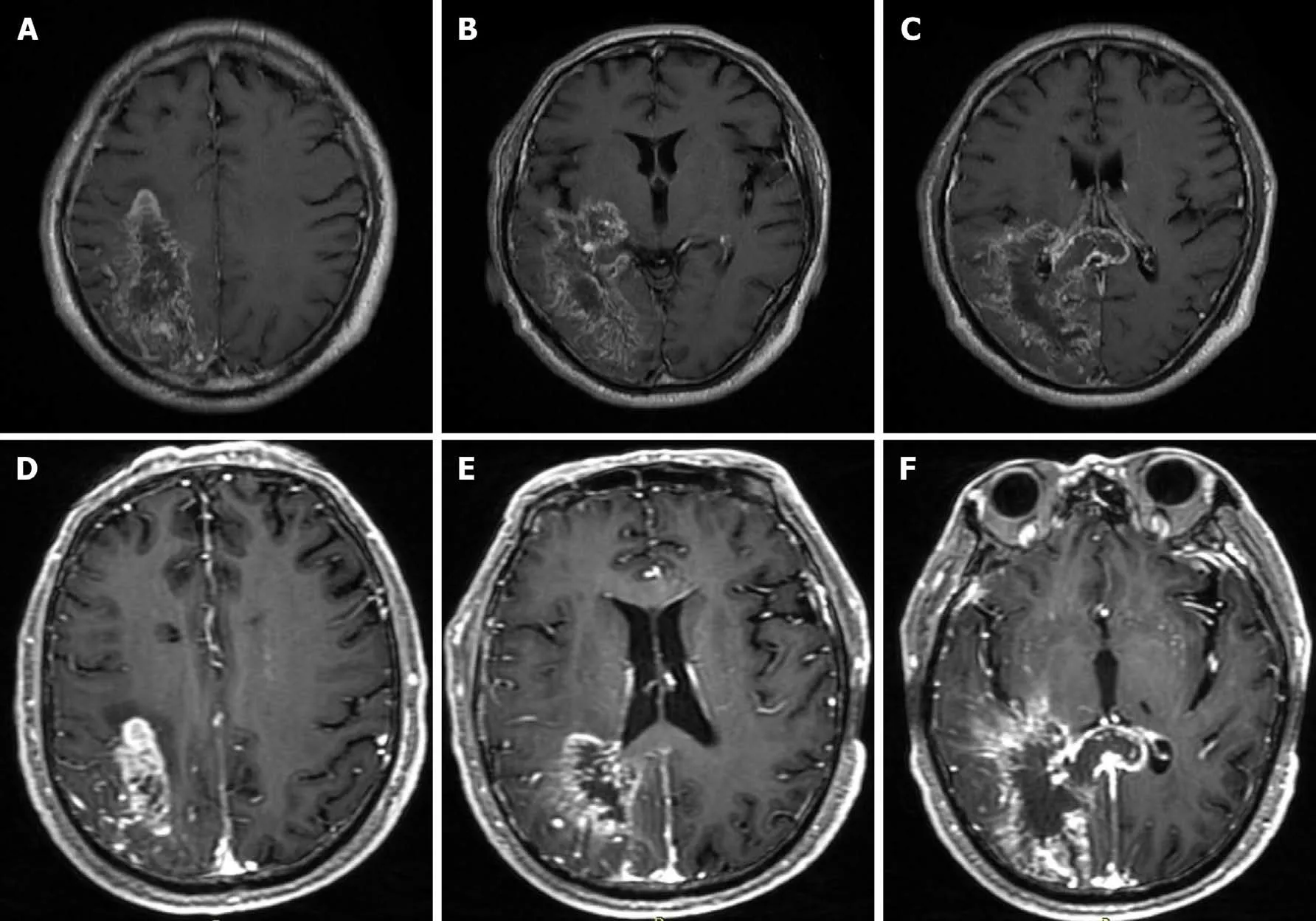
Figure 1 Brain magnetic resonance imaging. T1-weighted images showed different locations of a massive cerebral infarction accompanied by minor bleeding and gliosis. A: The right parietal lobe; B: The right temporal lobe and the occipital lobe; C: The right temporal lobe, the occipital lobe and the corpus callosum.Enhanced T1-weighted images showed irregular ring enhancement; D: The right parietal lobe; E: the right temporal lobe and the occipital lobe; F: The right temporal lobe, the occipital lobe and the corpus callosum.
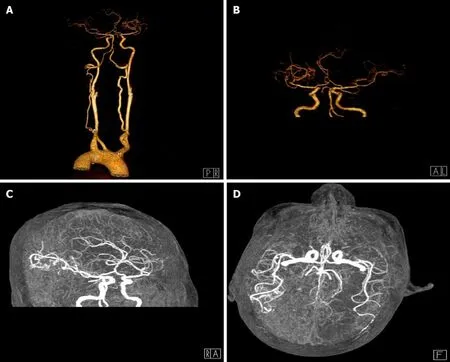
Figure 2 Brain computed tomography angiography. Computed tomography angiography showed different locations of artery stenosis and hyperplasia. A:Mild stenosis in the internal carotid arteries on both sides at the beginning; B: The right middle cerebral artery with hyperplasia; C: The thickness of the anterior cerebral arteries on both sides was uneven; D: The posterior cerebral artery on the right was slender.
Chest and abdominal pelvic computed tomography and brain magnetic resonance venography. Digital subtraction angiography showed a large number of proliferative blood vessels in the blood supply area of the right middle cerebral artery. A small number of proliferative blood vessels were also seen in the A4 segment of the right anterior cerebral artery. A large number of proliferative blood vessels were visible in the P3 or P4 segment of the posterior artery (Figure 3).
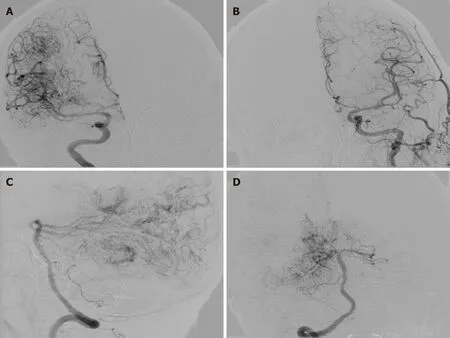
Figure 3 Brain digital subtraction angiography. Anteroposterior view of a right internal carotid artery (ICA) angiogram. A: Anteroposterior view of a left ICA angiogram; B: Lateral view of a right posterior cerebral artery (PCA) angiogram; C: Anteroposterior view of a right PCA angiogram; D: Diffuse vascular malformation can be seen in the right cerebral hemisphere.
FINAL DIAGNOSIS
Hemorrhagic CPA after ischemia
TREATMENT
In this case, symptomatic treatments such as lowering intracranial pressure and fluid supplementation were the main treatments. Considering that the risk of surgical treatment was too high, the family refused.
OUTCOME AND FOLLOW-UP
At his 1-year telephone follow-up, we learned that the aforementioned clinical symptoms had been progressively worsening with a disturbance of consciousness, and the patient had eventually passed away.
DISCUSSION
Recently, Lasjauniaset al[1] retrospectively analyzed 1434 AVM databases, where they identified CPA in 49 cases with an age range of 10-65 years, with the highest proportion in young women.In addition,Puertaet al[3]reported an 8-year-old child suffering from CPA. However, our patient was a 76-year-old male. Other investigations[4-6] showed that CPA accounted for approximately 2%-4% of all AVMs,indicating that the right cerebral hemisphere was the most common location,especially the temporal lobe. CPA usually manifested as epilepsy, headache and progressive neurological deficit (predominantly ischemia). Our patient had lesions in the right temporal, parietal and occipital lobes. The most important finding was that in the case described here, the patient had postischemic hemorrhagic transformation. To date, this transformation phenomenon has not been largely reported in the literature,and thus we collected and summarized the information available on all cases of hemorrhagic CPA to establish its clinical features[7-13] (Table 1).
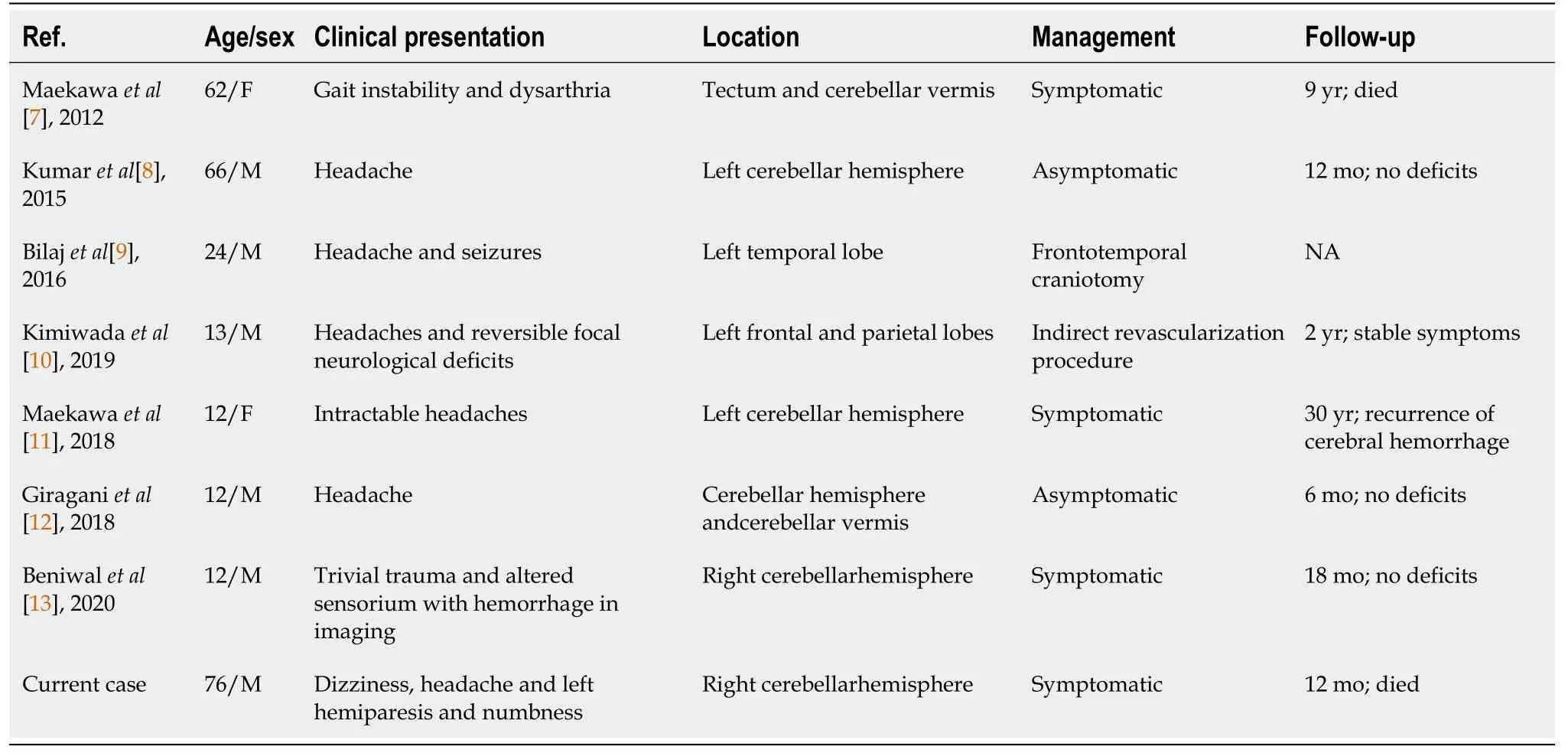
Table 1 Review of all hemorrhagic cerebral proliferative angiopathy published to date
CPA was diagnosed by its typical vascular imaging features. The major manifestation of CPA on MRI was diffuse lesions with a densely enhanced vascular network structure mixed with normal brain parenchyma. In some CPA patients, the drainage veins were reduced, with varying degrees of vein thickening on MRI. On digital subtraction angiography, the blood vessels were in a muddy shape with a scattered distribution, manifested in a small shunt volume, lack of dominant arterial blood supply period, delayed arterial phase and early venous phase. The patient had a large number of proliferative blood vessels in the blood supply area of the right middle cerebral artery. Proliferated blood vessels were also visible in the A4 segment of the right anterior cerebral artery. No obvious abnormalities were detected in the left middle cerebral artery and the anterior cerebral artery. The vertebral artery angiography showed extensive hyperplasia in the P3 or P4 segment of the right posterior cerebral artery. The draining veins were clearly visible, and no abnormality was found in the left posterior cerebral.
CPA may be cured surgically by embolization and using stereotactic radiotherapy,which could increase the blood flow to the hypoperfused brain tissue and prevent future ischemia[14,15]. Considering that the aforementioned treatment methods are risky with poor long-term prognosis, conservative treatment is still the mainstay[16].In our case, the most characteristic feature of CPA that distinguished it from cerebral AVMs was the presence of recognizable neurons and normal brain tissue intertwined with abnormal blood vessels[17].The vascular lesions of CPA were unstable,and their continuous growth was detected by neuroimaging at multiple time points. The lesions gradually expanded, accompanied by aggravated clinical symptoms, which indicated that CPA was progressive. After the patient was discharged from the hospital on September 3, 2019, his dysfunction of the limbs worsened again. However, due to the unstable vital signs of the patient, his digital subtraction angiography images were not reviewed. Larger clinical trials are required for a further exploration of the pathogenesis of this disease aimed at the discovery of new therapeutic options.
CONCLUSION
CPA is a rare ischemic vascular disease, and hemorrhagic transformation after ischemia has been seldom reported. In recent years, increased research attention has been paid to this disease. The pathogenesis, clinical manifestations, diagnosis and treatment of CPA have been initially established. However, in the future, more highquality clinical research is to be conducted to further explore its pathogenesis, improve therapeutic schedules for minimizing its disability and reduce mortality.
 World Journal of Clinical Cases2021年20期
World Journal of Clinical Cases2021年20期
- World Journal of Clinical Cases的其它文章
- Corrigendum to “Probiotic mixture VSL#3: An overview of basic and clinical studies in chronic diseases”
- Role of gastrointestinal system on transmission and pathogenesis of SARS-CoV-2
- COVID-19: Considerations about immune suppression and biologicals at the time of SARS-CoV-2 pandemic
- Histopathology and immunophenotyping of late onset cutaneous manifestations of COVID-19 in elderly patients: Three case reports
- Multidisciplinary team therapy for left giant adrenocortical carcinoma: A case report
- Splenosis masquerading as gastric stromal tumor: A case report
