抗生素降階梯治療慢性阻塞性肺疾病合并重癥肺炎效果分析
翟溶凡 蔣先訓
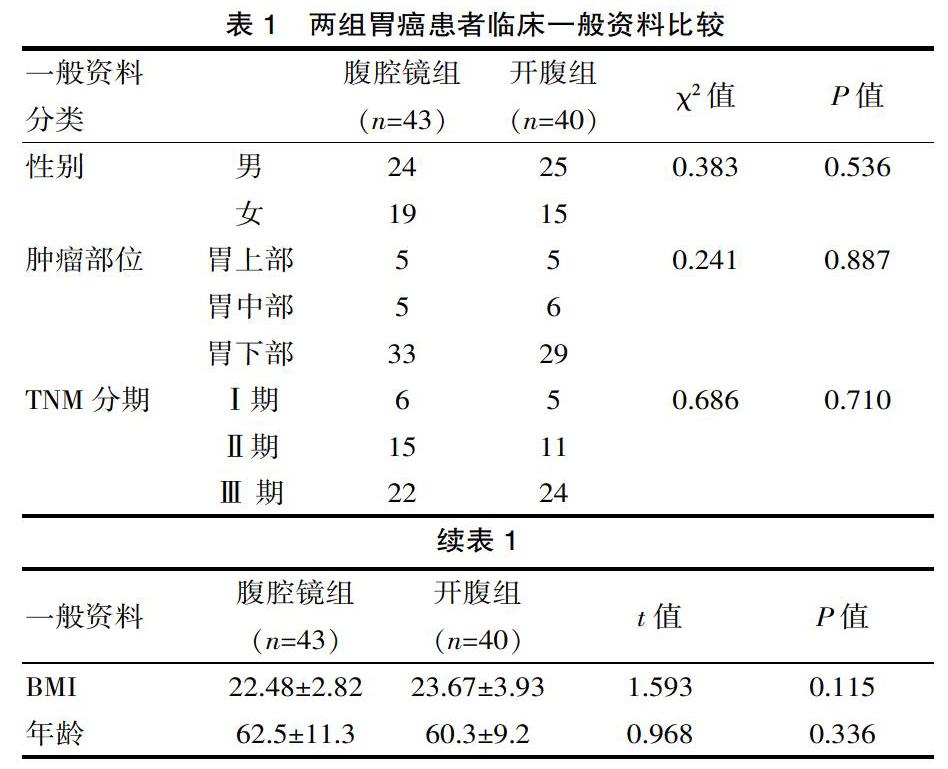
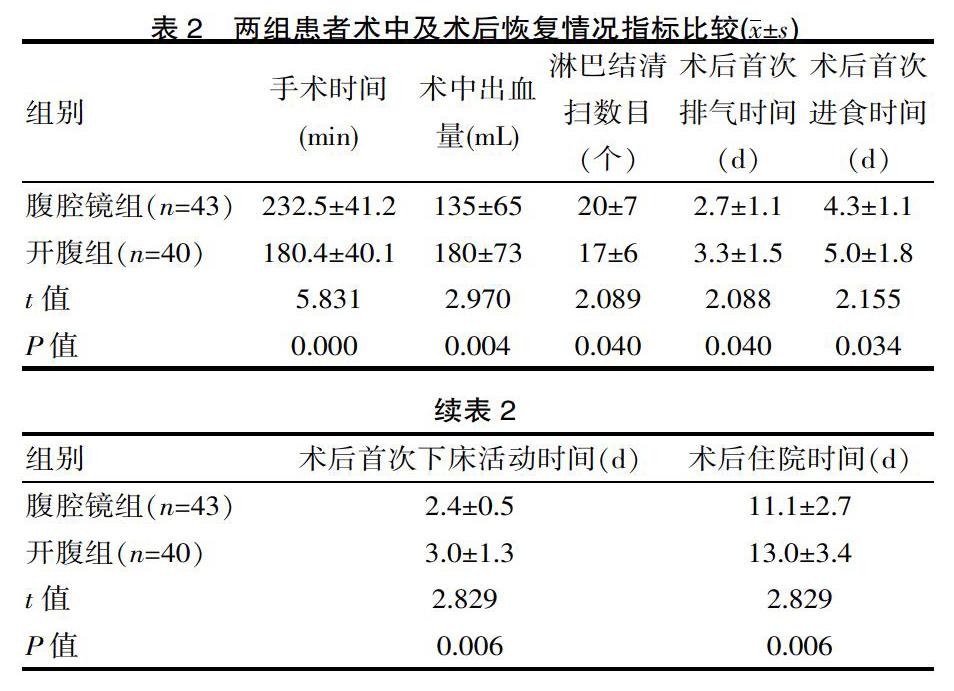
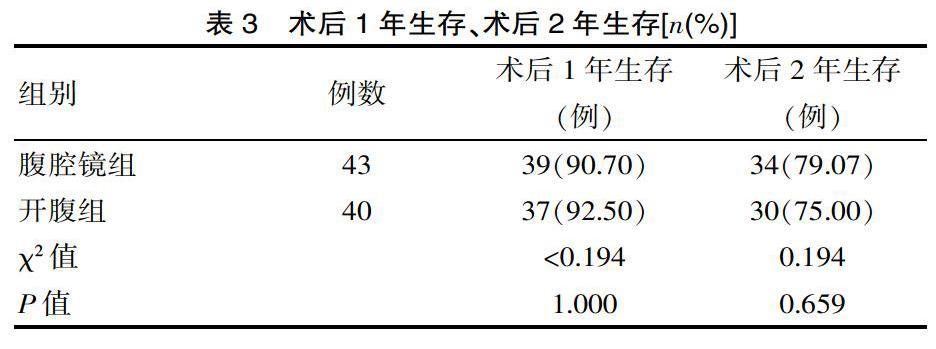
[摘要] 目的 探討比較胃癌在腹腔鏡手術與開腹手術中的療效。 方法 采用回顧性隊列研究方法。整理了2011年1月—2017年4月該院收治的83例胃癌患者,其中腹腔鏡組43例,開腹組40例。腹腔鏡組平均年齡:﹙62.5±11.3﹚歲,開腹組平均年齡:(60.3±9.2)歲,觀察指標:①臨床資料;②術中術后情況:手術時間,術中出血量,淋巴結清掃數目,術后首次排氣時間,術后首次進食時間,術后首次下床活動時間,術后住院時間,術后1年生存,術后2年生存;③術后并發癥:切口感染,肺部感染,腹腔感染,腹腔出血,吻合口瘺,十二指腸殘端瘺,胃癱。 結果 ①臨床資料比較:二者在性別、年齡、BMI、腫瘤部位、腫瘤分期方面,均差異無統計學意義(P>0.05)。②術中術后情況:術中出血量(135±65)mL、術后首次排氣時間(2.7±1.1)d、術后首次進食時間(4.3±1.1)d、術后首次下床活動時間(2.4±0.5)d、術后住院時間(11.1±2.7)d腹腔鏡組指標均優于開腹組,差異有統計學意義(t=2.970,2.088,2.155,2.829,0.194,P=0.004,0.040,0.034,0.006,0.659)。手術時間腹腔鏡組(232.5±41.2)min長于開腹組(180.4±40.1)min,差異有統計學意義(t=5.831,P=0.000),術后1年、2年生存時間差異無統計學意義(P>0.05)。③術后并發癥:二者術后并發癥(切口感染,肺部感染,腹腔感染,腹腔出血,吻合口瘺,十二指腸殘端瘺,胃癱)總數比較差異無統計學意義(P>0.05)。 結論 通過臨床對比研究,腹腔鏡手術治療胃癌相對于開腹手術治療胃癌,雖然手術時間長于開腹組,但具有術中出血少、淋巴結清掃數目多、術后胃腸功能恢復快、早期進食、下床活動、住院時間短等優點,同時在術后1年、2年生存期及術后并發癥方面無統計學差別,是損傷小,恢復快,安全可靠的術式,可以在臨床推廣發展。
[關鍵詞] 胃癌;腹腔鏡;開腹;療效
[中圖分類號] R735? ? ? ? ? [文獻標識碼] A? ? ? ? ? [文章編號] 1674-0742(2019)12(a)-0015-04
[Abstract] Objective To investigate the efficacy of gastric cancer in laparoscopic surgery and open surgery. Methods A retrospective cohort study approach was used. 83 patients with gastric cancer admitted to our department from January 2011 to April 2017 were enrolled, including 43 in the laparoscopic group and 40 in the open group. The average age of the laparoscopic group was (62.5±11.3)years, and the average age of the open group was (60.3±9.2)years. Observed indicators: 1.clinical data;2.intraoperative and postoperative conditions: operation time, intraoperative blood loss, lymph node dissection number, first postoperative exhaust time, first postoperative feeding time, first time to get out of bed after surgery, postoperative hospital stay, 1 year postoperative survival, 2 years postoperative survival;3.postoperative complications: incision infection , pulmonary infection, abdominal infection, abdominal bleeding, anastomotic leakage, duodenal stump fistula, stomach cramps. Results 1.Comparison of clinical data: There was no significant difference in gender, age, BMI, tumor location and tumor stage (P>0.05). 2.Intraoperative and postoperative conditions: intraoperative blood loss (135±65)mL, first exhaust time after surgery (2.7±1.1)d, first time after surgery (4.3±1.1)d, first time after going to bed time (2.4±0.5)d and postoperative hospital stay (11.1±2.7)d were better than the open group in the laparoscopic group , the difference was statistically significant(t=2.970, 2.088, 2.155, 2.812, P=0.004, 0.040, 0.034, 0.006). The laparoscopic group (232.5±41.2)min was longer than the open group (180.4±40.1)min, and there was a statistical difference (t=5.831, P=0.000). There was no significant difference in 1-year and 2-year survival time after surgery(P>0.05). 3.Postoperative complications: there was no statistically significant difference in the total number of postoperative complications (incision infection, pulmonary infection, abdominal infection, abdominal hemorrhage, anastomotic leakage, duodenal stump fistula, stomach cramps(P>0.05). Conclusion Through clinical comparative study, laparoscopic surgery for gastric cancer compared with open surgery for gastric cancer, although the operation time is longer than the open group, but with less intraoperative bleeding, more lymph node dissection, postoperative gastrointestinal function recovery, early eating, getting out of bed, short hospital stay, etc., and no statistical difference in 1-year, 2-year survival and postoperative complications are small, quick recovery, safe and reliable, and can be promoted in clinical practice and development.
綜上所述,與傳統開腹治療胃癌手術相比效,腹腔鏡胃癌根治術是術中損傷更小,術后恢復更快,安全有效的手術方式,值得推廣應用。雖然目前在進展期胃癌中腹腔鏡手術仍然存在著一定爭議,但隨著腹腔鏡器械、設備的完善成熟、腹腔鏡在多學科的廣泛開展、長期的多中心大樣本隨機對照試驗的進一步驗證,我相信腹腔鏡在胃癌手術方面的優勢將更加顯著,它將與傳統開腹手術長期并存。
[參考文獻]
[1]? Siegel RL,Miller KD,Jemal A.Cancer statistics,2018 [J].CA Cancer J Clin,2018,68(1):7-30.
[2]? 國家消化系疾病醫學研究中心,中華醫學會消化內鏡學分會,中華醫學會健康管理學分會,等.中國早期胃癌篩查流程專家共識意見(草案,2017年,上海)[J].中華消化雜志,2018,38(2):87-92.
[3]? 蔡慧,徐光寰,王玨.上海市原盧灣區2004-2011年消化系統常見腫瘤的發病和死亡趨勢分析[J].中國臨床醫學,2018, 25(4): 542-548.
[4]? 中國醫師協會內鏡醫師分會腹腔鏡外科專業委員會,中國研究型醫院學會機器人與腹腔鏡外科專業委員會,中國腹腔鏡胃腸外科研究組.中國腹腔鏡胃癌根治手術質量控制專家共識(2017版) [J]. 中華消化外科雜志,2017,16(6):539-547.
[5]? 邢亞峰.阿帕替尼聯合希羅達治療晚期胃部的臨床療效觀察[J].臨床醫學進展,2018,8(9):855-860.
[6]? 董朋朋,張紅軍 .晚期胃癌免疫治療研究進展[J].養生保健指南,2019(21):203.
[7]? 梁良.調強放療和同步化療用于進展期胃癌治療中的臨床效果[J].中國社區醫師,2019(3):53-56.
[8]? 胡建昆,張維漢,陳心足.從中國CLASS-03a研究的開展看腹腔鏡手術聯合新輔助化療的胃癌治療[J].中華胃腸外科雜志,2018(2):138-142.
[9]? Kitano S, Iso Y, Moriyama M, et al. Laparoscopy-assistedBillrothI gastrectomy[J].Surg Laparosc Endosc,1994,4(2):146-148.
[10]? 日本胃癌學會 胃癌處理規約[M]. 東京:金原出版株式會社,2017.
[11]? Lin JX, Huang CM, Zheng CH, et al. Is All Advanced Gastric Cancer Suitable for Laparoscopy-Assisted Gastrectomy With Extended Lymphadenectomy A Case-Control Study Using a Propensity Score Method[J]. Ann Surg Oncol,2016,23(4):1252-1260.
[12]? Chen QY, Zheng CH, Li P, et al. Which method is more suitable for advanced gastric cancer with enlarged lymph nodes, laparoscopic radical gastrectomy or open gastrectomy[J].Gastric Cancer,2018,21(5):853-863.
[13]? 張軍永,邢攸軒.腹腔鏡遠端胃癌根治與開腹對早期胃癌的影響[J].中國繼續醫學教育,2018, 10(36): 62-64.
[14]? 李國新,胡彥鋒,劉浩.中國腹腔鏡胃腸外科研究組CLASS-01研究進展[J].中華消化外科雜志,2017,16(1):38-42.
[15]? Lee HJ, Hyung WJ, Yang HK, et al. Morbidity of laparoscopic distal gastrectomy with D2 lymphadenectomy compared with open distal gastrectomy for locally advanced gastric cancer: Short term outcomes from multicenter randomized controlled trial(KLASS-02)[J].J Clin Oncol,2016,34:abstr 4062.
[16]? ?Park YS, Son SY, et al. Eleven-year experience with 3000 cases of laparoscopic gastric cancer surgery in a single institution: analysis of postoperative morbidities and long-term oncologic outcomes[J]. Surg Endosc,2016,30(9):3965-3975.
[17]? Xu Y, Hua J, Li J, et al. Laparoscopic versus open gastrectomy for gastric cancer with serous invasion: long-term outcomes[J].J Surg Res,2017,215:190-195.
[18]? 顏宏銳,朱煥明.胃腸外科腹腔鏡技術在基層醫院“復制”的學習曲線 [J].系統醫學,2018(5):98-100.
[19]? ?黃昌明,林建賢.腹腔鏡胃癌根治術淋巴結清掃中團隊配合的策略與技巧[J].中華消化外科雜志,2019,18(3):209-212.
[20]? 錢俊甫,李書旺,牛國浩. 腹腔鏡下不同淋巴結清掃方案對1-3期胃癌手術臨床指標及術后并發癥的影響[J]. 2019,34(1):57-60.
[21]? ?高增戰,李樹營 .胃癌D2 根治術采用腹腔鏡與傳統開腹術治療進展期胃癌的療效對比 [J].中華普外科手術學雜志:電子版,2018,12(6):520-522.
(收稿日期:2019-08-10)

