Micropulse laser trabeculoplasty under maximal tolerable glaucoma eyedrops: treatment effectiveness and impact of surgical expertise
Shinji Kakihara, Takao Hirano, Akira Imai, Taihei Kurenuma, Yoshiaki Chiku, Toshinori Murata
Department of Ophthalmology, Shinshu University School of Medicine, Matsumoto, Nagano 390-8621, Japan
Abstract
INTRODUCTION
Glaucoma is a chroni c neurodegenerati ve disease and one of the leading causes of blindness[1-3]. Visual field defects caused by glaucoma are irreversible. Currently, there is no evidence-based treatment for glaucoma other than slowing or preventing the progression of visual field defects by lowering the intraocular pressure (IOP)[4].
Laser trabeculoplasty, a procedure that increases aqueous outflow and decreases IOP, has been reported to be comparable with topical glaucoma eyedrops in terms of efficacy and quality of life[5]. However, with laser trabeculoplasty, there are no concerns regarding complications such as adherence or side effects of medication[6]. Recently, a multicenter, randomized, controlled trial indicated that selective laser trabeculoplasty (SLT) should be considered the first-line treatment for primary open angle glaucoma (OAG)[7]. However, it has been reported that SLT has limited effects on OAG using maximal tolerable glaucoma eyedrops, with a 1-year survival rate of 14.2%[8].
The micropulse laser technique, which divides laser energy into short on-and-off pulses instead of a continuous wave, has been recently developed[9]. It minimizes the heat buildup and thermal damage to adjacent tissues without losing therapeutic effects. The technology applied is not only retinal photocoagulation but also cyclophotocoagulation and trabeculoplasty[10-12]. Previous studies of micropulse laser trabeculoplasty (MLT) that applied micropulse laser technology to laser trabeculoplasty have reported ineffective results[13-14]. However, recently, there have been reports of its effectiveness[11,15-16]. Nevertheless, compared to SLT, MLT is still relatively less common.
In general, there is a learning curve for clinicians as they begin using a new treatment modality. In the field of ophthalmology, for example, there is a learning curve for heads-up vitreoretinal surgery[17]. We consider the steep learning curve associated with the procedure to be one of the reasons for the lack of the widespread use of MLT compared to SLT. We suspect that after a few unsuccessful MLT procedures, clinicians may consider it ineffective and may opt not to use it anymore.
The lack of observable treatment endpoints with MLT, such as the bubbles observed in the SLT procedure, has also led to concerns about the inter-operator variability of IOP[9]. The effectiveness of MLT needs further validation because previous reports have provided inconsistent results and the irradiation conditions are not constant[9,11,13-16].
In this study, we aimed to assess the efficacy of MLT for eyes with OAG using maximal tolerable glaucoma eyedrops. We also aimed assess the impact of surgical expertise performing MLT on its clinical effectiveness among Japanese patients.
SUBJECTS AND METHODS
Ethical ApprovalThis study was approved by the Institutional Review Board of Shinshu University (clinical research approval number: 4722) and adhered to the tenets of the Declaration of Helsinki. Due to the retrospective study design and use of de-identified patient data, the institutional review board waived the requirement for informed consent.
Patient Population and ExaminationsThis was a retrospective case series study that included 42 consecutive eyes of 34 patients with OAG under maximal tolerable glaucoma eyedrops. The patients underwent 360°, 577-nm MLT using IRIDEX IQ 577?Laser Systems (Iridex Corporation, Mountain View, CA, USA) performed by glaucoma specialists from October 2018 to August 2020 at Shinshu University Hospital. All patients underwent comprehensive ophthalmologic examinations before MLT, including measurements of the best-corrected visual acuity (BCVA), Goldmann applanation tonometry, slit-lamp biomicroscopy, gonioscopy, and visual field test (Central 30-2 program, Humphrey Visual Field Analyzer; Carl Zeiss Meditec, Dublin, CA, USA). We excluded eyes that required additional surgery and eyes of patients who dropped out of follow-up involving subsequent IOP analyses.
After topical anesthesia using Benoxil?ophthalmic solution 0.4% (Santen Pharmaceutical Co., Osaka, Japan), a yellow MLT laser was applied confluently to pigmented trabecular meshwork over 360° with a 300-μm spot size setting, 300ms duration, 700-1000 mW power (the power was determined by lowering from 1000 mW to the power resulting in tolerable pain), and 15% duty cycle using the Volk one mirror SLT lens (Volk Optical Inc., Mentor, OH, USA) by a glaucoma specialist who was familiar with gonioscopy. To detect the MLT-related IOP spikes, IOP was measured 1h after a series of MLT lasers. All patients were instructed to continue using the same topical glaucoma eyedrops before MLT and to attend follow-up examinations at 1wk, 1mo, and then every month if possible.
Outcome MeasuresThe primary outcome measure was the survival rate after MLT. Failure was defined as a reduction <20% in IOP from baseline or >21 mm Hg during two consecutive follow-up visits or the need for surgical intervention, as previously described. Kaplan-Meier survival curves were used to determine the effectiveness of MLT.
The IOP before and after MLT were compared. After a single series of MLT, the IOPs were compared to the baseline values at each timepoint (1, 3, and 6mo) using Dunnett’s test. The incidence of IOP spikes was also examined. An IOP spike was defined as an increase in IOP >5 mm Hg from baseline 1h after MLT.
Secondarily, we determined whether the MLT expertise of the glaucoma specialist affected the efficacy of MLT. The eyes were divided into two groups as follows: group 1 (n=21 eyes) underwent MLT performed by a glaucoma specialist who had performed fewer than ten MLT procedures (defined as a less experienced glaucoma specialist) and group 2 (n=21 eyes) underwent MLT performed by a glaucoma specialist who had performed ten or more MLT procedures (defined as an experienced glaucoma specialist). The difference between the two groups was analyzed using a log-rank test.
Demographic and Clinical Data of the PatientsThe following patient data were obtained from the medical records: type of glaucoma, sex, age, status of the lens, gonioscopic grading, BCVA, central corneal thickness, IOP, number of glaucoma eyedrops, mean deviation in visual field examinations, and number of laser applications. BCVA was converted to the logarithm of the minimum angle of resolution (logMAR) BCVA. The angle was graded using Scheie grading (grade I, visible ciliary body; grade II, visible scleral spur; grade III, visible anterior trabecular meshwork; grade IV, no visible structure seen)[18]. For the purpose of quantifying the number of glaucoma eyedrops, topical fixed combination medications were assigned 2 points, and other topical glaucoma medications were assigned 1 point. The medication score was calculated for each eye as described previously[19].
Statistical AnalysisWe conducted all statistical analyses using GraphPad Prism version 7.04 for Windows (GraphPad Software, San Diego, CA, USA). The Chi-square test, Fisher’s exact test, and Mann-Whitney U test were used to compare group 1 and group 2. P<0.05 was considered statistically significant.
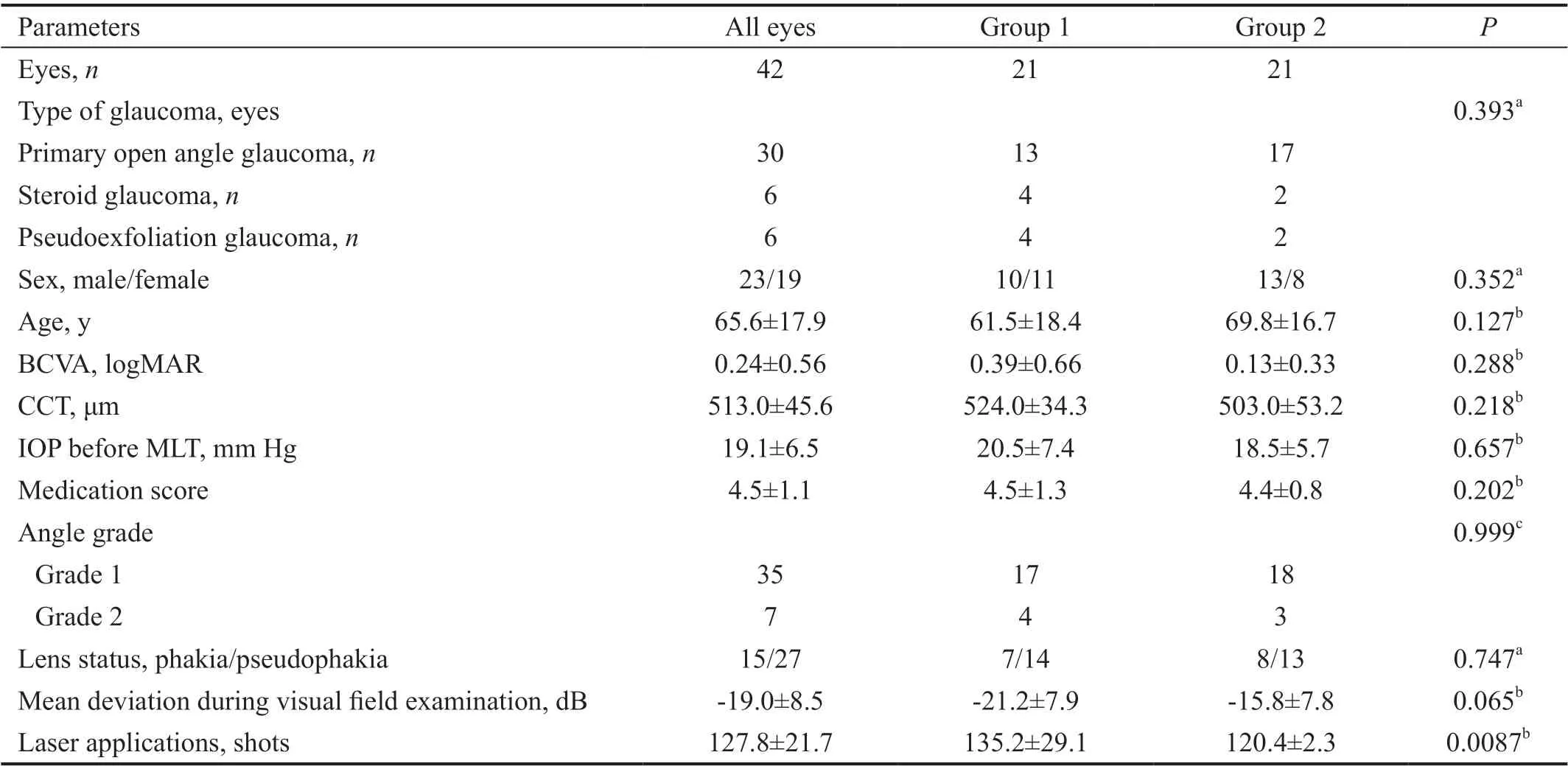
Table 1 Demographic characteristics and clinical data of patients treated with micropulse laser trabeculoplasty mean±SD
RESULTS
Three glaucoma specialists conducted the MLT procedures. Table 1 shows the demographic and clinical data of the patients treated with MLT. The mean age at the time of MLT was 65.6y [standard deviation (SD) ±17.9y]. Among the 42 eyes, six eyes had steroid glaucoma and six eyes had pseudoexfoliation glaucoma. The mean IOP before MLT was 19.1±6.5 mm Hg. The mean medication score was 4.5±1.1. There were no significant differences between the demographic characteristics of group 1 and group 2, except for the number of laser applications (135.2±29.1 shots for group 1 vs 120.4±2.3 shots for group 2; P=0.0087).
The Kaplan-Meier survival analysis showed overall survival rates after MLT of 0.76, 0.48, and 0.44 at 1, 3, and 6mo, respectively (Figure 1). By 6mo after MLT, 10 eyes had undergone additional glaucoma surgery due to inadequate IOP reduction. There were no eyes with IOP spikes after MLT. The mean IOP values before MLT and at 1, 3, and 6mo after MLT were 19.1±6.5 mm Hg (n=42), 16.8±8.8 mm Hg (n=39; P=0.31), 14.0±5.2 (n=30; P=0.0072), and 13.1±5.0 (n=18; P=0.0064), respectively.
Figure 2 shows the results of the secondary outcome. The P-value calculated using the log-rank test was 0.0061. The survival rates of group 1 were 0.62, 0.31, and 0.25 at 1, 3, and 6mo, respectively. In contrast, the survival rates of group 2 were 0.90, 0.64, and 0.64 at 1, 3, and 6mo, respectively.
DISCUSSION
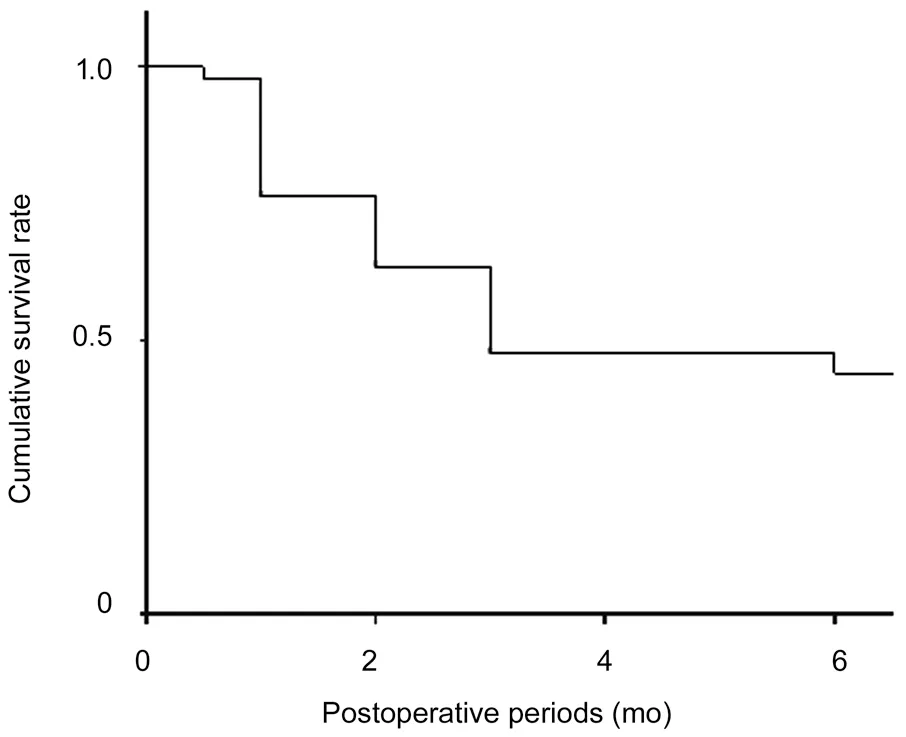
Figure 1 Survival rate after micropulse laser trabeculoplasty The overall survival rates after MLT were 0.76, 0.48, and 0.44 at 1, 3, and 6mo, respectively. Failure was defined as IOP reduction <20% from baseline or >21 mm Hg during two consecutive follow-up visits or surgical intervention.
The results show that the efficacy of MLT at 6mo after surgery was relatively limited, with a survival rate of 0.44. A similar study by Miki et al[8]reported that SLT for OAG using maximal tolerated eye drops (mean±SD, 3.4±1.3 drugs) had survival rates of approximately 0.4 (exact numbers were not given) and 0.14 at 6mo and 1y, respectively. Their definition of failure was IOP reduction <20% from baseline during two consecutive follow-up examinations. During our study, the results of the 6-month follow-up examination were comparable to those of the aforementioned study. The mean medication score for the eyes was 4.5 (SD ±1.1), and most of the eyes had highly advanced glaucoma. This study indicated relatively limited effectiveness in these eyes with highly advanced glaucoma. However, we should not overlook the fact that several eyes experienced IOP reduction, which might have postponed additional surgical intervention.
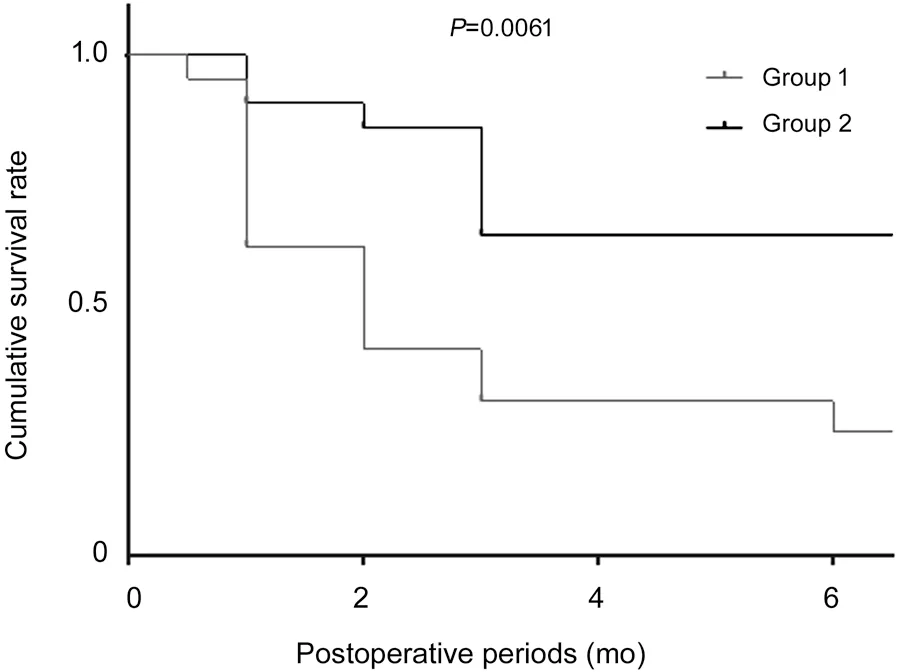
Figure 2 Effect of the MLT proficiency of the surgeon on the survival rate Kaplan-Meier survival analysis showing the survival rates of group 1 and group 2, with a log-rank test showing significant differences in the survival curves of the two groups. The survival rates of group 1 were 0.62, 0.31, and 0.25 at 1, 3, and 6mo, respectively. In contrast, the survival rates of group 2 were 0.90, 0.64, and 0.64 at 1, 3, and 6mo, respectively. The P-value calculated by a log-rank test was 0.0061.
Compared with SLT, MLT does not have a clear observable treatment endpoint[9]. Therefore, it is difficult to validate the procedural endpoint, and we hypothesized that there is a learning curve for MLT. In the present study, MLT procedures performed by a glaucoma specialist familiar with gonioscopy were divided in two groups according to the specialist’s experience with MLT. The survival rates were higher for MLT procedures performed by a glaucoma specialist with sufficient MLT experience than for those performed by a glaucoma specialist with less MLT experience. This result implies that there is inter-operator variability in the effectiveness of MLT to reduce IOP.
There is strong evidence that SLT can effectively reduce IOP, and it is considered a safe treatment with fewer complications[7]. However, the possibilities of IOP spikes and IOP elevation due to peripheral anterior synechia after SLT have been reported[16,20]. In contrast, MLT-induced IOP spikes have been reported only at conservatively suppressed levels[9]. MLT is considered safer than SLT; furthermore, no peripheral anterior synechia occurs because there are no visible tissue changes with MLT.
Conventional treatments such as prostaglandin analogue eyedrops, beta-blocker eyedrops, and filtration surgery aim to reduce IOP without increasing outflow from trabecular meshwork[4]. However, many of the newer glaucoma treatments, both pharmacological and surgical, aim to lower IOP through the main pathway[21-23]. MLT promotes aqueous outflow through the trabecular meshwork, a physiological outlet of the aqueous humor, like many of the new glaucoma treatments. It has been argued that the mechanism of IOP reduction of MLT involves cytokine secretion, matrix metalloproteinase induction, increased cell division, repopulation of burn sites, and macrophage recruitment[24-26]. The combination of various IOP reduction mechanisms may provide a more ideal glaucoma treatment.
This study had several limitations. It was a retrospective case series study with no control group that compared MLT and SLT. All patients were Japanese. Several patients were lost to follow-up, and the follow-up period was short (partly due to the COVID-19 outbreak). Several types of OAG were included, and both eyes from several patients were included in this study. Furthermore, the sample size was small. In the current study, we suggested that the level of MLT expertise may have influenced its effectiveness. Ideally, the Cox proportional hazards model should be utilized to determine factors affecting MLT efficacy other than expertise. However, the Cox proportional hazards model was inappropriate due to the small sample size. We performed a univariate analysis (log-rank test) without considering the influence of variables other than proficiency. According to a power calculation, to analyze the difference between the two groups, the required sample size was 13 eyes for each group; therefore, the sample size of this study was small but fulfilled the requirement[27]. Although the use of MLT as treatment has not been widespread compared to SLT, we considered these data significant given the current situation.
In summary, the results of the current study suggest that the effectiveness of MLT at 6mo to control IOP was relatively limited in eyes with OAG using maximal tolerable glaucoma eyedrops. The effectiveness may be improved if MLT is performed by a glaucoma specialist with sufficient experience. A prospective study with a larger sample size is recommended to evaluate and confirm the effectiveness of MLT.
ACKNOWLEDGEMENTS
We would like to thank Editage (www.editage.com) for their writing support.
Authors’ contributions:Kakihara S had full access to all the data in the present study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Kakihara S, Hirano T; Acquisition of data: All authors; Analysis and interpretation of data: All authors; Drafting of the manuscript: Kakihara S, Murata T; Critical revision of the manuscript for important intellectual content: All authors.
Conflicts of Interest:Kakihara S,None;Hirano T,None;Imai A,None;Kurenuma T,None;Chiku Y,None;Murata T,None.
 International Journal of Ophthalmology2021年3期
International Journal of Ophthalmology2021年3期
- International Journal of Ophthalmology的其它文章
- Corneal stromal mesenchymal stem cells: reconstructing a bioactive cornea and repairing the corneal limbus and stromal microenvironment
- Real-world outcomes of two-year Conbercept therapy for diabetic macular edema
- Role of home monitoring with iCare ONE rebound tonometer in glaucoma patients management
- Comparing posture induced intraocular pressure variations in normal subjects and glaucoma patients
- High interpretable machine learning classifier for early glaucoma diagnosis
- Visual quality after implantation of trifocal intraocular lenses in highly myopic eyes with different axial lengths
