An unusual case of renal calculi leading to myocardial infarction and cardiogenic shock
Vanessa Santos, James Espinosa, Alan Lucerna, Andrew Caravello
Department of Emergency Medicine, Rowan University SOM Kennedy University Hospital, Stratford, NJ, USA
Letter to the editor
An unusual case of renal calculi leading to myocardial infarction and cardiogenic shock
Vanessa Santos, James Espinosa, Alan Lucerna, Andrew Caravello
Department of Emergency Medicine, Rowan University SOM Kennedy University Hospital, Stratford, NJ, USA
World J Emerg Med 2017;8(2):148–150
INTRODUCTION
The presentation of cardiogenic shock (CS) is usually straightforward, and includes hypotension, absence of hypovolemia, and clinical signs of poor tissue perfusion such as oliguria, cyanosis, cool extremities and altered mentation.[1]The most common etiology of CS is acute myocardial infarction.[2]Here, we report a case of a 42-year-old male who presented with right flank pain, nausea and vomiting initially thought to be nephrolithiasis, which he had a history of but was ultimately diagnosed with CS due to a type II myocardial infarction. This case illustrates the importance of having a broad differential diagnosis especially when a patient's vital signs take a drastic turn since this patient initially resembled someone with nephrolithiasis.
CASE
A 42-year-old Caucasian male presented to the emergency department (ED) for the evaluation of right fl ank pain associated with nausea and vomiting radiating to his right groin that began two hours prior to arrival. He stated that he had been in his normal state of health prior to the onset of symptoms. The patient reported that his symptoms were exactly the same as his prior episode of renal calculi. Examination of the abdomen did not reveal any pulsatile mass and bilateral radial pulses are equal. He denied hematuria, dysuria, fevers or chills. He denied chest pain and sob. He denied any trauma or falls. He denied travel or recent hospitalizations. Other than moderate distress secondary to pain, his vital signs were unremarkable.
Initial laboratory data was noteworthy for a white blood cell count of 15 900×103(4 800–10 800); with segmented neutrophils of 81.3% (42%–75%). A renal ultrasound was performed showing a 3 mm stone in the lower pole of the right kidney with no evidence of hydronephrosis or solid mass.
Approximately 2.5 hours later, the patient became hypoxic and started complaining of shortness of breath. The patient was placed on a non-rebreather since his saturation deceased to the 70's–80's percent saturation range. Given the drastic change in the patient's clinical status, additional labs and imaging studies were ordered. The arterial blood gas was remarkable for pH 7.35 (7.34–7.45), PaCO251 mmHg (32–45), PaO295 mmHg (65–116), HCO328 mmol/L (20–26), SAO297%, arterial oxygen saturation (measured) 98% on a non-rebreather mask. Other notable laboratory data was a troponin 1.25 ng/mL (0.00–0.50), CKMB 16.1 ng/mL (0.0–12.0), brain natriuretic protein 405 pg/mL, CK 195 U/L (40–172). An electrocardiogram (ECG) showed sinus tachycardia with a ventricular rate of 102 with right bundle branch block (RBBB), slight T-wave depression in lateral precordial leads (V4–V6) and Q waves in inferior leads, age undetermined (Figure 1).
CTA aorta study demonstrated cardiomegaly with small bilateral pleural effusions and diffuse interstitial edema compatible with CHF. It also showed patchy alveolar infiltrates in the upper lobes that could reflect pulmonary edema or superimposed bilateral pneumonia. There was no aortic aneurysm or dissection, pericardial effusion or pulmonary embolus.
A repeat ECG showed sinus rhythm at 94 beats per minute with ST-segment depression in leads V3–V5 (Figure 2).
While the patient was at the CT scan suite (having completed the study), the patient became progressively hypoxic and was eventually intubated. Shortly after intubation, the patient became hypotensive with blood pressure (BP) around 80/50 mmHg. A central venous catheter (CVP) was placed and norepinephrine was administered to improve his BP. Furthermore, the patient had a prolonged episode of hypoxia in which he requiredmanual ventilation after being disconnected from the ventilator. The patient was admitted to the Intensive Care Unit. An echocardiogram was performed demonstrating akinesia of the inferior wall and mild hypokinesis of the anterolateral wall (Figure 3) with an estimated EF 40% and moderate-to-severe mitral regurgitation (Figure 4). The patient was transferred to another hospital for emergent cardiac cauterization.
The patient's coronary fi ndings on cardiac catheterization were as follows (Figures 5, 6): (1) Left main: luminal irregularities. (2) LAD showed 30%–40% mid stenosis. The D1 was a small size vessel with severe disease proximally. The D2 was small to medium size vessel with proximal 100% chronic total occlusion. (3) Left circumflex (LC): proximal 100% occlusion with faint left-to-left collaterals. (4) RCA: mid 70% stenosis of the distal vessel, 100% occluded with left-to-right collaterals. (5) EF was 25% with inferior akinesia and the remainder of the walls were hypokinetic.

Figure 1. Initial ECG: sinus tachycardia at 102 beats per minute with RBBB and T wave depressions in lateral precordial leads (V4-V6).
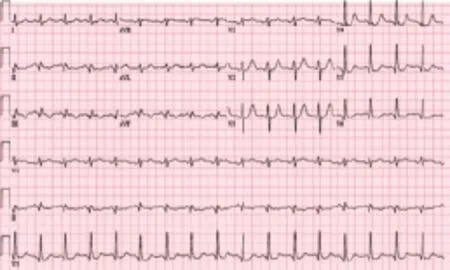
Figure 2. Repeat ECG after unstable clinical status: Sinus rhythm at 94 beats per minute with RBBB, short PR and marked ST segment depression in leads V3- V5 .
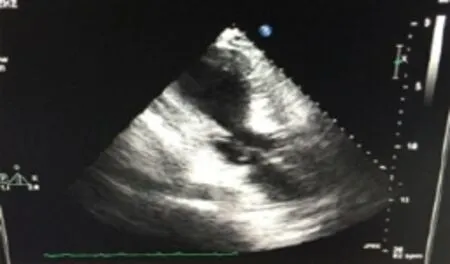
Figure 3. Hypokinesis of the anterolateral wall .
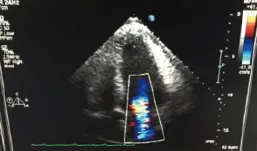
Figure 4. Moderate-to-severe mitral regurgitation.
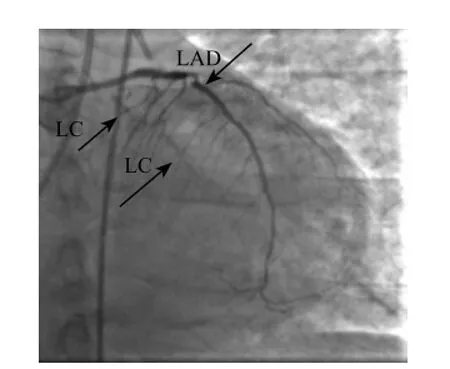
Figure 5. Cardiac catheterization, LAD and LC.
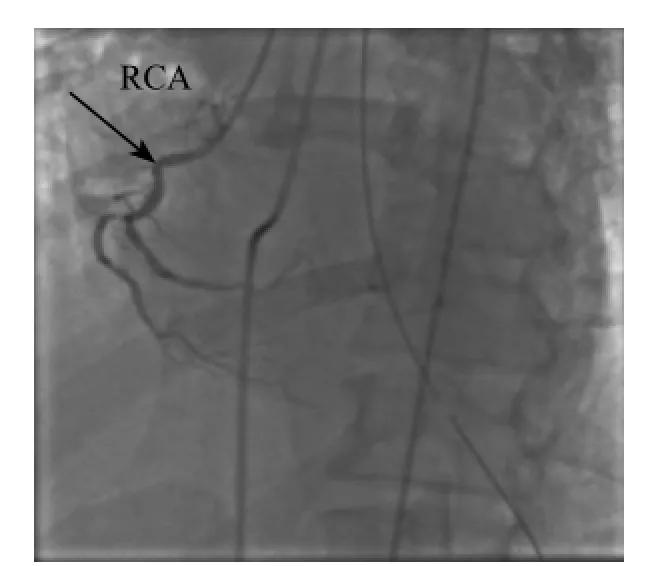
Figure 6. Cardiac catheterization, RCA.
DISCUSSION
Risk factors for developing CS in the context of an acute MI include older age, anterior MI, hypertension, diabetes mellitus, multi vessel coronary artery disease, prior MI or angina, history of heart failure, ST elevation myocardial infarction (STEMI) and left bundle branch block.[2–4]The most common etiology of CS is acute myocardial infarction (AMI).[2]Furthermore, atypical symptoms are mostly found among elderly females with diabetes, hypertension and previous heart disease.
The incidence of CS has been falling over the past40 years[2]Historically, the mortality rate was estimated to be as high as 80% to 90%.[5]Due to the high mortality that it is still associated with CS, physicians have adapted a more aggressive approach when treating patients with an AMI in order to prevent its development. In parallel with an increasing use of revascularization, mortality due to CS has declined in the USA and Europe.[5–7]
Current guidelines recommend early revascularization for all patients with STEMI and patients with CS in the setting of non-ST segment elevation myocardial infarction (NSTEMI) or unstable angina.[4]The importance of revascularization was demonstrated by the SHOCK trial, which randomized 302 patients with acute MI and CS to emergency revascularization vs. initial medical stabilization.[4]Mortality was improved for patients receiving early revascularization both at 6 months (50.3% vs. 61.3%[8]and at 6 years (32.8% vs. 19.6%).[9]
In the emergency department, the patient described in this case had symptoms consistent with nephrolithiasis. While the ultrasound showed non-obstructive uropathy, it is possible that the patient may have passed the stone. The patient's pain however may have induced an acute event to on already predisposed myocardial vasculature resulting in an acute coronary syndrome. The subsequent clinical change to the patient's condition led to additional studies and reconsideration of other differential diagnoses leading to identification, and directed treatment of an evolving acute coronary syndrome with cardiogenic shock. This case presented a patient that may have presented with a non-cardiac pain that induced stress and high sympathetic tone masking an undiagnosed coronary artery disease.
This is indeed an uncommon presentation for CS and type II AMI in totality especially in a patient with no known history of coronary artery. At present, there is no known literature describing acute kidney stone pain leading to acute myocardial infarction or cardiogenic shock making this case so unique. Atypical presentation of AMI posts a signif i cant challenge to the clinician and is associated with increased morbidity and mortality. This unique case helps illustrate why an ECG may be helpful in patients with fl ank pain when the patient's clinical picture appears more complicated than a simple renal calculus.
CONCLUSIONS
This case illustrated a unique case of CS complicated by a type II myocardial infarction manifesting as renal calculi. In this case study, nephrolithiasis likely led to stress that led to myocardial infarction, causing CS. Any acute stress reaction might result in direct myocardial involvement. As emergency physicians, it is imperative that we develop a broad differential diagnosis when presented with different disease processes and learn to change direction when a clinical course changes significantly. The environment of emergency medicine is full of atypical presentation of typical diseases. Reconsideration, therefore of the working diagnosis is imperative with any changes in a clinical course. This unique case report of cardiogenic shock complicated by myocardial infarction presenting as renal calculi beautifully captured and illustrated such presentation.
Funding: None.
Ethical approval: Not needed.
Conflicts of interest: The authors declare that there are no conf l icts of interest related to the publication of this paper.
Contributors: Santos V proposed the study, analyzed the data and wrote the fi rst drafts. All authors contributed to the design and interpretation of the study and to further drafts..
REFERENCES
1 Xiushui (Mike) R. (2015, Dec 13) Cardiogenic Shock.eMedicine. Retrieved 2/15/2016 from http://emedicine.medscape.com/ article/152191-overview#showall
2 Reynolds HR, Hochman JS. Cardiogenic shock: current concepts and improving outcomes. Circulation. 2008;117(5):686–97.
3 Spence N, Abbott JD. Coronary revascularization in cardiogenic shock. Curr Treat Options Cardiovasc Med. 2016;18(1):1.
4 Doll JA, Ohman EM, Patel MR, Milano CA, Rogers JG, Wohns DH, et al. A team-based approach to patients in cardiogenic shock. Catheter Cardiovasc Interv. 2016;88(3):424–33.
5 Goldberg RJ, Gore JM, Alpert JS, Osganian V, de Groot J, Bade J, et al. Cardiogenic shock after acute myocardial infarction. incidence and mortality from a community-wide perspective, 1975 to 1988. N Engl J Med. 1991;325(16):1117–22.
6 Babaev A, Frederick PD, Pasta DJ, Every N, Sichrovsky T, Hochman JS, et al. Trends in management and outcomes of patients with acute myocardial infarction complicated by cardiogenic shock. JAMA. 2005;294(4):448–54.
7 Goldberg RJ, Spencer FA, Gore JM, Lessard D, Yarzebski J. Thirty-year trends (1975 to 2005) in the magnitude of, management of, and hospital death rates associated with cardiogenic shock in patients with acute myocardial infarction: a population-based perspective. Circulation. 2009;119(9):1211–9.
8 Hochman JS, Sleeper LA, Webb JG, Sanborn TA, White HD, Talley JD, et al. Early revascularization in acute myocardial infarction complicated by cardiogenic shock. SHOCK Investigators. Should we emergently revascularize occluded coronaries for cardiogenic shock. N Engl J Med. 1999;341(9):625–34.
9 Hochman JS, Sleeper LA, Webb JG, Dzavik V, Bnller CE, Aylward P, et al. Early revascularization and long-term survival in cardiogenic shock complicating acute myocardial infarction. JAMA. 2006;295(21):2511–5.
Received July 1, 2016
Accepted after revision January 20, 2017
10.5847/wjem.j.1920–8642.2017.02.012
Alan Lucerna, Email: lucernaa@gmail.com
 World journal of emergency medicine2017年2期
World journal of emergency medicine2017年2期
- World journal of emergency medicine的其它文章
- Instructions for Authors
- Information for Readers
- World Journal of Emergency Medicine
- Acute airway emergency caused by an organic foreign body located in the laryngeal mucosa
- Bacteremia or pseudobacteremia? Review of pseudomonas fl uorescens infections
- Diverse coagulopathies in a rabbit model with different abdominal injuries
