The laparoscopic approach in emergency surgery: A review of the literature
Ionut Negoi, Mircea Beuran, Cezar Ciubotaru, Adelina Cruceru, Sorin Hostiuc, Massimo Sartelli, Matthew Hernandez, Mihaela Vartic
1Carol Davila University of Medicine and Pharmacy Bucharest, Romania
2Emergency Hospital of Bucharest, Romania
3Department of Legal Medicine and Bioethics, National Institute of Legal Medicine Mina Minovici, Romania
4Department of Surgery, Macerata Hospital, Macerata, Italy
5Division of Trauma, Critical Care and General Surgery, Department of Surgery, Mayo Clinic, Rochester, MN, USA
1. Introduction
The role of laparoscopy in the acute care surgery had significantly increased during the latest years, both as a diagnostic and treatment method of all the upper or lower gastrointestinal pathologies[1].Nowadays, extensive surgical procedures are performed through a minimally invasive approach, and the current medical evidence confirms for laparoscopy that “you can resist an invading army, but not an idea whose time has come” said by Victor Hugo.
The objective of the present research is to review the current indications for laparoscopy in abdominal emergencies and to detail the benefits and complications associated with this approach.
2. Materials and methods
We have reviewed the relevant literature on the topic, using the PubMed/Medline and Web of Science Core Collection databases.We searched keywords in the title and abstract as the following combinations: laparoscopy OR minimally invasive surgery AND acute OR emergency OR cholecystitis OR appendicitis OR diverticulitis OR perforated ulcer OR bowel obstruction OR mesenteric ischemia OR trauma. We limited our search to papers published between January 2005 – and December 2017 (Figure 1).
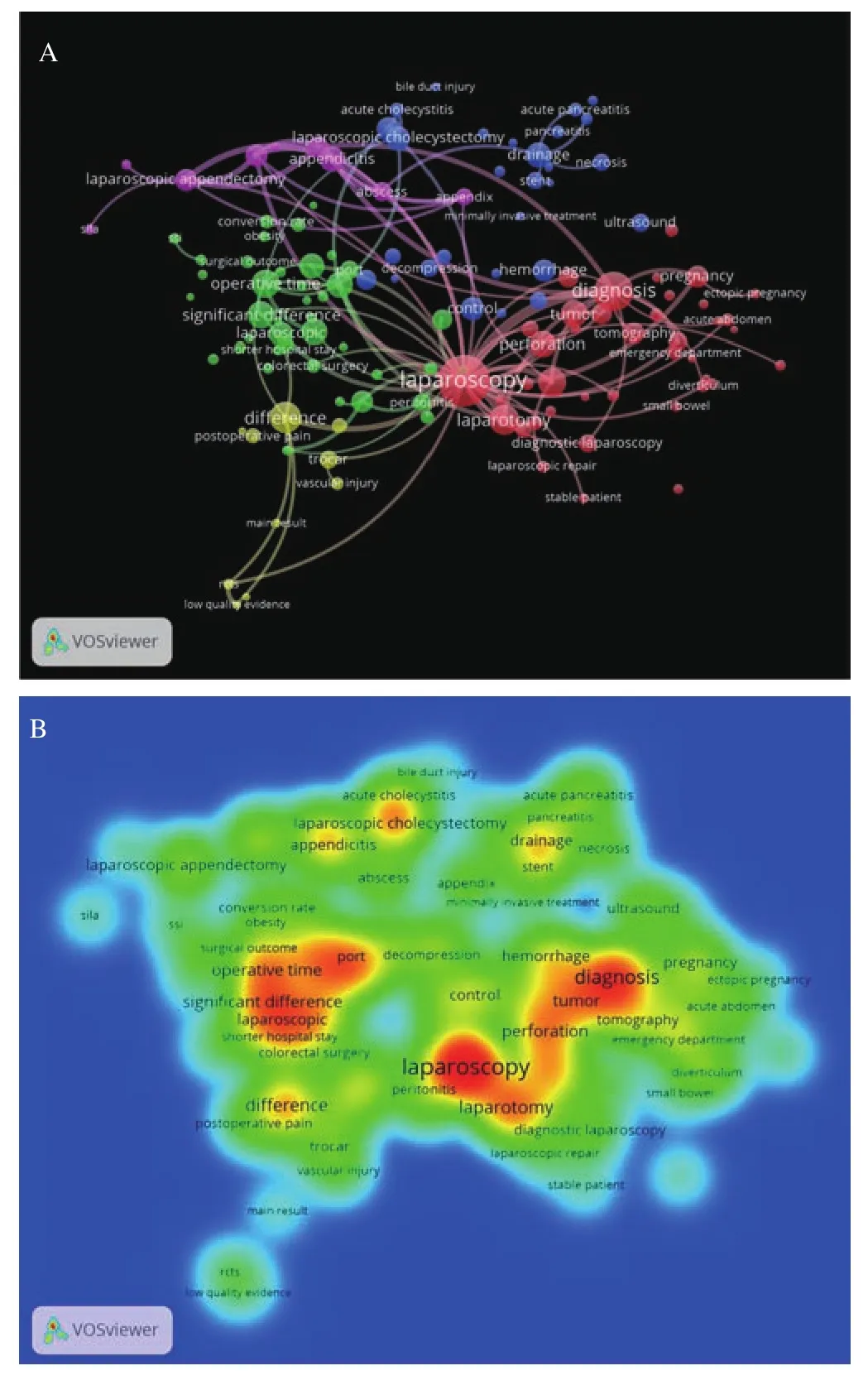
Figure 1. The network (A) and density (B) visualization syntax analysis of 10170 titles and abstracts published between 2005 and 2017, and indexed in Web of Science Core Collection using the following search strategy:((laparoscopy OR minimally invasive) AND (emergency OR acute OR cholecystitis OR appendicitis OR diverticulitis OR perforated peptic ulcer OR trauma OR injury)) (Analysis performed using the VOSviewer software).
3. Results
3.1. Acute cholecystitis
The gallbladder lithiasis is present in 10%-15% of the adult population, and 20% of them will develop acute cholecystitis. For diagnosis of acute cholecystitis, the positive Murphy sign along with leukocytosis and suggestive ultrasonography has a specificity and sensitivity of 62% and 74%, respectively. On the other hand,a suggestive ultrasonography only has a specificity of 81%[2]. The golden treatment of acute cholecystitis is represented by laparoscopic cholecystectomy. In 2013, Yonget al. presented a study of 316 patients with gallbladder preserving cholelithotomy[3]. Through a laparoscopic and choledocosopic guidance the authors had a success rate of 95%, with a recurrence of gallstones of 6.5% at 60 months[3].During the latest years, there were some controversies about when to operate acute cholecystitis. An increasing high-quality evidence supports the early cholecystectomy within 10 days from the onset of symptoms[4]. Soforet al. showed that laparoscopic cholecystectomy within two days from the onset of acute cholecystitis is associated with the best results and the lowest healthcare costs[5], while late cholecystectomy appears to be associated with an increase in postoperative complications and higher costs[4]. Sutcliffeet al.characterized the preoperative risk factors associated with conversion from laparoscopy to laparotomy. These risk factors were: increased age, male gender, acute cholecystitis and common bile duct stones,increased ASA class, thick gallbladder wall, and dilated common bile duct. A cutoff value of six for this score identified a conversion risk of 7.1%, compared with 1.2% in the general group[6].
The best moment to convert is not well defined by the medical literature. However, the Tokyo guideline recommends that surgeons should never hesitate to convert to open surgery, in order to prevent iatrogenic injuries, when they face difficulties in performing laparoscopic cholecystectomy[7]. The operating surgeon should strive for critical view of safety, popularized by Steven Strasberg[8].The Society of American Gastrointestinal and Endoscopic Surgeons(SAGES) have developed strategies to minimize the iatrogenic biliary tract lesions by adopting Universal Culture of Safety in Cholecystectomy[9].
In patients with severe inflammation and dense adhesions in the hepatoduodenal ligament, a subtotal cholecystectomy may be a viable option[10]. The subtotal cholecystectomy may be a subtotal reconstituting type (suturing the gallbladder infundibulum, which reduces the incidence of biliary fistula), or a subtotal fenestrating cholecystectomy (which abandons the gallbladder wall in contact with the cystic plate (with a higher incidence of postoperative biliary fistula, but no recurrent lithiasis)[10].
3.2. Acute appendicitis
Appendectomy represents the gold standard for acute appendicitis[11], and laparoscopy is recommended for all patients by the recent guidelines. The laparoscopic approach is associated with less postoperative pain, lower incidence of surgical site infections,decreased length of hospital stay, earlier return to work, and lower costs[12]. Laparoscopy should be preferred also in complicated disease and obese patients. There is no clear evidence for pregnant females, with disagreement in recommendations between European Association for Endoscopic Surgery and World Society of Emergency Surgery Guidelines[11,12].
Although early evidence showed a higher rate of intra-abdominal abscesses for laparoscopic group[13], a meta-analysis published in 2016 revealed that after the year 2001 the effect size in favor of open procedures began to disappear[14]. Analyzing all the available studies up to 2016, the intra-abdominal abscesses rate was similar between laparoscopic and open groups, with an overall cumulative odds ratio of 1.32 (P>0.05)[14].
During the latest years, the nonoperative treatment, with antibiotics,was proposed for uncomplicated acute appendicitis[15]. Kirbyet al.reported that for uncomplicated cases, appendectomy is associated with fewer complications compared to conservative treatment. Major post-intervention complications were 0.8% in appendectomy group and 10.1% in the antibiotic group[16].
3.3. Acute diverticulitis
Although seductive, according to increasing evidence, the laparoscopic peritoneal lavage and drainage should not be considered the treatment of choice in patients with perforated diverticulitis and generalized peritonitis. However, the emergency laparoscopic sigmoidectomy is feasible in selected patients with perforated acute diverticulitis, provided they are handled by experienced surgeons[17].Similar to other gastrointestinal resections, the laparoscopic sigmoidectomy is superior to open sigmoidectomy in terms of early postoperative outcomes[18].
The SCANDIV Randomized Clinical Trial showed a mortality at 90 days of 13.9% in the lavage group and of 11.5% in the resection group[19]. The reoperation rate was 20.3% and 5.7% in the lavage and resection group, respectively. There were no differences between the groups for the hospital stay and quality of life[19]. The LADIES trial, published in 2015, concluded that laparoscopic lavage is not superior to sigmoidectomy for the treatment of purulent perforated diverticulitis[20]. Cirocchiet al. showed in their meta-analysis that the laparoscopic lavage is associated with a statistically significant higher rate of postoperative intraabdominal abscesses. There were no differences regarding 30-day postoperative mortality and 30-day surgical reintervention rate. The laparoscopic group had a lower postoperative wound infection rate and a shorter length of hospital stay. The authors concluded that the laparoscopic lavage is not fundamentally inferior to surgical resection, and this technique may achieve reasonable outcomes with minimal invasiveness[21].
3.4. Perforated peptic ulcer
In patients with generalized peritonitis due to perforated peptic ulcer, the laparoscopy results are not clinically different from those of open surgery, although a decrease of septic abdominal complications were observed in minimally invasive group[22]. The main contraindication for a laparoscopic approach is the septic shock. As a surgical procedure to address the perforation, the primary repair should be performed in lesions smaller than two-centimeter diameter. The resection is indicated in patients with suspicion for malignancy, and in perforations larger than two-centimeter[23]. A multicenter retrospective study, which included 297 patients, showed that the laparoscopic approach for perforated peptic ulcer is feasible;the procedure is safe, with no increased risk of duodenal fistulae or residual intraperitoneal abscesses[24].
3.5. Small bowel obstruction
In the case of small bowel obstruction, Byrneet al. compared the outcomes of 83 patients operated by a laparoscopic approach with 163 patients in the open group[25]. In the multivariate analysis, the patients’age was the most reliable predictor for adverse outcomes (P= 0.003).The adjusted odds ratio for overall complications was 0.46, favoring the laparoscopic patients. The mean postoperative length of stay was also in favor of laparoscopic approach (3.8vs8.4 days)[25].
The predictive factors for a successful laparoscopic approach in patients with small bowel obstruction are: less than two previous laparotomies, pre-existent non-median laparotomy, appendectomy as suspected cause, a single band adhesion as the mechanism of obstruction, early management within 24 h, the absence of peritonitis on the physical examination and an experienced surgeon. Factors associated with failure of laparoscopic approach are the dilatation of the bowel loops more than four centimeters on abdominal computed tomography, severe associated morbidities, and hemodynamic instability[26].
3.6. Large bowel obstruction
Although the laparoscopic colorectal resections are predominant in elective patients, the minimally invasive approach is rarely used in the case of large bowel obstruction. To improve perioperative outcomes and to avoid an emergency laparotomy, colonic selfexpanding metal stents followed by minimally elective resection is increasingly used in cases of large bowel obstruction.
Gashet al. analyzed their outcomes with laparoscopic management of large bowel obstruction, including 45 patients in 8 years[27].There were twenty-one operations for colonic cancer, ten lower anterior resections, six Hartmann’s, seven right hemicolectomies and one total colectomy. The postoperative complications included two cases of atrial fibrillation, two wound infections, two cases of ileus, one case of CO2retention, one stoma necrosis, one circulatory collapse and bowel ischemia, and one anastomotic leak. The authors concluded that laparoscopic resection of acute large bowel obstruction is feasible and safe, which has a low complication rate and allows patients an early hospital discharge[27].
3.7. Acute mesenteric ischemia
The acute mesenteric ischemia is an elusive disease, with initial nonspecific symptoms until late peritonitis occurs. Nowadays, the modern imagistic tools increase the chance for early diagnosis and successful treatment. However, we should always remember the characterization of the disease by Cokkinis, in 1926: “Occlusion of the mesenteric vessels is apt to be regarded as one of those conditions of which the diagnosis is impossible, the prognosis is hopeless, and the treatment almost useless”[28].
In 2016, the European Society of Emergency Surgery published their guideline for acute mesenteric ischemia and concluded that there is insufficient evidence to support the routine use of laparoscopy in acute mesenteric ischemia for diagnosis or secondlook[29].
3.8. Abdominal trauma
In hemodynamically stable trauma patients with suspected abdominal injuries, laparoscopy can be performed safely and effectively[30–34]. The advantages are the reduction of the nontherapeutic/unnecessary laparotomy rate, shortening of hospitalization and cost-effectiveness. Blood loss higher than 750 mL, heart rate over 100 beats per minute, hemodynamic instability, and severe traumatic brain injury are a contraindication for laparoscopy. The main indication of laparoscopy in trauma patients is for diagnosis of occult diaphragmatic injuries in left thoracoabdominal penetrating wounds.
A systematic review of 51 studies revealed a sensitivity for laparoscopy in penetrating abdominal trauma of 66.7%-100%, a specificity of 33.3%-100%, with an accuracy of 50%-100%. Missed intraabdominal injuries were found in 3.3% of cases[32].
The medical literature is confusing about the current indications of minimally invasive approach in blunt trauma patients. In blunt injuries, the laparoscopy was proposed for suspected diaphragmatic injuries (found in 0.065%-0.148% of patients), suspected cavitary organ injury (found in 0.9%-2.5% of patients), the presence of free peritoneal fluid without solid organ lesions, discrepancy between imagistic and clinical examination, and as adjunctive of selective nonoperative management of grade IV – V liver injuries. An analysis of the National Trauma Data Bank between 2007-2010 found 4 755 patients who underwent diagnostic laparoscopy. Among them, 19.3%had a therapeutic laparoscopy, including diaphragm repair, bowel repair or resection and splenectomy[35].
4. Conclusion
According to the current evidence, the laparoscopic approach is an integral part of the emergency surgery for all the abdominal pathologies. Although laparoscopy requires special training and curricula, it brings all the benefits of minimal access in acute care arena.
Conflict of interest statement
The authors report no conflict of interest.
[1] Lupinacci RM, Menegaux F, Trésallet C. Emergency laparoscopy: Role and implementation.J Visc Surg2015; 152: S65-71.
[2] Katabathina VS, Zafar AM, Suri R. Clinical presentation, imaging, and management of acute cholecystitis.Tech Vasc Interv Radiol2015; 18:256-265.
[3] Zha Y, Zhou ZZ, Chen XR, Gan P, Tan J. Gallbladder-preserving cholelithotomy in laparoscopic and flexible choledochoscopic era.Surg Laparosc Endosc Percutaneous Tech2013; 23:167-170.
[4] Sutton AJ, Vohra RS, Hollyman M, Marriott PJ, Buja A, Alderson D,et al. Cost-effectiveness of emergency versus delayed laparoscopic cholecystectomy for acute gallbladder pathology.Br J Surg2017; 104:98-107.
[5] Zafar SN, Obirieze A, Adesibikan B, Cornwell EE, Fullum TM, Tran DD. Optimal time for early laparoscopic cholecystectomy for acute cholecystitis.J AMA Surg2015; 150: 129.
[6] Sutcliffe RP, Hollyman M, Hodson J, Bonney G, Vohra RS, Griffiths EA, et al. Preoperative risk factors for conversion from laparoscopic to open cholecystectomy: a validated risk score derived from a prospective U.K. database of 8820 patients.Hpb2016; 18: 922-928.
[7] Yamashita Y, Takada T, Strasberg SM, Pitt HA, Gouma DJ, Garden OJ,et al. TG13 surgical management of acute cholecystitis.J Hepatobiliary Pancreat Sci2013; 20: 89-96.
[8] Strasberg SM, Brunt LM. Rationale and use of the critical view of safety in laparoscopic cholecystectomy.J Am Coll Surg2010; 211: 132-138.
[9] Pucher PH, Brunt LM, Fanelli RD, Asbun HJ, Aggarwal R. SAGES expert Delphi consensus: critical factors for safe surgical practice in laparoscopic cholecystectomy.Surg Endosc2015; 29: 3074-3085.
[10] Strasberg SM, Pucci MJ, Brunt LM, Deziel DJ. Subtotal cholecystectomy-‘fenestrating’ vs ‘reconstituting’ subtypes and the prevention of bile duct injury: Definition of the optimal procedure in difficult operative conditions.J Am Coll Surg2016; 222: 89-96.
[11] Di Saverio S, Birindelli A, Kelly MD, Catena F, Weber DG, Sartelli M,et al. WSES Jerusalem guidelines for diagnosis and treatment of acute appendicitis.World J Emerg Surg2016; 11: 34.
[12] Gorter RR, Eker HH, Gorter-Stam MAW, Abis GSA, Acharya A,Ankersmit M, et al. Diagnosis and management of acute appendicitis.EAES consensus development conference 2015.Surg Endosc2016; 30:4668-4690.
[13] Sauerland S, Jaschinski T, Neugebauer EAM. Laparoscopic versus open surgery for suspected appendicitis. In: Sauerland S.Cochrane database of systematic reviews. Chichester, UK: John Wiley & Sons,Ltd; 2010.
[14] Ukai T, Shikata S, Takeda H, Dawes L, Noguchi Y, Nakayama T, et al. Evidence of surgical outcomes fluctuates over time: Results from a cumulative meta-analysis of laparoscopic versus open appendectomy for acute appendicitis.BMC Gastroenterol2016; 16: 37.
[15] Salminen P, Paajanen H, Rautio T, Nordstr?m P, Aarnio M, Rantanen T, et al. Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis.JAMA2015; 313: 2340.
[16] Kirby A, Hobson RP, Burke D, Cleveland V, Ford G, West RM.Appendicectomy for suspected uncomplicated appendicitis is associated with fewer complications than conservative antibiotic management: A meta-analysis of post-intervention complications.J Infect2015; 70: 105-110.
[17] Sartelli M, Catena F, Ansaloni L, Coccolini F, Griffiths EA, Abu-Zidan FM, et al, WSES Guidelines for the management of acute left sided colonic diverticulitis in the emergency setting.World J Emerg Surg2016; 11(1): 37.
[18] Vennix S, Lips DJ, Di Saverio S, van Wagensveld BA, Brokelman WJ, Gerhards MF, et al. Acute laparoscopic and open sigmoidectomy for perforated diverticulitis: a propensity score-matched cohort.Surg Endosc2016; 30: 3889-3896.
[19] Schultz JK, Yaqub S, Wallon C, Blecic L, Forsmo HM, Folkesson J,et al. Laparoscopic lavage vs primary resection for acute perforated diverticulitis: The SCANDIV randomized clinical trial.JAMA2015;314: 1364-1375.
[20] Vennix S, Musters GD, Mulder IM, Swank HA, Consten EC, Belgers EH, et al. Laparoscopic peritoneal lavage or sigmoidectomy for perforated diverticulitis with purulent peritonitis: A multicentre,parallel-group, randomised, open-label trial.Lancet2015; 386: 1269-1277.
[21] Cirocchi R, Di Saverio S, Weber DG, Tabo?a R, Abraha I, Randolph J, et al. Laparoscopic lavage versus surgical resection for acute diverticulitis with generalised peritonitis: a systematic review and meta-analysis.Tech Coloproctol2017; 21: 93-110.
[22] Sanabria A, Villegas MI, Morales Uribe CH. Laparoscopic repair for perforated peptic ulcer disease. In: Sanabria A.Cochrane Database of Systematic Reviews. Chichester, UK: John Wiley & Sons, Ltd; 2013.
[23] S?reide K, Thorsen K, Harrison EM, Bingener J, M?ller MH, Ohene-Yeboah M, S?reide JA. Perforated peptic ulcer.Lancet2015; 386:1288-1298.
[24] Varcus F, Beuran M, Lica I, Turculet C, Cotarlet AV, Georgescu S,et al. Laparoscopic repair for perforated peptic ulcer: A retrospective study.World J Surg2017; 41: 948-953.
[25] Byrne J, Saleh F, Ambrosini L, Quereshy F, Jackson TD, Okrainec A.Surg Endosc2015; 29(9): 2525-2532.
[26] Farinella E, Cirocchi R, La Mura F, Morelli U, Cattorini L, Delmonaco P, et al. Feasibility of laparoscopy for small bowel obstruction.World J Emerg Surg2009; 4: 3.
[27] Gash K, Chambers W, Ghosh A, Dixon AR. The role of laparoscopic surgery for the management of acute large bowel obstruction.Color Dis2011; 13: 263-266.
[28] Boley SJ, Brandt LJ, Sammartano RJ. History of mesenteric ischemia:The Evolution of a Diagnosis and Management.Surg Clin NA1997;77: 275-288.
[29] Tilsed JVT, Casamassima A, Kurihara H, Mariani D, Martinez I,Pereira J, et al. ESTES guidelines: Acute mesenteric ischaemia.Eur J Trauma Emerg Surg2016; 42: 253-270.
[30] Kindel T, Latchana N, Swaroop M, Chaudhry UI, Noria SF, Choron RL, et al. Laparoscopy in trauma: An overview of complications and related topics.Int J Crit Illn Inj Sci2015; 5: 196-205.
[31] El-Bendary YBA, Al-Adawi J, Al-Qadhi H. The use of laparoscopy in the management of trauma patients: Brief review.Sultan Qaboos Univ Med J2016; 16: e9-14.
[32] O’Malley E, Boyle E, O’Callaghan A, Coffey JC, Walsh SR. Role of laparoscopy in penetrating abdominal trauma: A systematic review.World J Surg2013; 37: 113-122.
[33] Ozkan OV, Justin V, Fingerhut A, Uranues S. Laparoscopy in abdominal trauma.Curr Trauma Reports2016; 2: 238-246.
[34] Justin V, Fingerhut A, Uranues S. Laparoscopy in blunt abdominal trauma: For whom? when? and why?Curr Trauma Reports2017; 3: 43-50.
[35] Zafar SN, Onwugbufor MT, Hughes K, Greene WR, Cornwell EE, Fullum TM, et al. Laparoscopic surgery for trauma: The realm of therapeutic management.Am J Surg2015; 209: 627-632.
 Journal of Acute Disease2018年1期
Journal of Acute Disease2018年1期
- Journal of Acute Disease的其它文章
- A case report of acute pulmonary vein stenosis
- Acute intra-operative brain swelling managed effectively with emergency basal cisternostomy: A case report
- Diminazene aceturate modified nanocomposite for improved efficacy in acute trypanosome infection
- Role of first day levels and subsequent trends of serum proteins in acute burns
- Progress in the surgery of rectal cancer
- Acute myocardial infarction and Yin Yang imbalance
