Primary intestinal extranodal natural killer/T-cell lymphoma,nasal type:A case report
Bao-Long Dong,Xiao-Hua Dong,Hui-Qi Zhao,Peng Gao,Xiao-Jun Yang
Bao-Long Dong,Xiao-Hua Dong,Hui-Qi Zhao,Peng Gao,Xiao-Jun Yang,Department of General Surgery,Gansu Provincial Hospital,Lanzhou 730000,Gansu Province,China
Abstract
Key words: Primary intestinal extranodal natural killer/T-cell lymphoma;Multidisciplinary team discussion;Rare disease;Case report
INTRODUCTION
Primary intestinal extranodal natural killer/T-cell lymphoma,nasal type (PIENKTCL) is a rare non-Hodgkin's lymphoma (NHL) subtype,accounting for 3.1% of cases,and its prognosis is extremely poor[1].As only a few cases have been reported and the majority have been in the form of national and international case reports and case reviews,there is no unified treatment regimen;moreover,knowledge of the clinical characteristics of this disease is limited.This poses a challenge for early diagnosis,which may be one of the key reasons for delayed diagnosis and poor prognosis[2].Herein,we report a patient with PI-ENKTCL who was treated at our hospital in January 2019.By combining this report with national and international literature,we analyzed the clinicopathological and immunological characteristics of PI-ENKTCL to improve awareness of this tumor type and to provide a reference for accurate early diagnosis and treatment.
CASE PRESENTATION
General information
The patient was a 45-year-old man who was referred to our department in January 2019 due to intermittent hematochezia for 20 days and recurrence and exacerbation for 1 d.Twenty days prior to referral,he experienced intermittent hematochezia,with a high volume of blood,for no apparent reason,which spontaneously stopped without treatment.He sought medical attention at our gastroenterology department where gastroscopy,colonoscopy,biopsy and abdominal computed tomography (CT)were performed.Pathology showed the following results:“superficial gastritis (Figure 1A and B),(transverse colon) necrosis,inflammatory exudates,and granulomatous tissue” (Figure 1C and D).Abdominal CT showed local intestinal wall changes at the descending colon,and he was diagnosed with gastrointestinal bleeding (unknown cause).One day prior to referral,the patient experienced large volume hematochezia and was transferred to our department to determine the etiology of bleeding.Hemostasis,supplementation of blood volume,and other symptomatic treatments were performed.Relevant examinations were conducted to obtain a definitive diagnosis and for further treatment measures.
Physical examination
The patient's vital signs were as follow:Temperature:36.5°C,pulse rate:78 bpm,respiratory rate:19 breaths/min,and blood pressure:108/56 mmHg.Physical examination showed the following:Anemic countenance;absence of superficial lymph node enlargement and heart abnormalities;abdomen flat;liver and spleen not palpated below the costal margin;hypogastric region tenderness present;shifting dullness absent;borborygmus of 5 times/min,with no increase or decrease;and gurgles and abdominal vascular murmurs not audible.
Laboratory tests
Laboratory tests showed the following results:White blood cell count:7.1 × 109/L;red blood cell count:2.91 × 1012/L;hemoglobin:86 g/L;platelet count:223 × 109/L;liver and kidney function normal;lactate dehydrogenase (LDH):643 U/L;prothrombin time:16.5 s;fibrinogen:4.14 g/L;erythrocyte sedimentation rate:84 mm/h;tumor marker CA-125:96.90 U/mL (normal < 35 U/mL);remaining parameters,normal range;anti-Epstein-Barr virus (EBV) capsid antigen IgG,positive;tuberculosis antibodies and tubercle specific immune responses,negative;and immune function,normal.
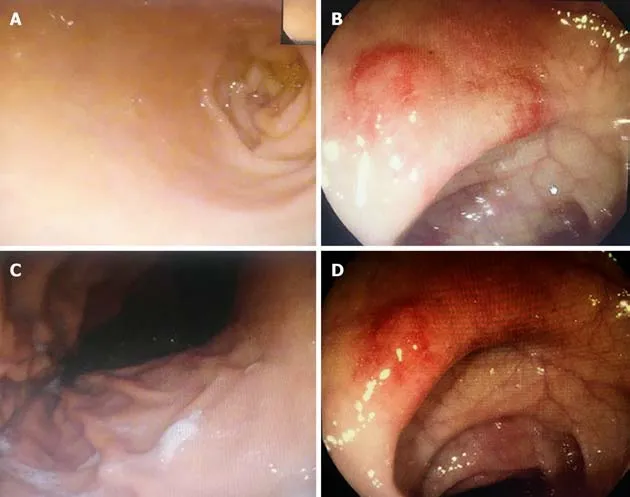
Figure1 Endoscopic appearances of the patient.
Imaging test
Abdominal CT showed local intestinal wall changes at the descending colon (Figure 2A).Digestive tract imaging showed local space-occupying lesion near the jejunum without obstruction (Figure 2B).Positron emission tomography (PET)-CT showed malignant small intestine lesions (suspected lymphoma),along with local lymph node metastases (Figure 2C,D).
Perioperative management
Two days before surgery,the patient was given liquid food.He fasted for 8 h before surgery,and 2 g of cefotiam was administered intravenously 30 min before surgery to prevent infection.After surgery,a patient-controlled analgesic pump was provided;hemostasis,electrocardiography,and nutrient,water,and electrolyte supplementation were performed.Routine blood and biochemical markers were monitored.
Surgery and outcomes
Following general anesthesia,the patient was placed in the supine position,followed by disinfection and trocar insertion.Examination found a 3 cm × 2 cm × 1 cm primary tumor in the jejunum 10 cm from the ligament of Treitz.The tumor had invaded the nearby descending colon to form a mass.The proximal jejunum 80 cm from the ligament of Treitz was dilated,and the distal small intestine was empty (Figure 3A).The surrounding organs were dissected,and the lesion-containing jejunum and descending colon were resected.A jejuno-jejunal anastomosis and an anastomosis between the residual ends of the descending colon were made.The surgery was successful,and the tumor was completely resected.The duration of surgery was 280 min,and intraoperative blood loss volume was 50 mL.Postoperative pathology tests showed that the resection margin was negative.No apparent surgical complications occurred after surgery and the patient was discharged 13 d after surgery.
Postoperative pathology tests
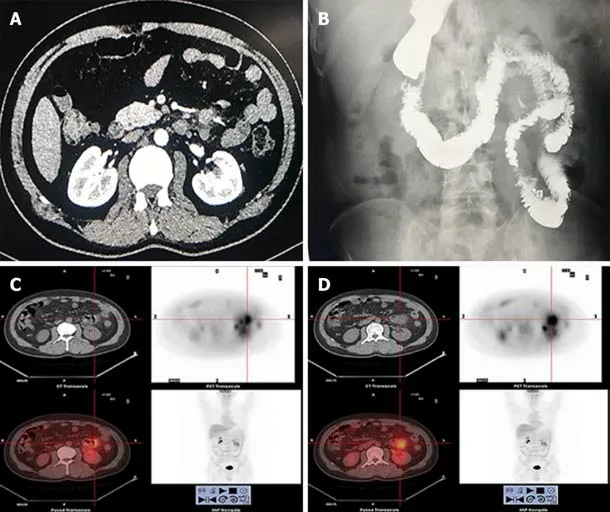
Figure2 Computed tomography,digestive tract imaging and positron emission tomography/computed tomography results.
The mucous membrane at the ulceration site had disappeared and was covered with necrosis,inflammatory exudates,and granulomatous tissues.The entire layer of the intestinal wall showed diffuse invasion by lymphocyte-like atypical cells,with the involvement of extraserosal adipose tissue.The nuclei of these cells were irregular,and distortions,lobules,and notches could be seen.These cells were rich in chromatin and granules and possessed visible nucleoli;mitotic figures were widely seen,with pink or clear abundant cytoplasm.The muscle layer at the intestinal wall showed widespread degeneration and necrosis (Figure 3B).Combined immunohistochemical staining of the small intestine specimens showed the following results:ENKTCL:1;CD3 (diffuse +):2;CD20 (+/-):3;TIA (+):4;Gr-B (partial+):5;CD56 (-):6;EMA (-):7;CD4 (diffuse +);8;CD8 (diffuse +):9;Perforin (focal +):10;CD38 (diffuse +):11;CD138 (diffuse +):12;CD79a (diffuse +):13;CD30 (-):14;ALK-D5F3 (-):15;CD45(diffuse +):16;Bcl-2 (diffuse +):17;Ki-67 index of 80%:18;andin situhybridoma with EBV RNA test (+) (Figure 4A and B).The final diagnosis was ENKTCL (Figure 4).
Postoperative treatment and follow-up
After surgery,the patient underwent a follow-up period of 6 mo and received 6 cycles of gemcitabine,oxaliplatin and L-asparaginase (L-GMOEX regimen),which was successful,and no apparent abnormalities were observed on relevant tests.PET-CT was performed at the 6-mo follow-up,and no recurrence or metastasis was observed(Figure 3C and D).Further follow-up is required to determine long-term efficacy and prognosis.
FINAL DIAGNOSIS
PI-ENKTCL.
TREATMENT
Surgery and systemic chemotherapy (L-GMOEX) was performed.
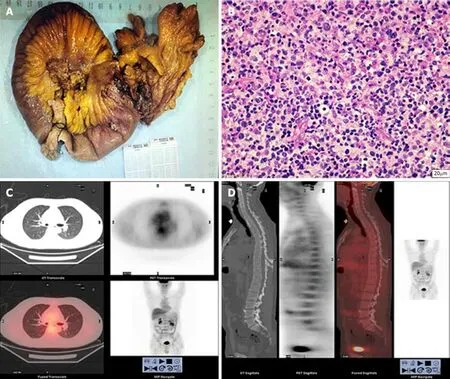
Figure3 Pathological test results and follow-up positron emission tomography/computed tomography results.
OUTCOME AND FOLLOW-UP
The patient underwent follow-up for 6 mo and received 6 cycles of gemcitabine,oxaliplatin and L-asparaginase.No recurrence or metastasis occurred.
DISCUSSION
Intestinal T-cell lymphoma and NK cell lymphoma are highly invasive and malignant tumors of the intestinal tract and account for 5.2% and 14.7% of primary lymphomas of the gastrointestinal tract,respectively[3].PI-ENKTCL is rare and accounts for 3.1%of NHL in Europe and North America.However,it is more common in Asia and South America[4].We performed a literature review and found that PI-ENKTCL tends to occur in middle-aged males around the age of 40 years and has a poorer prognosis than intestinal T-cell lymphoma or NK cell lymphoma[5].
Kimet al[6]reported that PI-ENKTCL mainly affects the small intestine,particularly the ileum and jejunum.This is different from B-cell lymphoma that usually affects the stomach,terminal ileum,and the cecum.Most PI-ENKTCL lesions do not have specific clinical presentations or endoscopic characteristics.The early symptoms of PIENKTCL are similar to gastrointestinal tuberculosis and Crohn's disease,with highly similar endoscopic findings;the biopsy positivity rate is low[7-9].Therefore,the misdiagnosis rate is high.PI-ENKTCL often results in bleeding,perforation,and other complications.Surgical resection of the primary tumor is mainly performed for diagnosis and treatment.There are slight differences in the factors that affect PIENKTCL prognosis,according to different studies.These factors generally include age,LDH levels,lymph node metastasis,clinical stage,and myelosuppression[10].Currently,there are no unified prognostic factors.
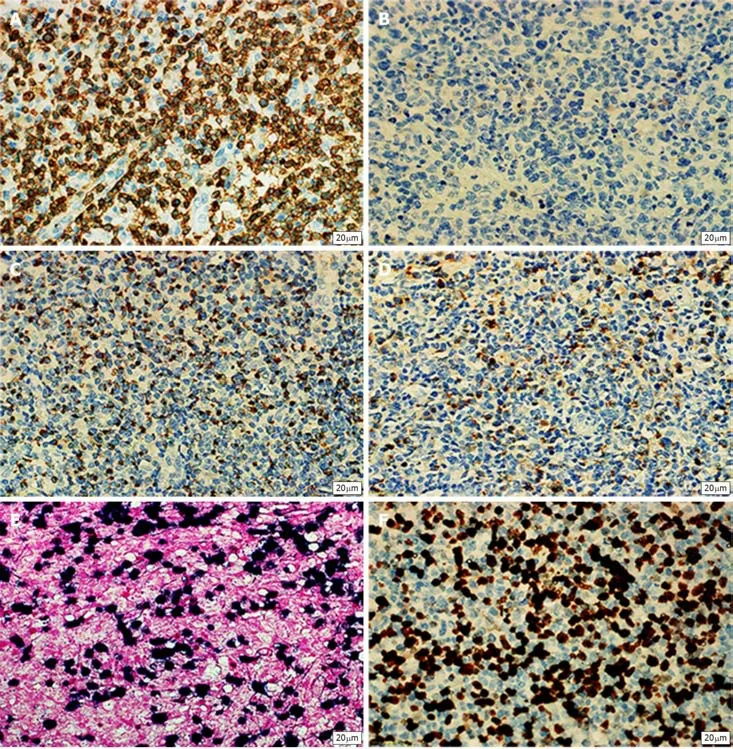
Figure4 Immunophenotypic analysis of the tumor.
PI-ENKTCL does not show a specific endoscopic presentation,with deep lymphoma lesions and a large amount of necrotic tissue at the surface.Therefore,it is usually difficult to diagnose PI-ENKTCL by biopsy[11].Other diagnostic imaging methods do not show significant advantages in PI-ENKTCL.In addition,PI-ENKTCL laboratory tests are often accompanied by EBV infection and LDH elevation.Therefore,it is necessary to test for EBV and LDH when PI-ENKTCL is suspected.According to our literature review,when the diagnosis of PI-ENKTCL is suspected,PET-CT is needed for diagnosis and to exclude primary tumors of the nasal cavity.In addition,differences in intake values can be used for differential diagnosis and can have clinical significance in guiding clinical stage,treatment,and diagnosis[12,13].
PI-ENKTCL has histological characteristics similar to those of ENKTCL at other sites and often presents with invasion of blood vessel centers,expression of cytotoxic proteins (granzyme B and TIA-1),and significant necrosis[14].Immunophenotypic characteristics include positivity for CD2,CD3,CD43,CD56,and cytotoxic factors(granzyme B and TIA-1).EBV and cytotoxic factor positivity are the key to diagnosis[15].A unique case involving CD56 negativity was reported,but a definitive diagnosis can be achieved when at least one cytotoxic factor and EBV are positive[16].
As PI-ENKTCL is rare and there is a lack of clinical tissue heterogeneity,there is currently no confirmed,optimal first-line treatment regimen.In addition,it is difficult to diagnose PI-ENKTCL,particularly those that occur in the small intestine,and PIENKTCL tends to result in complications such as obstruction,perforation,and bleeding.Therefore,early surgical resection is beneficial[17].Some studies also found that the occurrence of complications is one of the factors that directly affect prognosis[5].In addition,combined chemotherapy is more beneficial than surgery alone for patients that fulfill the criteria for surgery[6,18].Currently,there is no standard chemotherapy regimen for PI-ENKTCL.The chemotherapy regimen for PI-ENKTCL is similar to that for ENKTCL.Many previous clinical studies have used CHOP or SMILE as first-line chemotherapy regimens,and these regimens have fair efficacy considering drug resistance[1].Recently,the chemotherapy regimen of L-asparaginase combined with GMOEX has shown good therapeutic efficacy[19].Due to the popularity of immunotherapy,the use of the programmed death ligand 1 (PD-L1) inhibitor pembrolizumab has given new hope to ENKTCL patients.ENKTCL cells express PDL1,which binds to PD-1 on the surface of T-cells infiltrating the tumor microenvironment to inhibit tumor-specific T-cell activity or inactivate T-cells to block immune responses and to enable immune evasion in tumor cells[20,21].Therefore,overcoming this immune evasion mechanism and increasing T-cell activity will increase immunotherapy effects.
CONCLUSION
PI-ENKTCL has a low incidence,high invasiveness,and lacks specific clinical presentation,which makes it prone to misdiagnosis.This delays treatment and affects prognosis.Therefore,for suspected PI-ENKTCL patients,PET-CT and tests for EBV and LDH can provide a definitive diagnosis or diagnosis of exclusion,leading to multidisciplinary-assisted diagnosis and treatment.Surgery should be the mainstay of treatment for patients with no metastasis or surgical contraindications.Appropriate chemotherapy should be administered based on postoperative pathology results to improve the survival and prognosis of patients.
 World Journal of Clinical Cases2020年1期
World Journal of Clinical Cases2020年1期
- World Journal of Clinical Cases的其它文章
- Cluster headache as a manifestation of a stroke-like episode in a carrier of the MT-ND3 variant m.10158T>C
- Six families with balanced chromosome translocation associated with reproductive risks in Hainan Province:Case reports and review of the literature
- Clinical characteristics on manifestation and gene mutation of a transient neonatal cyanosis:A case report
- Sarcomatoid intrahepatic cholangiocarcinoma mimicking liver abscess:A case report
- Value of dynamic plasma cell-free DNA monitoring in septic shock syndrome:A case report
- Unusual presentation of bladder neuroblastoma in a child:A case report
