經(jīng)皮椎間孔鏡下椎間盤(pán)摘除術(shù)治療70例腰椎間盤(pán)突出癥的療效評(píng)價(jià)
趙輝+李德仁
[摘要] 目的 探究經(jīng)皮椎間孔鏡下椎間盤(pán)摘除術(shù)治療腰椎間盤(pán)突出癥的臨床療效。 方法 研究對(duì)象選取2015年6月~2017年6月間我院收治的140例腰椎間盤(pán)突出癥患者,采用數(shù)字表法隨機(jī)分為觀察組和對(duì)照組各70例,觀察組采用經(jīng)皮椎間孔鏡下椎間盤(pán)摘除術(shù)治療,對(duì)照組采用微創(chuàng)經(jīng)椎間孔腰椎融合術(shù)治療,比較兩組患者的手術(shù)時(shí)間、術(shù)中出血量、住院時(shí)間等手術(shù)指標(biāo),并比較治療前后兩組患者的功能障礙指數(shù)(ODI)、日本骨科學(xué)會(huì)評(píng)分(JOA),統(tǒng)計(jì)手術(shù)相關(guān)并發(fā)癥。 結(jié)果 觀察組患者的手術(shù)時(shí)間、術(shù)中出血量、住院時(shí)間均顯著低于對(duì)照組,差異有統(tǒng)計(jì)學(xué)意義(P<0.05);治療前兩組患者的ODI、JOA評(píng)分比較無(wú)顯著差異(P>0.05),治療后觀察組ODI、JOA評(píng)分改善程度均顯著優(yōu)于對(duì)照組,差異有統(tǒng)計(jì)學(xué)意義(P<0.05);兩組患者均未出現(xiàn)明顯的手術(shù)相關(guān)并發(fā)癥。 結(jié)論 經(jīng)皮椎間孔鏡下椎間盤(pán)摘除術(shù)治療腰椎間盤(pán)突出癥的療效確切,與微創(chuàng)手術(shù)相比對(duì)患者的創(chuàng)傷更小,術(shù)后癥狀改善更好,值得在臨床上推廣和應(yīng)用。
[關(guān)鍵詞] 骨科;腰椎間盤(pán)突出癥;經(jīng)皮椎間孔鏡下椎間盤(pán)摘除術(shù);經(jīng)椎間孔腰椎融合術(shù)
[中圖分類(lèi)號(hào)] R687.3 [文獻(xiàn)標(biāo)識(shí)碼] B [文章編號(hào)] 1673-9701(2017)33-0063-03
[Abstract] Objective To explore the clinical effect of percutaneous transforaminal endoscopic discectomy in the treatment of lumbar disc herniation. Methods 140 patients with lumbar disc herniation from June 2015 to June 2017 admitted in our hospital were randomly divided into observation group(n=70)and control group(n=70), according to the number table method. The observation group was treated with percutaneous transforaminal endoscopic discectomy. The control group was treated with minimally invasive intervertebral foramen lumbar fusion. The operation time, intraoperative blood loss and hospitalization time were compared between the two groups. And the dysfunction indexes(ODI)and the Japan Orthopedic Association score(JOA) were compared between the two groups before and after treatment. The surgery-related complications were counted. Results The operation time, intraoperative blood loss and hospitalization time of the observation group were significantly lower than those of the control group, and the difference was significant(P<0.05). There were no significant differences in the ODI and JOA scores between the two groups before treatment(P>0.05). After treatment, the improvement degree of ODI and JOA was significantly better than that of the control group, and the difference was significant(P<0.05). There was no obvious complication in the two groups. Conclusion Percutaneous transforaminal endoscopic discectomy for the treatment of lumbar disc herniation has exact effect. And the trauma of the patients with percutaneous transforaminal endoscopic discectomy is smaller compared with that of the minimally invasive surgery and the postoperative symptoms are better. The percutaneous transforaminal endoscopic discectomy is worthy of promotion and application.
[Key words] Orthopedics;Lumbar disc herniation;Percutaneous transforaminal endoscopic discectomy;Percutaneous intervertebral lumbar fusionendprint
腰椎間盤(pán)突出癥是骨科臨床常見(jiàn)的一類(lèi)疾病,患者表現(xiàn)為患側(cè)的腰、腿疼痛及功能障礙,嚴(yán)重的影響患者的生存質(zhì)量。目前此類(lèi)疾病主要包括保守治療和手術(shù)治療兩類(lèi)方案,對(duì)于重度腰椎間盤(pán)突出癥者一般建議采用手術(shù)治療[1]。傳統(tǒng)的經(jīng)椎間孔腰椎融合術(shù)雖然能夠有效減輕患者的術(shù)后疼痛,但術(shù)后不可避免的造成椎間盤(pán)的退變[2]。隨著椎間孔鏡在臨床的推廣,腰椎間盤(pán)突出癥的治療也有了更多的選擇,經(jīng)皮椎間孔鏡下手術(shù)能夠進(jìn)一步的降低手術(shù)創(chuàng)傷,提高療效[3]。為了進(jìn)一步了解經(jīng)皮椎間孔鏡下椎間盤(pán)摘除術(shù)治療腰椎間盤(pán)突出癥的臨床療效,本文進(jìn)行了相關(guān)研究,現(xiàn)報(bào)道如下。
1 資料與方法
1.1 一般資料
研究對(duì)象選取為2015年6月~2017年6月間我院收治的140例腰椎間盤(pán)突出癥患者,采用數(shù)字表法隨機(jī)分為觀察組和對(duì)照組各70例,觀察組包括男39例,女31例,年齡39~58歲,平均(48.4±4.6)歲;對(duì)照組包括男38例,女32例,年齡38~59歲,平均(48.7±5.1)歲。兩組患者基線資料比較無(wú)顯著差異(P>0.05)。
1.2 納入及排除標(biāo)準(zhǔn)
納入標(biāo)準(zhǔn):(1)符合腰椎間盤(pán)突出癥診斷標(biāo)準(zhǔn),經(jīng)影像學(xué)檢查證實(shí);(2)保守治療3個(gè)月癥狀無(wú)緩解;(3)符合手術(shù)指征;(4)患者知情同意參與本次研究。排除標(biāo)準(zhǔn):(1)椎間盤(pán)炎性改變;(2)椎間盤(pán)鈣化;(3)多次手術(shù)的復(fù)發(fā)性腰椎間盤(pán)突出癥;(4)腰椎不穩(wěn)者;(5)合并其他嚴(yán)重內(nèi)科疾病無(wú)法進(jìn)行手術(shù)者。
1.3 手術(shù)方法
觀察組采用經(jīng)皮椎間孔鏡下椎間盤(pán)摘除術(shù)治療,患者取俯臥位,標(biāo)記棘突正中線、髂骨輪廓線、椎間盤(pán)平行線。C臂透視下將后外放斜形標(biāo)志線和經(jīng)關(guān)節(jié)突上緣的安全線標(biāo)記出來(lái)。常規(guī)消毒鋪巾后,在脊柱后正中線旁開(kāi)12~14 cm的切口作為進(jìn)針點(diǎn),對(duì)穿刺部位皮膚進(jìn)行1%利多卡因麻醉,并將22 G的穿刺針接上,然后進(jìn)行逐層穿刺,直到穿刺針到達(dá)上關(guān)節(jié)突肩部。透視證實(shí)位置滿(mǎn)意。拔除針芯,置入導(dǎo)絲,取出穿刺針,做0.5 cm左右切口,沿導(dǎo)絲置入導(dǎo)管、環(huán)鋸及擴(kuò)張導(dǎo)桿,將椎間孔擴(kuò)大,置入工作套管,調(diào)整方向指向椎間盤(pán)突出位置,將內(nèi)鏡置入工作套管,持續(xù)沖洗并摘取髓核,松解組織粘連,用射頻刀對(duì)未取出的髓核和后縱韌帶進(jìn)行進(jìn)一步的消融并止血,完成處理后拔除工作套管,常規(guī)縫合。對(duì)照組采用微創(chuàng)經(jīng)椎間孔腰椎融合術(shù)治療,患者取俯臥位,全麻手術(shù),C 臂下定位后在目標(biāo)節(jié)段后正中做3~5 cm切口,分離組織向兩側(cè)牽開(kāi),在棘突旁3 cm處做2個(gè)3 cm左右縱向切口,鈍性分離最長(zhǎng)肌至小關(guān)節(jié)突處,在上位腰椎外上緣與峽部交接處置入1級(jí)擴(kuò)張?zhí)淄玻饾u打開(kāi)術(shù)野,鑿除椎板外側(cè)、上下位腰椎相接關(guān)節(jié)突,去除黃韌帶,充分暴露病灶部位及周?chē)窠?jīng)根,保護(hù)神經(jīng)根,打開(kāi)硬脊膜后切除椎間盤(pán),用鉸刀和中板銼處理后置入椎間融合器,在雙側(cè)人字嵴點(diǎn)處置入椎弓根螺釘,加壓鎖定后放置引流,常規(guī)縫合切口。兩組術(shù)后預(yù)防感染等措施均保持一致。
1.4 評(píng)價(jià)方法
比較兩組患者的手術(shù)時(shí)間、術(shù)中出血量、住院時(shí)間等手術(shù)指標(biāo),并比較治療前后兩組患者的功能障礙指數(shù)(ODI)[4]、日本骨科學(xué)會(huì)評(píng)分(JOA)[5]。ODI包括10個(gè)問(wèn)題,每個(gè)問(wèn)題根據(jù)患者選擇得分0~5分,最終得分轉(zhuǎn)為百分制計(jì)分,分值越高說(shuō)明功能障礙越嚴(yán)重;JOA量表包括主觀癥狀、臨床體征及活動(dòng)受限程度3個(gè)維度,總分29分,分值越高說(shuō)明運(yùn)動(dòng)能力越好。
1.5 統(tǒng)計(jì)學(xué)方法
數(shù)據(jù)錄入SPSS 20.0軟件包處理,計(jì)量資料用t檢驗(yàn),計(jì)數(shù)資料用χ2檢驗(yàn),檢驗(yàn)水準(zhǔn)α=0.05,P<0.05為差異有統(tǒng)計(jì)學(xué)意義。
2 結(jié)果
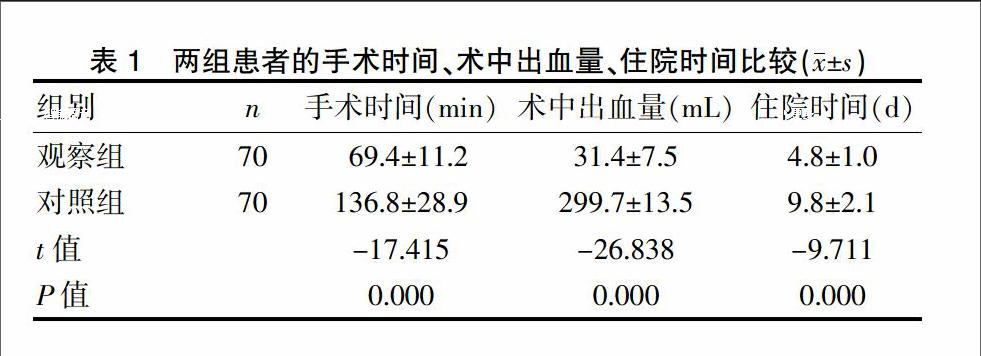
2.1兩組患者的手術(shù)時(shí)間、術(shù)中出血量、住院時(shí)間比較
觀察組患者的手術(shù)時(shí)間、術(shù)中出血量、住院時(shí)間均顯著低于對(duì)照組,差異有統(tǒng)計(jì)學(xué)意義(P<0.05)。見(jiàn)表1。
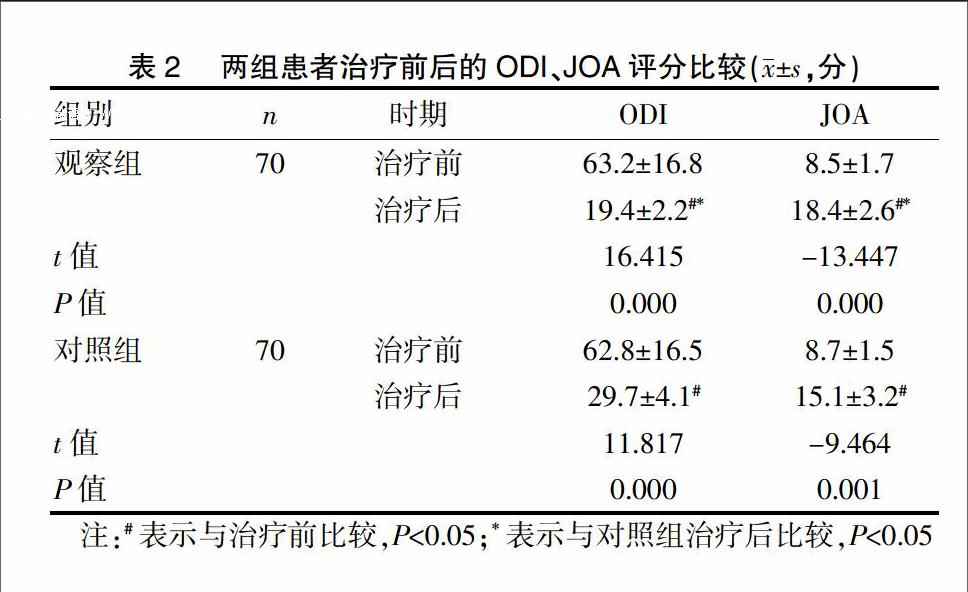
2.2兩組患者治療前后的ODI、JOA評(píng)分比較
治療前兩組患者的ODI、JOA評(píng)分比較無(wú)顯著差異(P>0.05),治療后觀察組ODI、JOA評(píng)分改善程度均顯著優(yōu)于對(duì)照組,差異有統(tǒng)計(jì)學(xué)意義(P<0.05)。見(jiàn)表2。
2.3 兩組并發(fā)癥比較
兩組患者均未出現(xiàn)明顯的手術(shù)相關(guān)并發(fā)癥。
3 討論
重度腰椎間盤(pán)突出癥目前主要以手術(shù)治療為主,傳統(tǒng)的椎間盤(pán)有限切除術(shù)術(shù)后對(duì)患者的癥狀改善有限,且術(shù)后易再次復(fù)發(fā)[6,7],為了確保療效,同時(shí)避免過(guò)多椎間盤(pán)切除導(dǎo)致脊柱不穩(wěn)、椎間隙狹窄等并發(fā)癥的發(fā)生,椎間盤(pán)切除椎間融合術(shù)受到推崇,此類(lèi)手術(shù)能夠有效地改善患者的癥狀,且與傳統(tǒng)有限切除術(shù)相比能夠更好地防止術(shù)后復(fù)發(fā)[8,9]。但椎間盤(pán)融合術(shù)可能會(huì)導(dǎo)致鄰近節(jié)段發(fā)生退變,且患者術(shù)后硬膜外瘢痕難以避免,對(duì)于老年患者而言,這些問(wèn)題并不突出,然而對(duì)于青中年患者而言首次即進(jìn)行椎間盤(pán)融合術(shù)治療容易導(dǎo)致腰椎活動(dòng)度降低、神經(jīng)根損傷、異位骨化等并發(fā)癥[10,11]。
隨著椎間孔鏡在臨床的推廣應(yīng)用,腰椎間盤(pán)突出癥的治療也有了更多選擇。椎間孔鏡下手術(shù)進(jìn)一步體現(xiàn)了微創(chuàng)手術(shù)的特點(diǎn),鏡下能夠直接觀察到患者病灶部位的各類(lèi)情況,且能夠通過(guò)工作套管的移動(dòng)來(lái)觀察髓核的位置變化,評(píng)估神經(jīng)根狀態(tài)及硬脊膜搏動(dòng)情況[12]。利用亞甲藍(lán)染色能夠區(qū)分發(fā)生蛻變的酸性髓核,更便于鏡下區(qū)分并切除,可有效避免過(guò)分切除或?qū)е虏∽儦埩鬧13]。椎間孔鏡下手術(shù)能夠?yàn)槭中g(shù)提供清晰的視野,能夠在直視下切除突出的髓核,并可對(duì)鈣化的后縱韌帶、破裂的軟骨終板及纖維環(huán)進(jìn)行處理。利用髓核鉗可輕易處理變性的髓核組織,而射頻則能夠?qū)埩艚M織進(jìn)行進(jìn)一步處理[14]。射頻下能夠觀察到變性髓核和正常髓核的差異,正常髓核在汽化前會(huì)出現(xiàn)溢油樣改變,從而避免造成正常髓核的損傷,最大程度避免并發(fā)癥的發(fā)生[15]。從本次研究數(shù)據(jù)來(lái)看,觀察組患者的手術(shù)時(shí)間、術(shù)中出血量、住院時(shí)間均顯著低于對(duì)照組,說(shuō)明椎間孔鏡下手術(shù)能夠進(jìn)一步發(fā)揮微創(chuàng)手術(shù)的優(yōu)勢(shì),減少了患者的手術(shù)創(chuàng)傷,為術(shù)后快速康復(fù)提供了條件。從兩組患者治療前后的ODI、JOA評(píng)分比較來(lái)看,治療后觀察組ODI、JOA評(píng)分改善程度均顯著優(yōu)于對(duì)照組,說(shuō)明兩種術(shù)式都能夠有效改善患者的關(guān)節(jié)功能,但椎間孔鏡下手術(shù)能夠更有效地解除病灶部位的功能障礙,從而提高療效。endprint
需要指出的是,椎間孔鏡下手術(shù)的成功率取決于工作套管的置入位置,對(duì)于高度移位的游離髓核,椎間孔鏡下手術(shù)的療效有限,即使能夠捕捉到游離髓核,也容易出現(xiàn)髓核殘留的情況,需要二次手術(shù)處理,不但增加了手術(shù)創(chuàng)傷,還可能導(dǎo)致神經(jīng)根損傷。此外,由于本次研究時(shí)間所限,并未對(duì)患者進(jìn)行長(zhǎng)期隨訪,因此僅能進(jìn)行近期療效評(píng)價(jià),遠(yuǎn)期療效評(píng)價(jià)尚需進(jìn)一步研究證實(shí)。
綜上所述,經(jīng)皮椎間孔鏡下椎間盤(pán)摘除術(shù)治療腰椎間盤(pán)突出癥的療效確切,與微創(chuàng)手術(shù)相比對(duì)患者的創(chuàng)傷更小,術(shù)后癥狀改善更好,值得在臨床上推廣和應(yīng)用。
[參考文獻(xiàn)]
[1] Watanabe K,Yamazaki A,Morita O,et al.Clinical outcomes of posterior lumbar interbody fusion for lumbar foraminal stenosis:Preoperative diagnosis and surgical strategy[J]. J Spinal Disord Tech,2011,24(3):137-141.
[2] 黃承軍,唐福宇,王力平,等.可擴(kuò)張通道系統(tǒng)輔助椎間盤(pán)鏡下經(jīng)椎間孔腰椎椎體間融合術(shù)的初步使用[J].中國(guó)微創(chuàng)外科雜志,2009,9(8):747-749.
[3] Doi T,Harimaya K,Matsumoto Y,et al.Endoscopic decompression for intraforaminal and extraforaminal nerve root compression[J]. J Orthop Surg Res,2011,41(6):16.
[4] Firbank J,Pynsent P.The Oswestry disability index[J]. Spine,2014,39(2):2940-2953.
[5] 井上駿一.腰痛治療成績(jī)判定基準(zhǔn)[J].日整會(huì)志,1986,60:391-394.
[6] MacNab I.Negative disk exploration: An analysis of the causes of nerve-root involvement in sixty-eight patients[J].J Bone Joint Surg(Am),2016,88(4):891-903.
[7] Watters WC,McGirt MJ. An evidence-based review of the literature on the consequences of conservative versus aggressive discectomy for the treatment of primary disc herniation with radiculopathy[J].Spine,2015,15(3):240-257.
[8] McGirt MJ,Ambrossi GL,Garcés BS,et al. Recurrent disc herniation and long-term back pain after primary lumbar discectomy:Review of outcomes reported for limited versus aggressive disc removeal[J].Neurosurgery,2015,70(2):338-344.
[9] Liu T,Zhou Y,Wang J,et al.Clinical efficacy of three different minimally invasive procedures for far lateral lumbar disc herniation[J].Chin Med J,2012,125(5):1082-1088.
[10] Wang JC,Arnold DM,Hermsmeyer JT,et al.Do lumbar motion preserving devices reduce the risk of a adjacent segment pathology compared with fusion surgery? A systematic review[J].Spine,2012,37(22 Suppl):S133-S143.
[11] Chrastil J,Patel AA. Complication associated with posterior and transforiminal lumbar interbody fusion[J].J Am Acad Orthorp Surg,2012,20(5):289-291.
[12] Lew SM,Mchalic TF,F(xiàn)agone KL.Transforaminal percutaneous endoscopic discectomy in the treatment of far-lateral and foraminal lumbar disc herniations[J]. J Neuro Surg,2011,104(2 Suppl):216-220.
[13] 趙偉,李長(zhǎng)青,周躍,等.經(jīng)皮椎間孔鏡下TESSYS 技術(shù)治療腰椎間盤(pán)突出癥[J].中國(guó)矯形外科雜志,2012,20(3):1191-1195.
[14] 李長(zhǎng)青,周躍,王建,等.經(jīng)皮內(nèi)窺鏡下手術(shù)治療腰椎間盤(pán)突出癥的并發(fā)癥及其防治策略[J].中國(guó)脊柱脊髓雜志,2012,22(11):969-974.
[15] Hermantin FU,Peters T,Quartararo L,et al. A prospective randomized study comparing the results of open discectomy with those of video-assisted arthroscopic microdiscectomy[J].J Bone Joint Surg Am,2016,98(7):958-965.
(收稿日期:2017-09-07)endprint

