柯薩奇病毒A6感染致足月新生兒NEC、腸穿孔一例
林瀚妮?李管明?張靄潤?翁立堅?房曉祎
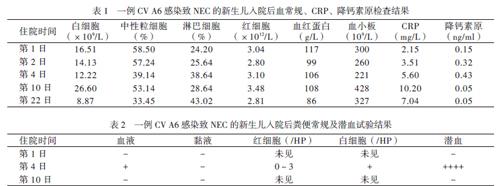
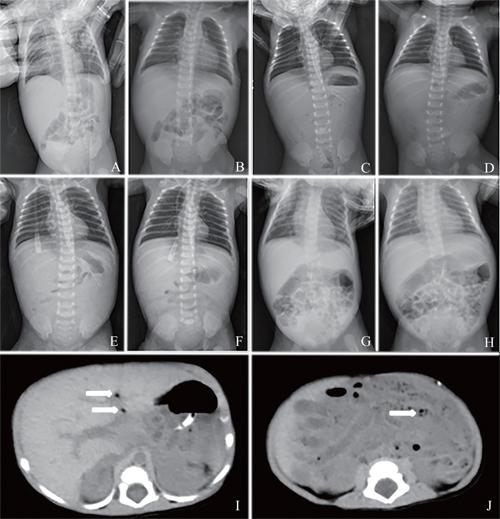
【摘要】新生兒腸道病毒感染以隱匿感染為主,癥狀不典型,但可發生嚴重并發癥,甚至導致死亡,可引起新生兒病房暴發性感染。該文報道1例因感染柯薩奇病毒(CV)A6導致壞死性小腸結腸炎、腸穿孔、感染性休克的新生兒。患兒為女性,因皮膚黃染及排血便而入院,結合臨床表現及完善相關檢查后考慮為壞死性小腸結腸炎、敗血癥。經予積極綜合治療后,包括禁食、胃腸減壓、擴容、抗感染、輸注血液制品等,患兒于住院第28 日痊愈并出院。患兒出院后大便逆轉錄PCR結果回報:住院第2日、第23日大便 CV A6均陽性,遂補充診斷為新生兒CV感染。新生兒敗血癥需重視腸道病毒感染可能,及時進行病原學檢測十分重要。
【關鍵詞】腸道病毒;柯薩奇病毒;新生兒;感染性休克;腸穿孔;壞死性小腸結腸炎
Necrotizing enterocolitis and intestinal perforation in a term infant caused by Coxsackievirus A6: a case report Lin Hanni, Li Guanming, Zhang Airun, Weng Lijian, Fang Xiaoyi. Department of Neonatology, the Seventh Affiliated Hospital of Sun Yat-sen University, Shenzhen 518107, China
Corresponding author, Fang Xiaoyi, E-mail: judyfangxy@ 126. com
【Abstract】Neonatal enterovirus (EV) is mainly manifested with occult infection and atypical symptoms. However, it may cause severe complications, and even death. It can also lead to the outbreak of nosocomial infection in the neonatal ward. In this article, one female case of neonatal necrotizing enterocolitis, intestinal perforation and septic shock caused by Coxsackievirus (CV) A6 infection was reported. She was admitted to hospital due to yellow skin and bloody stool. The possibility of necrotizing enterocolitis and septicemia was considered according to clinical manifestations combined with relevant examinations. After active and comprehensive treatment including fasting, gastrointestinal decompression, volume expansion, anti-infection, and infusion of blood products, the neonate was cured and discharged. At the 2nd and 23rd d after hospitalization, RT-PCR revealed the stool samples were positive for CV A6. Hence, she was diagnosed with neonatal CV infection. The possibility of EV infection should be considered for neonatal septicemia. It is of significance to deliver detection of the pathogen.
【Key words】Enterovirus;Coxsackievirus;Newborn;Septic shock;Intestinal perforation;
Necrotizing enterocolitis
腸道病毒(EV)是單股正鏈RNA病毒,屬于微小RNA病毒科,是嬰幼兒感染常見病毒[1]。EV型別眾多,包括:①人脊髓灰質炎病毒1 ~ 3型;②人柯薩奇病毒(CV),A組(CVA)1 ~ 22型和24型,CV A23型為埃可病毒9型,CV A6可引起手足口病,B組(CVB)1 ~ 6型;③致腸細胞病變人孤兒病毒(ECHO),即埃可病毒1 ~ 9、11 ~ 21、24 ~ 27、29 ~ 33共29個血清型,E22型、23型分別是副腸孤病毒1型和2型;④新型EV 68 ~ 72型,其中1971年分出的EV D70型可引起急性出血性結膜炎,EV A71型可引起手足口病,EV A72型為甲型肝炎病毒[2]。新生兒可通過胎盤、產道或生后獲得性感染EV,并可因母親、醫護人員或新生兒間交叉感染在新生兒病房引起EV暴發流行[3]。新生兒感染多由CV和ECHO引起,雖然大多數患兒出現的是非典型或輕微的臨床癥狀,但也有發生危及生命的感染可能而導致預后不良[4-5]。在本文中,筆者報道1例因感染CV A6而引發壞死性小腸結腸炎(NEC)的新生兒病例,以引起臨床醫師對新生兒EV感染的重視,加強管理。
病例資料
一、主訴及病史
臨床上可通過血、糞便、尿液等病毒分離方法明確EV感染的診斷,但耗時較長、不實用,目前多采用RT-PCR方法檢測病毒血清型,較為快速、準確。
新生兒EV感染無特殊治療,主要是對癥及支持治療。本例經過抗休克、禁食、胃腸減壓、抗生素及維持內環境穩定等保守治療后癥狀逐漸好轉,2周后重新喂養、停抗生素,胃腸功能恢復,全身表現良好,最終獲得痊愈。有文獻報道大劑量丙種Ig能提供特異性抗體,可以改善嚴重EV感染的預后,但缺乏科學證據支持[14]。有臨床試驗證實EV衣殼抑制劑Pocapavir、Pleconaril能較快清除病毒、降低病死率,但無法逆轉已發生的器官損傷,對嚴重EV感染效果不佳[15-16]。
綜上所述,新生兒EV感染可致嚴重并發癥,臨床醫師必須高度重視。在臨床工作中,我們必須密切觀察新生兒病情變化,做到早預防、早識別和早處理,避免發生嚴重并發癥。
參 考 文 獻
[1] Wallace SS, Lopez MA, Caviness AC. Impact of enterovirus testing on resource use in febrile young infants: a systematic review. Hosp Pediatr, 2017, 7(2):96-102.
[2] King AMQ, Adams MJ, Carstens, Lefkowitz EJ. Virus taxon-omy: classification and nomenclature of viruses: ninth report of the international committee on taxonomy of viruses. San Diego: Elsevier, 2012: 931-934.
[3] 郭玥馨. 新生兒腸道病毒感染的高危因素分析. 臨床研究, 2017,25(1): 194-195.
[4] Centers for Disease Control and Prevention (CDC). Nonpolio enterovirus and human parechovirus surveillance——United States, 2006-2008. MMWR Morb Mortal Wkly Rep, 2010, 59(48): 1577-1580.
[5] Chuang YY, Huang YC. Enteroviral infection in neonates. J Microbiol Immunol Infect, 2019 , 52(6):851-857.
[6] Lagae D, Rigo V, Senterre JM, Kalenga M, Piérart J. Early enterovirus neonatal infection: when should we think about it?? Rev Med Liege, 2016 , 71(2):78-82.
[7] Harik N, DeBiasi RL. Neonatal nonpolio enterovirus and parechovirus infections. Semin Perinatol, 2018, 42(3):191-197.
[8] 林瀚妮, 房曉祎, 李管明, 張靄潤, 李寧寧, 林霓陽. 新生兒重癥監護病房住院新生兒糞便腸道病毒類型及感染臨床特點. 中華婦幼臨床醫學雜志(電子版),2019, 15(6):681-687.
[9] Berger JR, Chumley W, Pittman T, Given C, Nuovo G. Persis-tent coxsackie b encephalitis: report of a case and review of the literature. J Neurovirol, 2006, 12(6): 511-516.
[10] Dunn J. Enteroviruses and Parechoviruses. Microbiol Spectr, 2016, 4(3): 1-22.
[11] Morriss FH Jr, Lindower JB, Bartlett HL, Atkins DL, Kim JO,Klein JM,Ford BA. Neonatal enterovirus infection: case series of clinical sepsis and positive cerebrospinal fluid polymerase chain reaction test with myocarditis and cerebral white matter injury complications. AJP Rep, 2016, 6(3): e344-e351.
[12] Jones G, Muriello M, Patel A, Logan L. Enteroviral meningo-encephalitis complicated by central diabetes insipidus in a neonate: a case report and review of the literature. J Pediat Inf Dis Soc, 2015, 4(2): 155-158.
[13] Amdani SM, Kim HS, Orvedahl A, John AO, Said A, Simpson K. Successful treatment of fulminant neonatal entero-viral myocarditis in monochorionic diamniotic twins with cardiopulmonary support, intravenous immunoglobulin and pocapavir. BMJ Case Rep,2018,2018:bcr2017224133.
[14] Ooi MH, Wong SC, Lewthwaite P, Cardosa MJ, Solomon T. Clinical features, diagnosis, and management of enterovirus 71. Lancet Neurol, 2010, 9(11): 1097-1105.
[15] Collett MS, Hincks JR, Benschop K, Duizer E, van der Avoort H, Rhoden E, Liu HM,? Oberste MS, McKinlay MA, Hartford M. Antiviral activity of Pocapavir in a randomized, blinded, placebo-controlled human oral poliovirus vaccine challenge model. J Infect Dis, 2017, 215(3): 335-343.
[16] Abzug MJ, Michaels MG, Wald E, Jacobs RF, Romero JR, Sánchez PJ, Wilson G, Krogstad P, Storch GA, Lawrence R, Shelton M,Palmer A, Robinson J, Dennehy P, Sood SK, Cloud G, Jester P, Acosta EP, Whitley R, Kimberlin D, the National Institute of Allergy and Infectious Diseases Collaborative Antiviral Study Group. A randomized, double-blind, placebo-controlled trial of Pleconaril for the treatment of neonates with enterovirus sepsis. J Pediatric Infect Dis Soc, 2016, 5(1): 53-62.
(收稿日期:2020-02-22)
(本文編輯:洪悅民)

