Admission delay is associated with worse surgical outcomes for elderly hip fracture patients: A retrospective observational study
Wei He, Yue-yang You, Kai Sun, Chen Xie, Yue Ming, Li-na Yu, Feng-jiang Zhang, Min Yan,
1 Department of Anesthesiology, the Second Affiliated Hospital of Zhejiang University School of Medicine, Hangzhou 310009, China
2 Jiangsu Province Key Laboratory of Anesthesiology, Jiangsu Province Key Laboratory of Anesthesia and Analgesia Application Technology, Xuzhou Medical University, Xuzhou 221004, China
KEY WORDS: Geriatric; Hip fracture; Admission delay; Mortality; Complications
INTRODUCTION
With the aggravation of the aging population, hip fractures in elderly people are becoming increasingly prevalent. According to an epidemiological study,hip fractures worldwide would exceed 6 million by 2050.[1]As we all know, hip fractures often bring about many adverse consequences, including high mortality, difficulty in recovering pre-injury activity and complications such as pneumonia, pulmonary embolism(PE) and deep venous thrombosis (DVT).[2]
In order to improve the prognosis of fracture surgery, experts and scholars have carried out a great deal of relevant studies,[3-7]one kind of which is about the relationship between preoperative waiting time and postoperative death and complications. Of these researches,[3,4,6]some suggest early surgery may be beneficial, and guidelines in different countries recommend corresponding operation timing of 36 or 48 hours after admission.[8,9]
However, most studies only focus on the time from admission to operation, not taking the time from injury to admission into account.[3-6]Nevertheless, according to our clinical observation, many Chinese patients tend to delay admission, which we believe cannot be neglected.At the same time, considering the huge differences in the medical systems and economic levels in different countries and regions, findings of previous researches may not conform to the situation of China.
Therefore, the aim of this study is to investigate the actual pre-admission waiting time when Chinese elderly patients are subjected to hip fractures, and to explore the influence of admission delay on postoperative mortality and morbidity. We hypothesized that delayed admission could result in worse outcomes.
METHODS
Setting and data sources
This is a retrospective study conducted in the Second Affiliated Hospital of Zhejiang University School of Medicine. Characteristics data and partial surgical outcomes of patients were collected from the hospital's Electronic Medical Record System (EMRS),while information on anesthesia and surgery were obtained from another system, the Docare system.Postoperative survival was acquired by telephone followup. Permission was acquired from the Human Subject Research Committee of our hospital (Approval Number:I2019001002) before carrying out the research. Personal informed consent was not required.
Inclusion and exclusion criteria
Patients over 65 years old who underwent hip fracture surgery between January 1, 2014 and December 31, 2017 were included. We set the year to between 2014 and 2017 because we can only extract data from EMRS and Docare system as early as 2014 and we lacked follow-up data, especially one-year mortality, of subsequent patients the year after 2017. Patients with multiple injuries or multiple fractures, high-energy injuries caused by car accidents or fall from height,pathological fractures, hip fracture history, bilateral fracture were excluded.
Main exposures and covariates
The main exposure in the study was admission timing which was obtained from chief complaint in medical records (e.g., “one day of pain in the left hip caused by a fall”). Timing of admission was recorded as day 0 for the first day of injury, day 1 for the next day, etc. Admission of one month or later was recorded as day 30. Interval from hospitalization to operation was calculated according to the date and time of hospitalization and operation. Other covariates that were clinically meaningful or reported by previous studies[10,11]included age, sex, ASA classification, fracture type,operative method, anesthesia method, intraoperative blood loss, preoperative comorbidities (pneumonia,hypertension, coronary heart disease, heart failure,stroke, diabetes mellitus, renal insufficiency, Alzheimer's disease, Parkinson's disease) and the latest preoperative laboratory examinations (hemoglobin, leukocyte,platelet, albumin, creatinine, C-reactive protein).
Primary and secondary outcomes
The primary outcome was 1-year all-cause mortality.The secondary outcomes were 1-month mortality,3-month mortality, ICU admission and postoperative pneumonia. Postoperative pneumonia referred to pneumonia that did not occur before surgery but emerged after surgery. Postoperative survival status and survival time were obtained by telephone follow-up, while other outcomes were acquired through the EMRS.
Statistical analysis
Continuous variables were presented as mean with standard deviation (SD) or median with interquartile range (IQR), and categorical variables were presented as frequencies with percentages. For the comparison of differences between groups, continuous variables were tested by t test or non-parametric test, and categorical variables were tested by Chi-square test or Fisher exact test. Correlation among continuous variables was assessed by Pearson's coefficient. Variables with P<0.1 and correlation coefficient among them (collinearity)less than 0.25[12]would be included in multivariate logistic regression. Considering mortality rate varies at different time point within one year after operation, we also conducted an additional survival analysis via Kaplan Meier method. SPSS version 25.0 was used for statistical analysis and a two-tail significance level of P<0.05 was considered statistically significant.
RESULTS
Procedure of patient selection was showed in Figure 1. Totally 970 patients were included in this study, and 867(89.4%) of them were successfully followed up. Among those followed up patients, 648 (74.7%) were female,average age was 81.2 years, 582 (67.1%) had femoral neck fracture, and 486 (56.1%) had hip replacement surgery. The proportion of patients hospitalized on day 0, day 1, day 2 after injury was 25.4%, 54.7% and 66.3%, respectively (Figure 2). However, still 12.6%patients visited hospital one week later after injury. Mean time from admission to surgery was 5.2 days (standard deviation 2.8 days). The mortality of one year, three month and one month after operation was 10.5% (n=91),5.4% (n=47) and 3.3% (n=29), respectively.
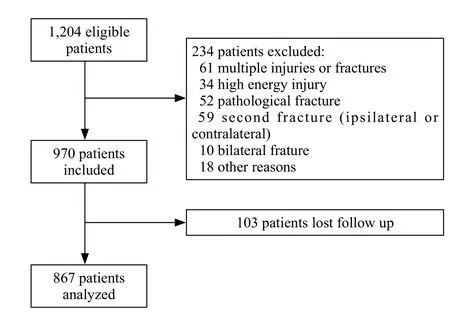
Figure 1. Flow chart.
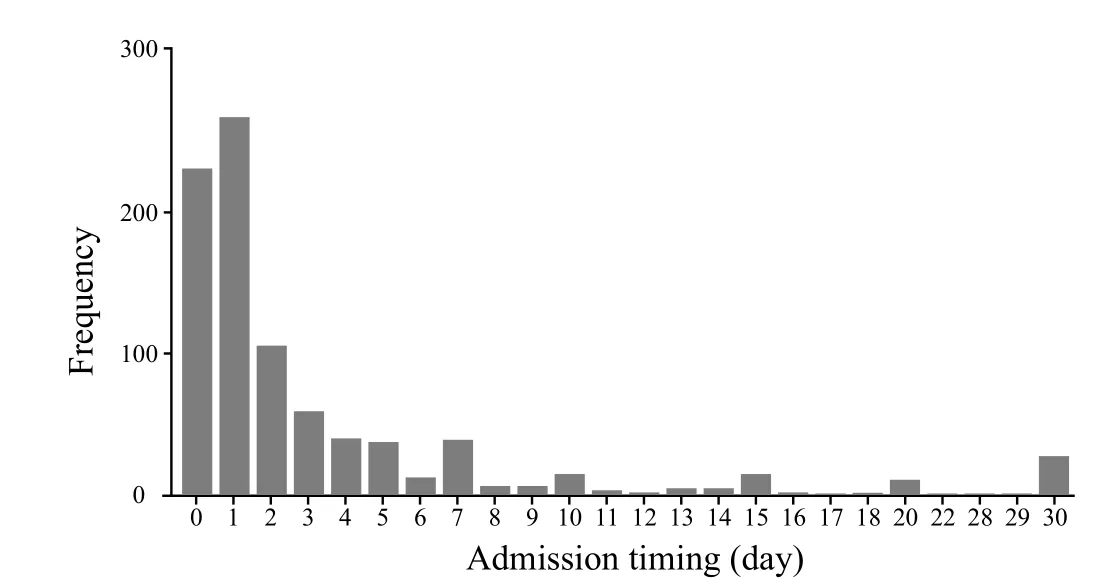
Figure 2. Bar chart of admission timing.
In univariate logistic regression of 1-year mortality,we found that admission delay over one week could be a potential risk factor (Table 1). Other variables with P<0.1 in univariate analysis were age, gender, ASA classification, fracture type, preoperative pneumonia,preoperative renal insufficiency, hemoglobin level,albumin level, creatinine level, admission-to-surgery time. Collinearity existed among hemoglobin level,albumin level, ASA classification and age (0.3< |r| <0.5).High correlation also existed between preoperative renal insufficiency and creatinine level (r=0.6). But there was no correlation between injury-to-admission timing and admission-to-surgery timing. Thus, we finally included age, gender, preoperative pneumonia,fracture type, preoperative renal insufficiency, injury-toadmission timing and admission-to-surgery timing in the multivariate regression (Table 2). Hence, we determined that admission delay over one week was associated with 1-year mortality.
Characteristics and surgical outcomes of patients who were admitted to hospital within or over one week after injury were given in Table 3 and Table 4. An additional analysis showed patients admitted to hospital within one week after injury would have a better survival during the first postoperative year (Figure 3).
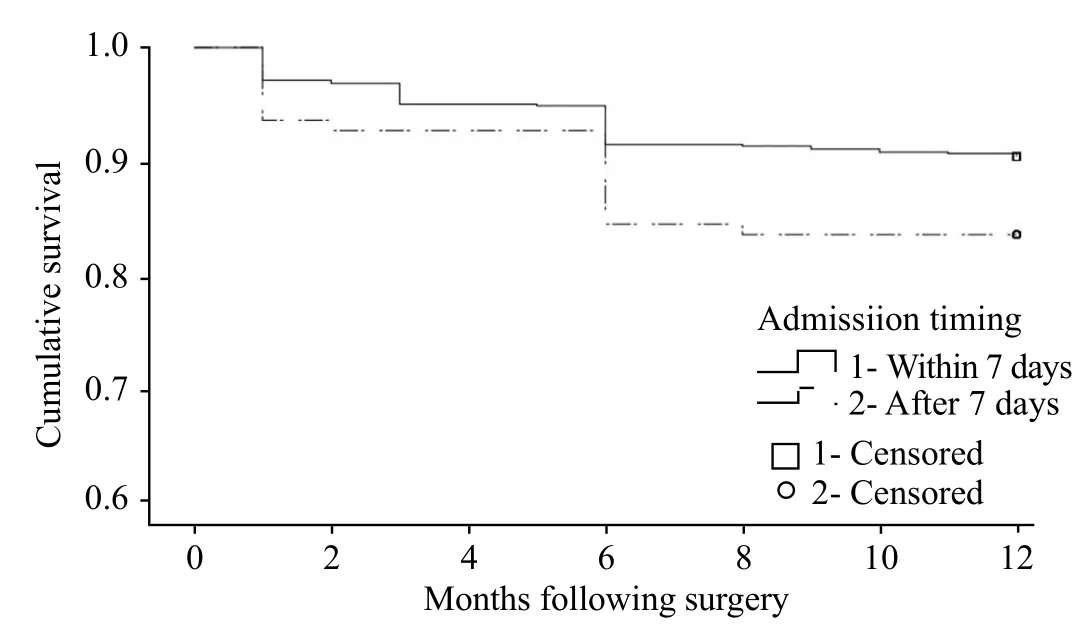
Figure 3. Survival analysis of patients by admission timing (Log Rank P=0.027).
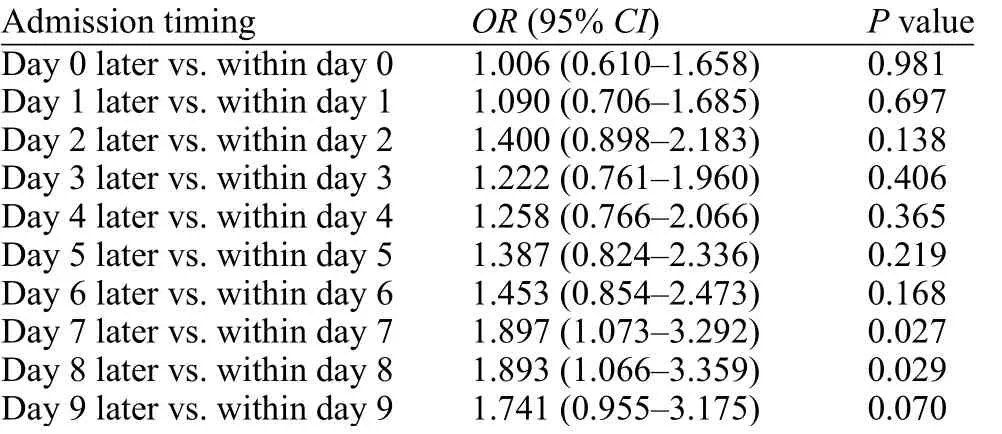
Table 1. Univariate logistic regression for 1-year mortality with admission timing dichotomized according to different cut point

Table 2. Multivariate logistic regression analysis for 1-year mortality
DISCUSSION
In our study, we found that compared with patients admitted to hospital within one week of injury,patients with later admission would have significantly higher 1-year mortality, but not 3-month mortality or postoperative pneumonia. Admission delay over one week was also related to higher 1-month mortality and ICU admission though not statistically significant.
As far as we know, this is the first report of the effect of delayed admission on mortality and morbidity in Chinese elderly hip fracture patients. Previous studies about the effect of admission timing on surgicalprognosis are also rare. Paul et al[7]studied the waiting time of hospitalization in their research. They found that patients who received operation within 2 days after injury had lower in-hospital mortality. Uzoigwe et al,[6]however, did not take delayed hospitalization into account, claiming this interval is difficult to obtain and cannot be intervened by medical staff. While, many Chinese patients may not present to the hospital timely after fracture, and not much information is available.Compared to former researches,[6,7]seven days as a recommended admission timing may not be early, but in our research, still 12.6% patients admitted later than this cut point. These people are just the potential patients who can benef it a lot. So, it is still meaningful to propose this time window.
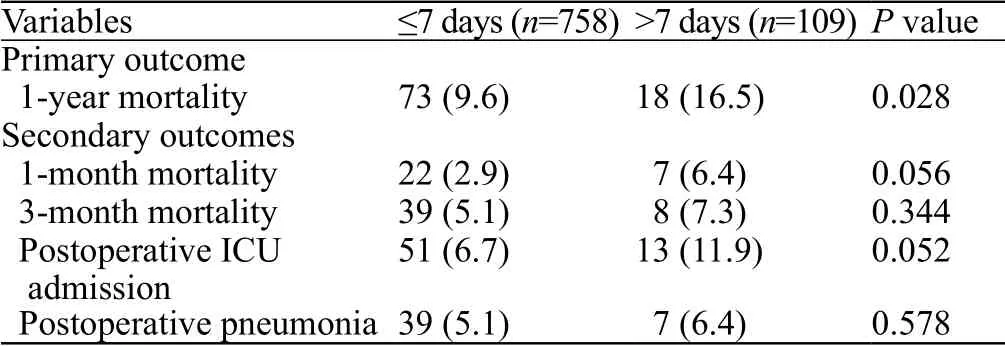
Table 4. Primary and secondary outcomes of patients by admission timing, n (%)
As for admission-to-surgery timing, previous studies[13,14]suggested that patients who had surgery within 48 hours of admission would have better outcomes. Our study also confirmed early surgery patients would have lower 1-year mortality, though not statistically significant. In fact, the average time ofadmission-to-surgery was around 5.2 days no matter patients were admitted early or late, which was far beyond the current recommendation of 48 hours. This reminds us although guidelines around the world all propose early surgery, the status quo in our country is still not optimistic. On the one hand, we need to emphasize early surgery after admission, on the other hand, we also need to emphasize early admission.

Table 3. Characteristics of patients by admission timing
The key to advocating early surgery is to restore motor function at an early stage and to reduce complications associated with bed rest. Such complications can occur not only postoperatively but also preoperatively. This is the reason why we studied the timing of admission and its influence on outcomes. In fact, our study showed that patients admitted one week after injury had higher incidence of preoperative pneumonia and lower level of albumin. We speculate the intrinsic link is that with admission delay continuing and bedridden time prolonging, preoperative pneumonia would appear and aggravate, and nutritional status would deteriorate.In other words, delayed hospitalized patients are worse off, often as a result, not as a cause. Yet, further research is needed to prove this speculation. Here, it is worth mentioning that researches have suggested that preoperative malnutrition will increase the probability of postoperative complications and the risk of death.[15,16]
The importance of our research lies in its clinical implications, that is, we need to recommend rational clinical practice in line with the present condition of our own country. In addition to advocating early surgery after admission, we also need to call for early admission. The former is the field of quality improvement,[17]which can be directly intervened by medical staff, while the latter requires the improvement of social awareness, publicity and education.
Limitations also exist in this study. Firstly, this is a retrospective study with data from a single center. The results may not be representative. But just because of that, we have more reasons to speculate that delayed admission may be more common in areas with underdeveloped transportations, backward economic levels and low educational levels. Secondly, the injuryto-admission time is not that precise. The collection of time is mainly based on chief complaints in medical records, and most of them can only be accurate to days.Although day is not as precise as hour, it does not prevent us determining the cut point of one week. At the same time, it also directly reflects elderly patients with hip fracture in our country will not be hospitalized in time and waiting time has great variation. Thirdly,postoperative mortality is mainly obtained by telephone follow-up with a loss rate of about 10%, which may bias the result. Fourthly, the present study lack information on pulmonary embolism (PE) and deep venous thrombosis(DVT) due to limited and incomplete data, so we don't know what role PE/DTV would play in the prognosis of patients. We also lack enough data on dementia, which is reported to be closely related to the prognosis of hip fracture patients.[18]But we obtained data of patients who were diagnosed as Alzheimer's disease, and we did not f ind its correlation with postoperative mortality. Finally,although this study found that a considerable number of patients had delayed admission, the reasons for admission delay were still unknown, thus a prospective research is needed to tell us what might be done to make a change.
CONCLUSION
Under the current conditions in China, admission delay is significantly associated with higher 1-year mortality for elderly hip fracture patients. In addition to early surgery highlighted in the guidelines, we also advocate early admission. Moreover, we suggest both health administrators and clinicians should strengthen education and publicity of hip fracture, to improve the whole society's awareness of severity of this kind of severe disease, to improve timely admission rate, and finally to improve survival of those vulnerable ones.
Funding:This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval:The study has been approved by the Human Subject Research Committee of the Second Affiliated Hospital of Zhejiang University School of Medicine (I2019001002).
Conflicts of interest:All authors declare no financial and personal relationships with other people or organizations.
Contributors:WH and YYY contributed equally to this study. WH and YYY: study design; acquisition, analysis, and interpretation of data; preparation of initial draft. Kai sun: study design; analysis and interpretation of data. CX and YM: study design, acquisition of data. LY, FJZ, and MY: study design and manuscript revision. All authors read and approved the final manuscript.
 World journal of emergency medicine2020年1期
World journal of emergency medicine2020年1期
- World journal of emergency medicine的其它文章
- Surgical closure of large splenorenal shunt may accelerate recovery from hepato-pulmonary syndrome in liver transplant patients
- Investigations for the assessment of adult patients presenting to the emergency department with supraventricular tachycardia
- Epidemiological characteristics and disease spectrum of emergency patients in two cities in China: Hong Kong and Shenzhen
- Role of penehyclidine in acute organophosphorus pesticide poisoning
- The first two cases of transcatheter mitral valve repair with ARTO system in Asia
- A pulmonary source of infection in patients with sepsis-associated acute kidney injury leads to a worse outcome and poor recovery of kidney function
