Intracranial hematoma development following thrombolysis inpatients suffering with acute myocardial infarction: Management strategy
Luis Rafael Moscote Salazar, Amit Agrawal, Guru Dutta Satyarthee, George Chater Cure,Alfonso Pacheco-Hernandez
1Universidad de Cartagena, Cartagena de Indias, Colombia
2Department of Neurosurgery, Narayna Medical College Hospital, Chinthareddypalem, Nellore-524003, Andhra Pradesh, India
3All India Institute of Medical Sciences, New Delhi, India
4Clinica General de Norte, Barranquilla, Colombia
Keywords:Acute myocardial infarction Thrombolysis Intracranial hematoma Management Outcome
ABSTRACT Intracerebral hemorrhage secondary to thrombolysis in patients with acute myocardial infarction is a catastrophic condition. Several factors predispose to intracranial bleeding including low body weight, female sex, advanced age, use of oral anticoagulants prior to the administration of fibrinolytic therapy, diastolic blood pressure (greater than 110 mm Hg),among others. Optimal medical management involves multidisciplinary roles of hematology,neurosurgery and critical medicine. In this illustrative case, a classification and management algorithm were proposed for patients with complications hemorrhage associated with thrombolysis after myocardial infarction.
1. Introduction
Acute myocardial infarction is considered as a major cause of mortality. The current usage of therapeutic strategies including thrombolysis for management in the acute phase can result in serious complications[1-5]. After the confirmation of the diagnosis of acute myocardial infarction, the proposed management options must take consideration of individual cases and must also take into account of the absolute and relative contraindications of initial and follow-up for thrombolytic therapy. Intracerebral hemorrhage accounts for 10%-15% of all intracranial vascular events in the general population. A number of risk factors for haemorrhagic stroke are advanced age, hypertension, trauma, vascular malformations,and anticoagulant threrapy. Following the use of thrombolytic therapy in patients suffering with acute myocardial infarction, at least half of the vascular events are related to the hemorrhagic manifestation[6-14]. This paper briefly reviews current status of various management options for therapy of intracranial hemorrhage after thrombolysis in acute myocardial infarction.
2. Case illustration
A 66-year-old man was admitted to critical patient unit with a history of suden chest pain. Evaluation at admission in the emergency department revealed an anxious elderly male had tachypnoea with respiratory rate at 26 per minute and vrest of physical examination did not find any abnormality. His peripheral pulses were normal.His electrocardiogram showed a ST-segment elevation and based on ECG finding, a diagnosis of acute myocradial infaerction was made and planned for emergency thrombolysis therapy. He underwent thrombolysis therapy with 10 000 IU of tenecteplase and then transferred to an intensive care unit for hemodynamic surveillance.Six hours after the thrombolysis therapy, the patient noticed acute difficulty in speech and right side hemiparesis. Cranial noncontrast CT scan was performed, which revealed presence of intracerebral and ventricular hemorrhage (Figure 1). Fresh plasma was transfused and he was evaluated by neurosurgery. He also underwent external ventricular drainage and kept for seven days. The patient was slowly showing recovery of speech with mild hemiparesis. He was discharged from hospital twenty days after admission.
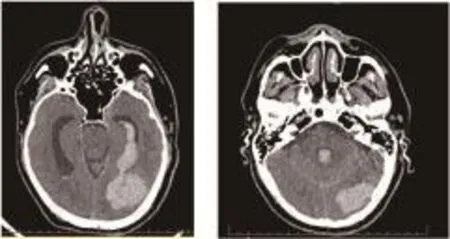
Figure 1. Brain CT showing intracerebral hemorraghe after thrombolysis in a patient with myocardial infarction.
3. Discussion
The use of thrombolytic therapy has shown to limit the size of infarct with preservation of left ventricular function and decrease mortality after an acute myocardial infarction. Risk of thrombolytic therapy commonly include intracranial hemorrhage following thrombolysis in acute myocardial infarction, occurs in about 0.9%-1.0% of cases and is considered as an emergency condition due to its high mortality. The diagnosis of post-thrombolytic haemorrhage in acute myocardial infarction should be considered in any patient who has a focal or sensory neurological deficit after thrombolysis[15].Its early recognition is essential to establish strategies that allow limiting the evolution of the disease. A study involving 1 696 patients described tomographic patterns in patients with myocardial infarction, who also underwent pharmacological thrombolysis,the most frequent site was supratentorial and intraparenchymal,and 84% of the symptoms occurred within the first 24 hours of therapy[6]. Al Khuwaitir et al reported the case of a 40-year-old male who underwent surgical evacuation of a right temporoparietal hematoma after thrombolysis with streptokinase[16]. Although the place of bleeding following thrombosis is the gastrointestinal tract,neurosurgeons should be vigilent before any neurological deficits.
Thrombolytic therapy improves coronary blood flow by the activation of plasmin and the enzyme responsible for fibrin degradation. The most commonly used pharmacological agents are: streptokinase and recombinant plasminogen activatoralteplase, reteplase and tenecteplase. It has been postulated that the development of bleeding areas requires the loss of vascular integrity,dissolution of hemostatic plugs and the depletion of coagulation factors. Intracranial hematomas with large volumes have been associated with higher mortality. Authors proposed a classification of intracranial hemorrhage following thrombolysis in acute myocardial infarction based on the various hemorrhagic patterns. Type Ⅰ:Supratentorial hemorrhage without hydrocephalus; Type Ⅱ:Supratentorial multiple hemorrhage without hydrocephalus; Type Ⅲ:Supratentorial hemorrhage with hydrocephalus; Type Ⅳ: Cerebellar hemorrhage with/without hydrocephalus.
The development of an organized approach is crucial for evaluation and treatment of post-thrombolysis intracerebral hemorrhage in myocardial infarction (Figure 2). It is important to emphasize that the algorithm is intended to guide management of post-thrombolysis intracerebral hemorrhage in myocardial infarction. The clinical judgment will be fundamental in the management. Variations in clinical resources available locally will also influence the management. The guidelines of neurocritical care society (2015) for Reversal of Antithrombotics in Intracranial Hemorrhage provided recommendations for thrombolytic reversal: i. To discontinue thrombolytic agents when intracranial hemorrhage is present or suspected (good practice statement), ii. To use cryoprecipitate(10 units initial dose) in patients with thrombolytic agent-related symptomatic intracranial hemorrhage, who received a thrombolytic agent in the previous 24 hours. (Conditional recommendation,low-quality evidence), iii. In cases where cryoprecipitate is contraindicated or not available in a timely manner, we suggest use an antifibrinolytic agent (tranexamic acid 10-15 mg/kg intravenous over 20 min or e-aminocaproic acid 4-5 g intravenous) as an alternative to cryoprecipitate (conditional recommendation, very low-quality evidence). iv. Checking serum fibrinogen levels after administration of reversal agents. If the serum fibrinogen level is less than 150 mg/dL, administration of additional cryoprecipitate(Conditional recommendation, very low-quality evidence). v. It is unclear if platelet transfusion is useful and we cannot offer a recommendation at this time.
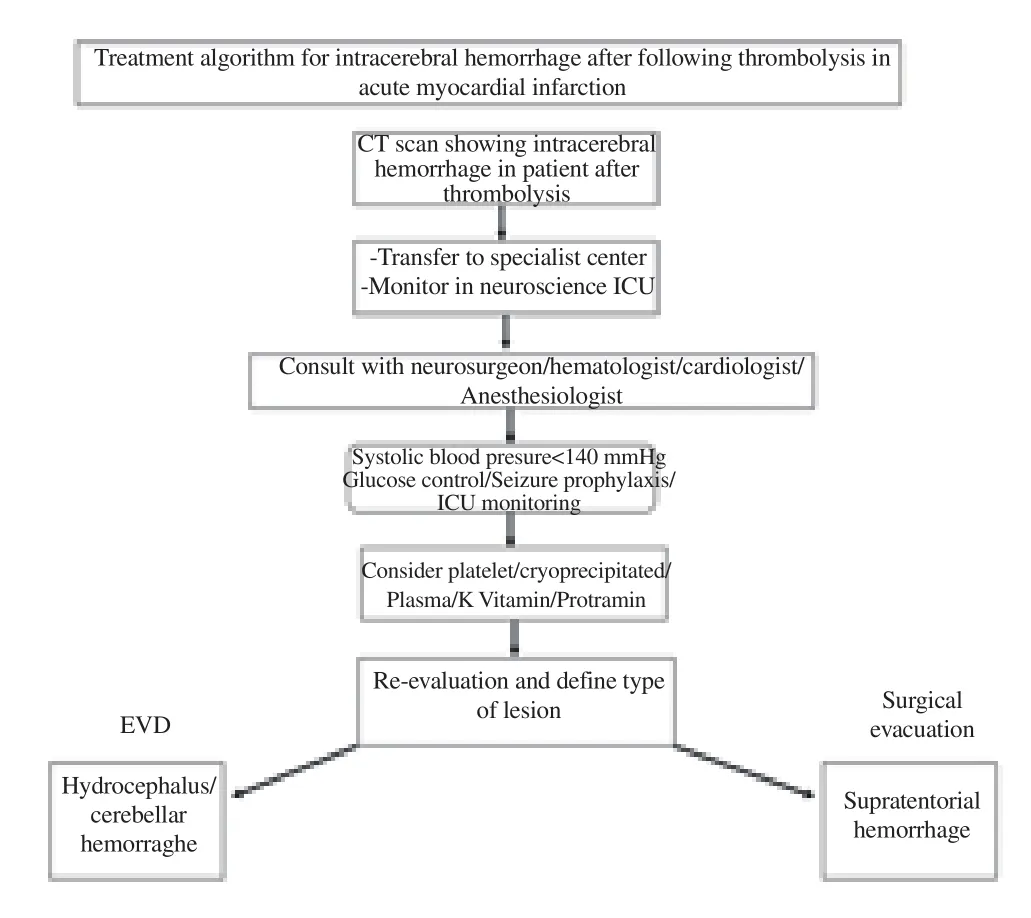
Figure 2. Algorithm for treatment of intracerebral hemorrhage after following post-thrombolysis.
The development of intracerebral hemorrhage following thrombolytic therapy carry a poor prognosis with about 62%mortality during hospitalization. The application of our proposed classification and management algorithm will contribute to better management of patients with this catastrophic pathology.Although there is a lack of enough evidence for recommendation of cryoprecipitate use, we observed improved outcome following administration of fresh frozen plasma.
Conflict of interest statement
The authors declare no conflict of interest.
 Journal of Acute Disease2018年5期
Journal of Acute Disease2018年5期
- Journal of Acute Disease的其它文章
- CORRIGENDUM
- False negative diffusion weighted imaging in an acute onset double vision patient with isolated internuclear ophthalmoplegia from ischemic origin
- A case of human acute otoacariasis caused by Rhizoglyphus sp, the first report from Iran
- Think muscle; Think rhabdomyolysis
- Survival rate among tuberculosis patients identified in south of Iran,2005-2016
- Inhibiting effect of immunoeffector cells induced by denderitic cells vaccine on growth of PC3 and BEL7402
