Extensive multifocal and pleomorphic pulmonary lesions in Waldenstr?m macroglobulinemia: A case report
De-Feng Zhao, Hao-Yong Ning, Jian Cen, Yi Liu, Li-Ren Qian, Zhi-Hai Han, Jian-Liang Shen
De-Feng Zhao, Department of Hematology, Beijing Boren Hospital, Beijing 100070, China
Hao-Yong Ning, Department of Pathology, Navy General Hospital of PLA, Beijing 100048,China
Jian Cen, Yi Liu, Li-Ren Qian, Jian-Liang Shen, Department of Hematology, Navy General Hospital of PLA, Beijing 100048, China
Zhi-Hai Han, Department of Respiratory Care, Navy General Hospital of PLA, Beijing 100048,China
Abstract
Key words: Waldenstr?m macroglobulinemia; Lung; Amyloidosis; Computed tomography; Case report
INTRODUCTION
Amyloidosis refers to a series of diseases characterized by the extracellular pathological deposition of amyloid-like fibrillary proteins in different organs and can be classified into secondary and primary amyloidosis[1]. Secondary disorders are more common and occur following other diseases such as lymphoproliferative or plasma cell disorders[1]. The kidney and heart are the most commonly affected organs, and amyloidosis of the lower respiratory tract occurs very rarely[1,2]. Nodular lesions or diffuse infiltrations of amyloid in alveolar septa are the most common imaging features of amyloidosis affecting the lungs[2]. Needle core biopsy is used to confirm the diagnosis, but if the evaluation of the biopsy is improper, these changes can be easily misdiagnosed as tuberculosis, tumors, or other inflammatory infiltrations[2].
Waldenstrom macroglobulinemia (WM) is a rare (0.34-0.55 per 100000) B-cell lymphoproliferative neoplasm characterized by the infiltration of bone marrow by lymphoplasmacytic cells that secrete a monoclonal immunoglobulin M (IgM)protein[3,4]. The proliferation of IgM-producing plasmacytoid lymphocytes leads to excessive monoclonal IgM levels, which may lead to a variety of different clinical manifestations[3,4]. The complications of WM include amyloid light chain amyloidosis[4].
CASE PRESENTATION
Chief complaints
A 60-year-old male patient who experienced intermittent breath-holding for 6 mo(symptom aggravation for 3 mo) was admitted to our hospital on August 14, 2017.From May 2017 onwards, the patient complained of the sensation of the pressure in the chest with aggregated suffocation, and he had an apparent decrease in exercise capacity.
History of present illness
Chest computed tomography (CT) examination indicated multiple pulmonary cavities in the upper lobes of both lungs, with pulmonary consolidation, ground-glass opacities, patchy infiltrates, fibrous bands, large bullae, and enlarged lymph nodes in the mediastinum (Figure 1).
After receiving an anti-infective treatment, the breathing difficulty did not improve.In addition, similar lesions were observed after performing a second CT examination,and the anti-infection treatment was stopped.
這次勝利付出了慘重的代價!一連共付出了十八條寶貴的生命。馬國平想著,順著坡坎一步步向半山腰走去。半道上,見幾個擔架員,抬著一副副用白布蒙得嚴嚴實實的擔架走過來。

Figure 1 Chest computed tomography examination showing extensive multifocal and pleomorphic lesions in the lungs, including multiple pulmonary cavities, consolidation, ground-glass opacities, patchy infiltrates,fibrous bands, and large bullae. A and B: Upper lung; C: Middle lung; D: Lower lung.
History of past illness
The patient was a heavy smoker (20 cigarettes/d for 40 years) with no history of lung disease or tumors.
Personal and family history
No similar phenotypic features were observed in other members of his family.
Physical examination upon admission
During hospitalization, diagnostic fiberoptic bronchoscopy revealed normal findings.In addition, a multi-target nucleic acid amplification assay using bronchoalveolar lavage fluid showed negative results. Arterial blood gas analysis indicated that the value for oxygen partial pressure was 69.2 mmHg, while relative oxygen saturation was 94.5%. Multiple pulmonary function tests showed mild mixed (obstructive and restrictive) ventilatory dysfunction, small-airway dysfunction, a slight reduction in lung volume, normal airway resistance, a moderate reduction in pulmonary diffusing capacity, and a slight reduction in diffusing capacity for carbon monoxide per liter of alveolar volume (DLCO/VA) (corrected for patient’s hemoglobin). Moreover, no abnormalities were found on electrocardiogram and echocardiography.
Laboratory examinations
Serological examination revealed a remarkable increase in serum IgM levels (30.24 g/L, compared to the average concentration of 0.4-2.30 g/L). In addition, serum immunofixation electrophoresis uncovered the presence of light chain λ and heavy chain μ. Bone marrow examination showed hyperplastic hematopoiesis as well as “a string of copper coins”-like arrangement of red cells. Furthermore, immunophenotypic analysis of bone marrow cells indicated that CD45+CD19+ cells (which accounted for 2.2% of all the nucleated cells) were all expressing HLA-DR, CD20,CD22, LAMBDA, and cLAMBDA, suggesting the presence of abnormal monoclonal B lymphocytes. Comparatively, CD45dimCD38st cells (accounting for approximately 0.4% of all the nucleated cells) all expressed CD19, CD138, and cLAMBDA, further suggesting the presence of abnormal monoclonal plasma cells. In addition, the L265P mutation in the MYD88 gene was detected using the polymerase chain reaction technique, even though the G-banding technique suggested a normal karyotype. Bone marrow biopsy showed hyperplastic hematopoiesis with a normal erythroid/myeloid morphology, slight accumulation of megakaryocytes, and scattered infiltration of plasma cells and lymphocytes.
On September 4, 2017, the examination by Congo red staining showed Congo redpositive amyloid deposits in the biopsy specimens (Figure 2). Immunohistochemistry indicated that they were lambda-positive (+++) and appeared as a typical “applegreen birefringence” under a polarizing microscope (Figure 3).
Imaging examinations
On September 4, 2017, a CT-guided percutaneous pulmonary biopsy was performed in the left lower lobe of the lung with pulmonary consolidation and indicated that the alveolar structure disappeared and that a large amount of amyloid-like deposition was present along with the infiltration of very few lymphocytes and plasma cells(Figure 4).
FINAL DIAGNOSIS
Based on these findings, the patient was diagnosed with WM accompanied by pulmonary amyloid-like depositions.
TREATMENT
From October 15, 2017, the patient was treated with the combined treatment of dexamethasone + rituximab + lenalidomide over four courses (Mabthera, 375 mg/m2on day 0; lenalidomide, 25 mg, PO, QD, from day 1 to 21; dexamethasone, 20 mg QD,once a week; 28 d as a course).
OUTCOME AND FOLLOW-UP
On March 8, 2018, the patient underwent further tests. The serum IgM level was slightly reduced (26.93 g/L). Besides slightly alleviated dyspnea, no obvious alterations were observed by chest CT. Considering that the patient’s IgM concentration almost remained unchanged, he was placed on an alternative combined treatment using ibrutinib + dexamethasone.
DISCUSSION
WM is a type of small lymphocytic lymphoma that mainly affects the bone marrow,spleen, and lymph nodes. Patients with WM may develop amyloidosis. The patient reported here had WM and lung amyloidosis, manifesting as a wide range of pulmonary lesions and a variety of morphological features, which was a rare case.
WM is a rare and usually insidious small lymphocytic lymphoma[4], and is rarely detected as extramedullary involvement or leukemia evolution[5]. Amyloidosis is a rare complication of WM[4]. Amyloidosis involving the pulmonary parenchyma is usually characterized by a number of solitary pulmonary lesions and by diffuse alveolar septal infiltration[6].
A variety of hematological malignancies such as myeloma, lymphoma, and chronic lymphocytic leukemia can be combined with pulmonary amyloidosis or light chain deposition disease. A subset of patients with WM demonstrates extramedullary involvement (4.4%), and the most frequent extramedullary disease site involved is the lungs (30%)[5,7], resulting in a relatively low prevalence of pulmonary involvement in patients with WM. Besides pulmonary amyloidosis or light chain deposition disease,infiltration or compact mass composed of lymphoma cells can also be detected.Imaging examinations normally reveal some changes, including diffuse pulmonary nodules, pulmonary mass, infiltration, or pleural effusions[8]. The patient reported here had a wide range of pulmonary lesions and a variety of morphological features,which was indeed a rare case. Yet, there is still a possibility that some of the lesions on CT could be ascribed to the patient’s heavy smoking history. Because of invasiveness and the risk of complications, only one lung lesion was biopsied, and the pathological examination clearly revealed amyloid deposition.
Currently, there is no standard treatment for symptomatic or progressive WM,although traditional drugs such as chlorambucil and cyclophosphamide as well as nucleoside analogs such as cladribine and fludarabine are usually prescribed for patients with WM. New effective drugs include lenalidomide, thalidomide,bortezomib, and rituximab[4,9,10], while some other medications are currently undergoing clinical trials[9]. After four courses of combined treatment with lenalidomide + rituximab + dexamethasone, the IgM levels were not significantly reduced. Therefore, new options for the patient’s treatment are indeed required in the future.
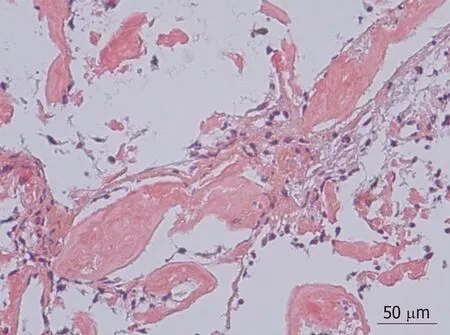
Figure 2 Needle punch biopsy specimen stained with Congo red showing amyloid deposition (magnification,× 200).
Of course, this is the report of a single case and does not constitute reliable evidence for clinical practice. Nevertheless, it could add to the description of the symptoms and signs of WM combined with lung amyloidosis.
CONCLUSION
The rarity of the case reported here is the presentation of WM and lung amyloidosis on CT, which revealed a wide range of pulmonary lesions and a variety of morphological features. The physicians that may encounter the same kind, of course,will benefit from the option of differential diagnosis when they detect peculiar CT findings.
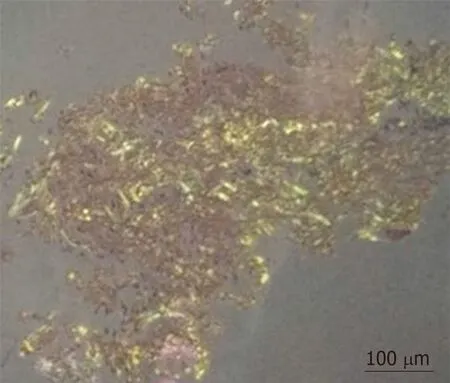
Figure 3 Evaluation of needle punch biopsy specimens under a polarizing microscope after Congo red staining showing a typical “apple-green birefringence” of Congo red-stained amyloid (magnification, × 100; U-POT, lens type; Olympus, Tokyo, Japan).

Figure 4 Evaluation of needle punch biopsy specimens by hematoxylin-eosin staining. The specimens were fixed in 10% formaldehyde solution for 6 h,followed by dehydration, clearing, waxing, and sectioning for 4-μm sections. The sections were stained with hematoxylin-eosin and then observed under a light microscope (BX40, Olympus). A large amount of amyloid-like deposition was detected under alveolar epithelial cells (magnification, × 200).
 World Journal of Clinical Cases2020年11期
World Journal of Clinical Cases2020年11期
- World Journal of Clinical Cases的其它文章
- Macrophage activation syndrome as an initial presentation of systemic lupus erythematosus
- Optical coherence tomography guided treatment avoids stenting in an antiphospholipid syndrome patient: A case report
- Uterine incision dehiscence 3 mo after cesarean section causing massive bleeding: A case report
- Ataxia-telangiectasia complicated with Hodgkin's lymphoma: A case report
- Gastric pyloric gland adenoma resembling a submucosal tumor: A case report
- Reduced delay in diagnosis of odontogenic keratocysts with malignant transformation: A case report
