Impaired eye tracking is associated with symptom severity but not dynamic postural control in adolescents following concussion
Jessie R.Oldham*,William P.Meehan IIIc,David R.Howell
a The Micheli Center for Sports Injury Prevention,Waltham,MA 02453,USA
b Division of Sports Medicine,Department of Orthopedics,Boston Children’s Hospital,Boston,MA 02115,USA
c Department of Pediatrics and Orthopedics,Harvard Medical School,Boston,MA 02115,USA
d Sports Medicine Center,Children’s Hospital Colorado,Aurora,CO 80045,USA
e Department of Orthopedics,University of Colorado School of Medicine,Aurora,CO 80045,USA
Abstract
Keywords: Gait;Mild traumatic brain injury;Vision
1. Introduction
Concussions are complex injuries that result in a disruption of normal brain functioning.1Approximately one-half of the brain’s circuits are involved with visual pathways, so effects of concussion on the visual system are routinely observed.2,3Post-concussion vision disorders are commonly seen in adolescents cared for in specialty clinics,with up to 51%demonstrating either accommodative disorders,convergence insufficiency, or saccadic dysfunction, and 46% presenting with multiple diagnoses.4,5Symptom resolution remains one of the main indicators of concussion recovery, and visual symptoms have been associated with persistent concussion symptoms.6,7However, physiological impairments may linger beyond symptom resolution,8and it is unknown how visual symptoms may be associated with other clinical concussion symptoms.Furthermore, while total symptom scores are frequently used in concussion evaluations, the individual symptom domains can provide important clinical information,9,10and it is unknown how the individual symptom profiles may influence eye tracking visual performance.
Traditionally,concussion evaluations require a multifaceted approach,consisting of symptom,neurocognitive,and postural control assessments.1Horizontal saccades tests have been used in concussion evaluations and have been associated with other functional abilities,such as concentration,visual motor speed,and reaction time, suggesting that vision assessments should be included in the multifaceted battery.11Additionally,using a combination of saccadic eye movements, smooth pursuits,convergence,vestibular ocular reflex,and visual motion sensitivity, the Vestibular/Ocular Motor Screening assessment has successfully differentiated between concussion and control groups with high sensitivity.12This has allowed clinicians to provide more targeted treatment following injury since the Vestibular/Ocular Motor Screening evaluates distinct ocular and vestibular symptoms.12
Although not as established in the concussion literature,eye tracking is another visual function that has recently demonstrated efficiency in assessing both concussion and central nervous system impairments by identifying abnormalities in oculomotor neural pathways.13-15Furthermore, emerging technology has allowed for the objective evaluation of eye tracking movements in a portable, clinical environment. Due to algorithms developed to interpret ocular abnormalities,these eye tracking measures have correctly distinguished between individuals with a concussion and healthy controls and have successfully identified vision abnormalities following concussion, even in the absence of pre-concussion eye tracking data.13,16Using a metric of pupillary disconjugacy,researchers have previously identified concussion-related visual impairment in a pediatric concussion population,14,17but the relationship between this approach and other concussion measures warrants further study.
儀器設(shè)備:過(guò)濾器,島津GC2010 PLUS氣相色譜儀,安捷倫氣相色譜-質(zhì)譜聯(lián)用儀(GC-MS,5975C+7890A,EI源),北京普析通用TU-1901型紫外分光光度計(jì)。
Vision is a critical component of postural control, and it is imperative for the stabilization of upright posture because it allows individuals to detect their motion relative to other structures in their visual field.18,19Eye movements appear to play a large role in this process and have shown to affect posture during quiet standing.18,20,21Visual feedback is also important for dynamic tasks of postural control, such as locomotion, and information from the visual system is necessary for locomotor control regulation.18,22-24Individuals with visual impairments who are otherwise healthy have appeared to adopt a more cautious gait strategy,similar to that seen following concussion.22However, less is known about how vision and gait are related following concussion, particularly in a population with eye tracking impairments.
Gait speed is a clinically feasible measure that reflects an individual’s functional capacity and physiological changes,25and a conservative gait strategy, evidenced largely by slower gait speed, has been observed repeatedly following concussion.26,27Additionally, previous work has reported a significantly slower single-task and dual-task gait speed in a group of adolescent athletes who presented with receded near point of convergence following concussion relative to uninjured controls, suggesting that vision deficits may be related to motor dysfunction.5It is unknown whether motor dysfunction also exists in a post-concussion adolescent population with abnormal eye tracking abilities.However,both vergence and pursuit eye movements have anatomical pathways rooted in the cerebellum,2which also largely controls the feedforward control required during gait.28Thus, it is possible that those with impaired eye tracking also demonstrate deficits in dynamic postural control.
The purpose of our investigation was to (1) examine the relationship between self-reported symptoms and concussion related eye tracking impairments,and(2) compare single-task and dual-task gait speed between (a) adolescents with a concussion who have normal eye tracking, (b) adolescents with a concussion who have abnormal visual tracking abilities, and(c) healthy controls. We hypothesized that those adolescents with a concussion and abnormal eye tracking would have higher symptoms on the Post-Concussion Symptom Scale(PCSS) and slower single-task and dual-task gait speed compared to those with a concussion and normal eye tracking and healthy controls.
2. Methods
2.1. Study design and participants
We conducted a cross-sectional study to evaluate eye tracking, symptoms, and gait performance in both concussed individuals and healthy controls. Concussion participants were patients who presented to a sport concussion clinic within a tertiary care regional children’s hospital. Following injury,patients self-presented or were referred from an emergency department or their regular healthcare provider. They were diagnosed and evaluated by a sports medicine physician in accordance with the most recent International Consensus on Concussion in Sport definition.1Similar to previous work,17,29healthy controls were individuals reporting to the injury prevention center for personal training sessions or injury prevention evaluations, or were the children of hospital employees.We included participants who were between the ages of 8 and 18 years and agreed to participate within the first 10 days of injury (concussion group). We excluded participants who had a current lower extremity orthopedic injury that may have affected normal gait, participants with sensory deficits (deafness or blindness),and participants with diagnosed psychiatric disorders. Institutional review board approval was obtained from the Boston Children’s Hospital’s Ethical Committee prior to the start of the study, and all participants provided written informed assent or consent(if ≥18 years old)to participate before enrollment. Consent was obtained from the parents/guardians if the participant was younger than 18 years old.
2.2. Eye tracking protocol
During the eye tracking trials, participants watched a brief(220 s) video that moved around the screen while their eye movements were recorded. An Eyelink 1000 eye tracker (SR Research Ltd.,Mississauga,Ontario,Canada)recorded continuous eye movements at a fixed distance of 55 cm between the computer monitor and the participants’ eyes, and eye position data were recorded at 500 Hz. The video occupied approximately one-ninth of the computer screen and moved clockwise around the outer edges of the computer monitor as it played.During the procedure, participants sat in a height-fixed chair and placed their chin on a chin rest fixed on a height-adjustable table. This procedure has been described previously in detail and has successfully identified post-concussion vision problems,as well as demonstrated an acceptable level of test-retest reliability in healthy adolescents.13,16,17,29All eye tracking was binocular, and no spatial calibration was performed to allow for the independent analysis of both pupils for the duration of the trial.
2.3. Gait protocol
Gait speed was measured using 3 triaxial accelerometers(Opal Sensors,APDM Inc.,Portland,OR,USA)placed on the dorsal surfaces of each foot and around the L5 vertebra of the spine. The accelerometers have been demonstrated to be reliable when compared to force plates and to be valid for use in both neurological and healthy populations.30-32Participants were instructed to walk, at a self-selected pace, down a 10-m walkway, turn around at a specified end point, and return to the starting line. All participants completed 5 trials of singletask gait(i.e.,walking without any other task completion)and 5 trials of dual-task gait. During the dual-task condition, individuals simultaneously answered cognitive questions while walking. As with prior work,33,34the cognitive tasks were mini-mental-style questions that consisted of either spelling 5-letter words backwards, counting backwards by 6 s or 7 s from a specified number,or reciting the months of the year in reverse order. The order of the cognitive tasks was randomized.Participants were not given any practice trials or prioritization instructions on the motor task or the cognitive task.
2.4. Clinical symptoms
To evaluate concussion symptoms, we used the PCSS,which is a standard form that records the presence and severity of 22 concussion symptoms at the time of testing.35The PCSS is part of the 5th version of the Sport Concussion Assessment Tool36and requires participants to rate their concussion symptoms from 0 to 6, where 0 equates to “no symptom” and 6 equates to“severe symptoms”.In addition to total PCSS score,we also evaluated the individual symptom profiles, as previously published.10The profile breakdown was somatic (headache, pressure in the head, neck pain, nausea or vomiting,sensitivity to light, and sensitivity to noise), vestibular-ocular(blurred vision, balance problems, and dizziness), cognitive(don’t feel right, confusion, feeling like in a “fog”, difficulty concentrating, and difficulty remembering), emotional (more emotional than usual,irritable,sadness,and nervous/anxious),and sleep(feeling slowed down,drowsiness,fatigue,and trouble falling asleep).
2.5. Outcome variables and statistical analysis
From the eye tracking protocol,our outcome variable was the BOX score, which is a metric of pupillary disconjugacy that has been reliably used for diagnostic purposes in a pediatric concussion population.13,14,17We classified the concussion group into those with a normal BOX score of <10 and those with an abnormal BOX score of ≥10,based on existing standards.13Our outcome variables from the gait protocol were single-task and dual-task gait speed, and our symptom variable was the total score from the PCSS.The average gait speed across the 5 trials was measured by the accelerometers and calculated within Mobility Lab as the average stride velocity for left and right feet across all gait cycles in each trial.37,38
Demographic variables are presented as mean ± SD and were compared using one-way analyses of variance, with the exception of sex,which was compared using a x2-analysis of variance test. Normality was determined using a Shapiro-Wilk test. Total PCSS scores, PCSS symptom profiles, and BOX scores were also compared using one-way analyses of variance. We conducted linear regressions to examine the relationships between BOX scores and both total PCSS scores and specific PCSS symptom profiles (somatic, vestibularocular,cognitive,emotional,and sleep)10in the concussion and control groups. Our secondary analysis was a two-way mixed effects analysis of variance followed by a Tukey post hoc to examine the effect of group (abnormal BOX, normal BOX,and healthy control) on single- and dual-task gait speed. We used an α level of p <0.05, and statistical analyses were performed with Stata (Version 15.1; Stata Corp., College Station,TX,USA).
3. Results
A total of 30 concussed participants(age:14.4±2.2 years,50% female) and 30 controls (age: 14.2 ± 2.2 years, 47%female) completed eye tracking and gait assessments. There were no significant differences between groups for age,height,or mass(Table 1).There was a significant association between total PCSS score and BOX score in the concussion group but not in the control group (Fig. 1). There were no significant associations between the PCSS symptom profiles and BOX scores in the concussion or control groups(Table 2).
The total PCSS and individual symptom profile scores were significantly higher for both concussion groups relative to the control group (Table 1). The BOX score was significantly higher in the abnormal eye tracking concussion group compared to the normal eye tracking concussion group and healthy controls(Table 1).However,the healthy controls had a significantly higher BOX score than the concussion group with normal eye tracking. The concussion group with impaired eye tracking (abnormal BOX score) reported the highest total PCSS score, the highest individual PCSS symptom profile score, and highest BOX score compared to the normal eye tracking concussion group and healthy controls(Table 1).
Single-task gait speed (p=0.63) and dual-task gait speed(p=0.89) were both normally distributed. There was not a significant difference in single- or dual-task gait speed between the groups(Fig.2).

Table 1 Demographic characteristics(mean±SD).

Table 2 Associations between PCSS symptom profiles and BOX scores.
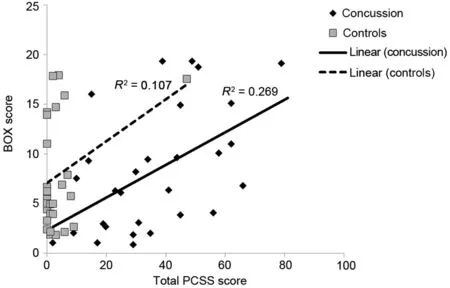
Fig. 1. There was a significant association between total PCSS scores and BOX scores in the concussion group (β=0.16, p=0.004, 95%CI:0.06-0.27) but not in the control group (β=0.21, p=0.08, 95%CI:-0.03 to 0.45). CI=confidence interval; PCSS=Post-Concussion Symptom Scale.

Fig. 2. There was not a significant difference for single-task (F=2.15,p=0.13) or dual-task (F=1.66, p=0.20) gait speed. A Tukey post hoc test revealed no significant differences in single-task gait speed (Abnormal: 1.00±0.14 m/s;Normal:1.11±0.21 m/s;Healthy:1.14±0.18 m/s;p=0.08)or dual-task gait speed (Abnormal: 0.77 ± 0.15 m/s; Normal: 0.84 ± 0.21 m/s;Healthy:0.90±0.18 m/s;p=0.16)between the groups.The error bars represent 95%confidence intervals.
4. Discussion
The results of our study demonstrate a significant association between eye tracking and total PCSS score following concussion, since those with a concussion and abnormal visual tracking also had the highest symptom scores.However,there were no significant associations between eye tracking and the individual PCSS symptom profiles,suggesting that there is no one symptom domain driving these eye tracking deficits.Additionally, the concussion group with abnormal visual tracking walked with a slower gait speed than both the concussion group with normal eye tracking ability and healthy controls.While not statistically significant,this finding still has clinical implications, because motor deficits have been shown to persist beyond concussion clinical recovery.34
We found a significant association between total symptom score and eye tracking in adolescents following concussion,whereby those individuals with abnormal BOX scores also reported the highest PCSS scores within 10 days of concussion.The concussion group with a BOX score that was considered to be abnormal self-reported an average total symptom severity score 20 points higher than the concussion group with normal eye tracking and 47 points higher than the healthy controls.We did not observe any significant associations between the 5 PCSS symptom profiles and BOX scores in either the concussion or control groups. Thus, it does not appear that abnormal eye tracking is being driven by 1 particular symptom domain. However, when compared to the concussion group with normal eye tracking and healthy controls,the concussion group with eye tracking impairments still had significantly worse symptom severity across all 5 domains. Dysfunctional eye movements and visual perception after concussion are associated with increased concussion symptoms,39and changes in visual tracking performance relative to pre-injury reflected clinical symptoms in individuals tested within 2 weeks following concussion.40Additionally, adolescent athletes with convergence insufficiency during a near point of convergence task reported higher total symptom scores than those with normal near point convergence.41These findings suggest that multiple types of visual impairments are related to symptoms, and further support the use of vision testing as an objective clinical measure following concussion.
Our total symptom scores, as well as the 5 PCSS symptom profiles, were higher in our abnormal eye tracking group than those observed in other studies of visual impairments in adolescents;9,10,16,41however, the abnormal concussion group sample size was the smallest of the 3 groups,so future research with a larger abnormal sample is warranted to further examine the relationship between symptoms and eye tracking deficits.The abnormal group was also largely female, so we cannot rule out the influence of sex differences since both female youth and adolescent athletes have been shown to report greater symptom severity, particularly in the somatic domain,but the literature on this point remains mixed.10,38,42While our data only provided a cross-sectional look among a sample of adolescents, visual system dysfunction has also shown to predict prolonged concussion recovery in youth and adult populations.6,43Furthermore, a higher initial somatic and vestibularocular symptom burden has been associated with prolonged symptom duration in adolescent athletes.9Therefore, future research should address whether individuals with abnormal eye tracking take longer to recover than individuals with normal eye tracking.
Unsurprisingly, and consistent with prior eye tracking research in a youth population,16both concussion groups reported significantly higher total symptom severity and individual symptom profile severity than the healthy controls.The BOX scores were also significantly different between groups.For the purpose of our investigation, we divided the concussion group based on whether their BOX score was considered to be normal or abnormal; however, when combined into 1 group,both the mean and median BOX scores were consistent with what has been reported in a similar population.16The healthy controls had a higher BOX score than the concussion group with normal eye tracking, but both scores still fell below the score threshold of 10.Scores of ≥10 are considered to be abnormal.
In addition to higher symptom and BOX scores,those with a concussion and impaired eye tracking also walked with a slower gait speed compared to both the concussion group with normal eye tracking and the healthy controls.The mean difference in single-task gait speed between the concussion group with impaired eye tracking and healthy controls was approximately 0.14 m/s,which is double that of the minimum detectable change (0.074 m/s) previously established for average walking speed in the literature.44This demonstrates a meaningful biological difference between the group with impaired eye tracking and the other groups, despite a lack of statistical significance. A slow gait speed is evidence of a conservative gait strategy,which has been observed in multiple populations following concussion.26,27While the difference in gait speed between the 3 groups did not reach statistical significance,there may still be clinical implications. Gait impairments following concussion have been observed beyond symptom resolution in numerous populations, suggesting that motor deficits may linger beyond clinical recovery.45-47Additionally,a link between conservative gait strategy and subsequent lower extremity musculoskeletal injury has been recently identified,which provides further evidence that motor dysfunction may persist beyond return to play following concussion.48
Impaired eye tracking is not the only ocular deficit present in individuals with a conservative gait strategy. When adolescents with a concussion were divided into 2 groups based on receded or normal near point convergence and compared to a healthy control group, those with abnormal vergence findings walked with a significantly slower single-task and dual-task gait speed that was comparable to the gait speeds within our investigation.5These findings suggest that deficits in smooth pursuit eye movements, not just vergence, may play a role in motor system dysfunction.The anatomical pathways responsible for vergence and pursuit movements are largely controlled by the cerebellum, which also produces the feedforward control required for gait.2,28,49Because the physiological control of pursuit eye movements and motor function has the same foundation, individuals with impaired eye tracking abilities may also be more likely to have motor deficits.Future research should further explore this possibility.
Our study had several limitations. First, we recruited our population from a single specialized sport concussion clinic affiliated with a regional tertiary care children’s hospital.Therefore, our results cannot be generalized to other populations.Second,our sample size of individuals with an abnormal BOX score was limited and predominantly female.We do not believe this factor influenced our visual results, because eye tracking did not previously appear to be associated with sex in a youth concussion population.13However, it could have potentially influenced symptom severity, and future research should examine the role of sex differences in eye tracking with a larger abnormal group. Last, we did not ask participants if they required glasses or corrective devices and will make a point to do so in future studies.
5. Conclusion
There appears to be an association between eye tracking and clinical symptoms following concussion, but it does not appear that abnormal eye tracking is influenced by a single symptom domain. The concussion group with abnormal eye tracking ability had worse overall total symptom severity and higher scores on each of the 5 symptom profiles than those with normal eye tracking and healthy controls. Additionally,the abnormal eye tracking group walked with slower singleand dual-task gait speeds,although the difference was not statistically significant. Regardless, eye tracking appears to be a clinically useful tool for identifying ocular and motor deficits following concussion, and further research is needed to determine if eye tracking can assist clinicians in monitoring those individuals at risk for prolonged concussion recovery.
Acknowledgment
The eye tracking device used in our study was provided by Oculogica Inc.,New York,NY,USA.
Authors’contributions
JRO performed the statistical analysis and drafted the manuscript; WPM III made critical edits to the manuscript; DRH conceived the study, participated in its design and coordination, and made critical edits to the manuscript. All authors have read and approved the final version of the manuscript,and agree with the order of presentation of the authors.
Competing interests
WPM III receives royalties from (1) ABC-Clio publishing for the sale of his books,Kids,sports,and concussion:A guide for coaches and parents and concussions,(2)Springer International for the book Head and neck injuries in young athletes, and (3) Wolters Kluwer for working as an author for UpToDate. His research is funded, in part, by philanthropic support from the National Hockey League Alumni Association through the Corey C. Griffin Pro-Am Tournament and the National Football League. DRH receives research support from the Eunice Kennedy Shriver National Institute of Child Health & Human Development (R03HD094560) and the National Institute of Neurological Disorders and Stroke(R01NS100952 and R41NS103698) of the National Institutes of Health.He has previously received research support from a research contract between Boston Children’s Hospital,Cincinnati Children’s Hospital Medical Center, and ElMindA Ltd.,and the Eastern Athletic Trainers Association Inc.JRO has no competing interests to declare.All the support had no involvement in the study design and writing of the manuscript or the decision to submit it for publication.
 Journal of Sport and Health Science2021年2期
Journal of Sport and Health Science2021年2期
- Journal of Sport and Health Science的其它文章
- Concussion research:Moving beyond the natural history
- Author biographies
- Learners’motivational response to the Science,PE,&Me!curriculum:A situational interest perspective
- Effects of chronic decaffeinated green tea extract supplementation on lipolysis and substrate utilization during upper body exercise
- Training load characteristics and injury and illness risk identification in elite youth ski racing:A prospective study
- Effects of flexibility and strength training on peak hamstring musculotendinous strains during sprinting
