Clinical ef f ects of acupoints moxibustion therapy on postsurgical gastroparesis syndrome after resection of esophageal cardia cancer
Duan Tao(段濤)*, Li Wenxian(李文獻), Liu Changzeng(劉長增), Liu Zichao(劉自超), and Yang Yun(楊云)
The third surgical department, The second hospital affiliated to Nanyang medical college, Nanyang 473000, China
Clinical ef f ects of acupoints moxibustion therapy on postsurgical gastroparesis syndrome after resection of esophageal cardia cancer
Duan Tao(段濤)*, Li Wenxian(李文獻), Liu Changzeng(劉長增), Liu Zichao(劉自超), and Yang Yun(楊云)
The third surgical department, The second hospital affiliated to Nanyang medical college, Nanyang 473000, China
OBJECTIVE:To evaluate effects of acupoints moxibustion therapy on postsurgical gastroparesis syndrome (PGS) after resection of esophageal cardia cancer.
Postsurgical gastroparesis syndrome; Acupoints moxibustion; Clinical curative ef f ects
Postsurgical gastroparesis syndrome (PGS) is a syndrome in gastric motility disorders after operation with the main signs of gastric emptying disorder, gastric outlet non-mechanical obstruction. It is an early complication of surgery. The problem has been studied by domestic TCM researchers, However, the current approach ignores the application of traditional physicotherapeutics-moxa-moxibustion in PGS’s treatment.
This study applied the combination of TCM acupuncture and moxibustion, which was called acupoints moxibustion, in treating PGS, and it had unique advantages and achieved signif i cant ef f ect in the treatment of PGS.
MATERIALS AND METHODS
General information
All of the 60 patients were diagnosed as esophageal cardia cancer and conformed to postoperative diagnostic criteria of PGS in the second affiliated hospital to Nanyang medical college from August 2012 to August 2015 in this study. The study was approved by the ethics committee and consented by the patients themselves before the treatment. It included 40 males, 20 female.
Their ages are between 40 to 80, mean (61.93±7.79) years. The duration was (8.35 ± 1.30) days, of which 35 cases of esophageal cancer, 25 cases of gastric cardia. They were divided into two groups randomly by using single blind controlled method. The treatment group: 30 cases, aged 40~80 years, mean (63.3±8.13) years; course of 7~12 days, an average of (8.20±1.32) days. The control group: 30 cases, aged 40~80 years, mean (60.5±7.31) years; course of 7~12 days, an average of (8.50 ± 1.28) days. There were no remarkable differences in sex, age statistically between the two groups. There was no remarkable dif f erence in drainage volume of gastric juice, value of motilinand the score of GCSI (P>0.05).
Diagnostic criteria
PGS diagnostic criteria (Currently, there is no uniform criteria for PGS, the criteria used here is developed by referring to Zhongshan hospital PGS diagnostic criteria and the clinical experience): ①Having history of esophageal cancer surgery;② The drainage volume of gastric juice was more than 800m1 per day; ③ With the history of abdominal distention, abdominal pain, nausea, vomiting and so on;④ One or more evidence suggests that there was no mechanical obstruction for the etiology;⑤ No obvious symptoms in water and electrolyte acidbase imbalance;⑥ No related diseases to gastroparesis, such as diabetes, scleroderma, hypothyroidism etc;⑦No drug using that affected smooth muscle contraction;⑧ These symptoms lasted more than 7 days after operation.
The case in line with the standards
①The patients older were above 18 years old; ②The patients were with gastric emptying dysfunction after resection of esophageal cancer and cardiac cancer; ③Mechanical obstruction by endoscopy or angiography was excluded;④Meeting the diagnostic criteria for PGS; ⑤ The patients were with excellent compliance.
The methods and treatment
60 patients were randomly divided into two groups. Both groups underwent conventional therapies, such as fasting, continuous gastrointestinal decompression, nutritional support, maintain electrolyte, acid-base balance, symptomatic and supportive and our hospital prescription of the Tongfu Dachengqi decoction enema (1 time/3 days), there is prompt surgical treatment indications for surgery intervention. The treatment groups received conventional therapies based on the joint use acupoint moxibustion (including Jinque, Guanyuan, Qihai, Zhongwan acupoints) for treatment, acupoint moxibustion 2 times per day, in the morning and afternoon respectively, every 30 minutes, 7 days as a course of treatment, for 3 courses, and efficacy was scored. The control group received conventional therapy, 7 days as a course of treatment, for 3 courses, and efficacy was scored.
Observational index
①GCS score, the symptom score rating quantization table 1, 7, 14, 21 days after treatment (Table 1);② Tube drainage 1, 7, 14, 21 days after treatment;③ Plasma motilin assay, fasting plasma motilin value 1, 7, 14, 21 days after treatment.
Clinical criteria
This study efficacy criteria was formed by referring to Chinese new drug clinical research guidelines syndromes of clinical research guidelines.
Cure:①Main symptoms disappeared or almost disappeared, GCSI score decrease≥95%. ②Tube drainage <100mL/24h, 24h observation tube clamping the tube removed without discomfort, resumed eating with no obvious discomfort.③Plasma motilin measured parameters were significantly improved.
Improvement: ① Main symptoms were improved, 95%>GCSI score reduction≥50%.②300mL/24h>tube drainage≥100mL/24h, stomach bloating after clipping.③ Plasma motilin measured indicators improved.
Effective:①Main symptoms were improved, 50%>GCSI score reduction≥30%. ②Tube drainage was not signif i cantly reduced, still decompression. ③ Plasma motilin showed no improvement.
Invalid: ① Main symptoms did not improve, or even worsen, GCSI score decreased less than 30%. ② Tube drainage was not significantly reduced, still decompression.③ Plasma motilin showed no signif i cant improvement or even increased.
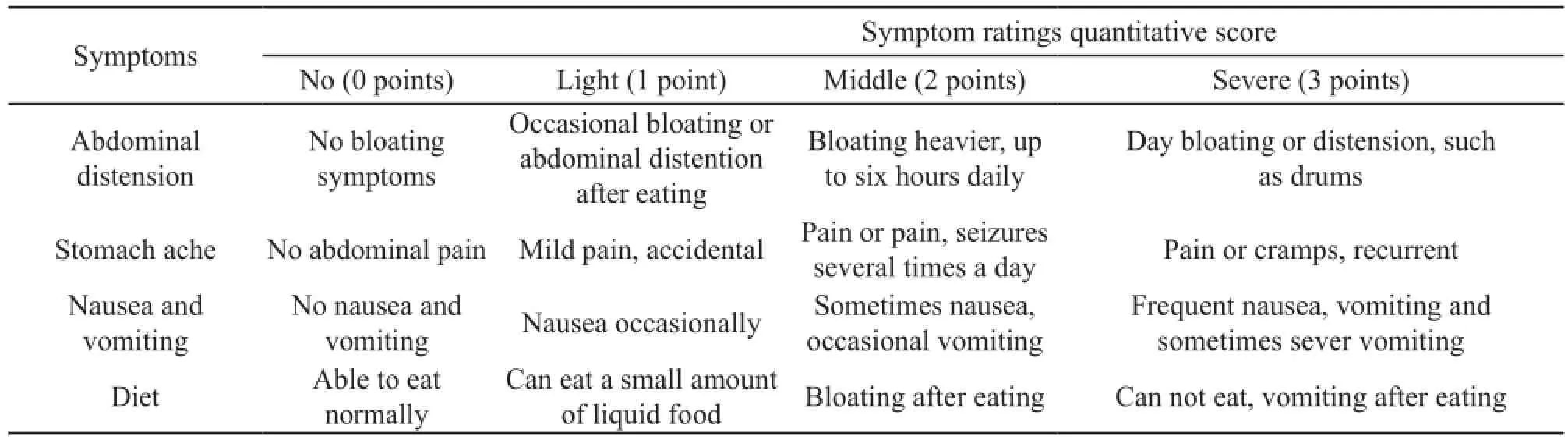
Table 1. Symptom score rating quantization table
Statistical analysis
Using SPSS 22.0 statistical software for analysis, measurement data using mean ± standard deviation, paired T test before and after treatment in the same group, between groups usingttest, count data usingx2test, withP<0.05 for the statistically signif i cant dif f erence.
RESULTS
Comparison of GCS scores, gastric drainage, motilin before and after treatment
Two symptom ratings quantitative score (Table 2), the treatment group and the control group GCSI score, stomach drainage, changed in motilin contrast (Table 3). There were signif i cant dif f erences (P<0.05). The treatment group was better than the control group.
Comparison of clinical efficacy
According to determiner of the efficacy of the standard recovery, the treatment in the treatment group was more ef f ective in 7 and 14 days than that in the control group. The dif f erence was signif i cant (P<0.05) (Table 4), 21 days was no signif i cant difference. Nevertheless, there were more recovery cases in the treatment group than those in the control group (x2=4.59,P<0.032) (Table 5).
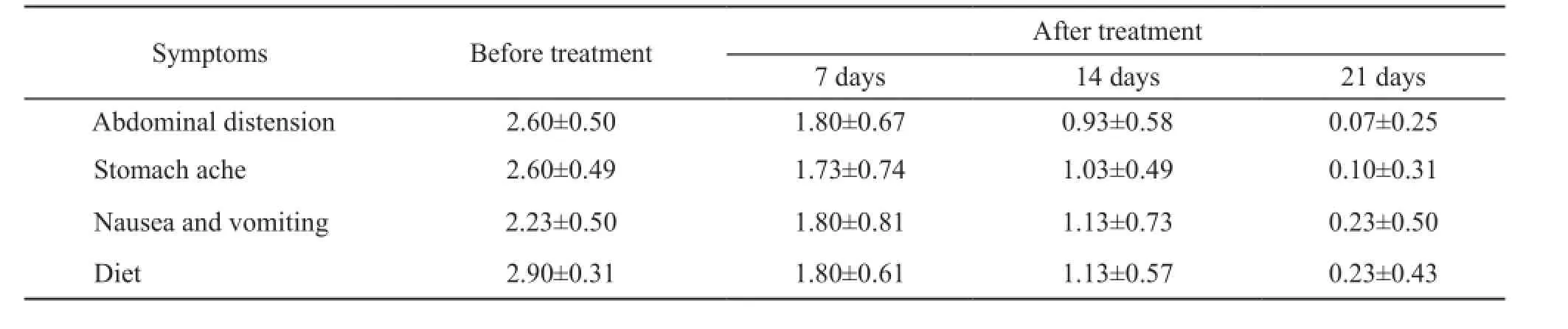
Table 2. Case analysis and comparison table before and after treatment
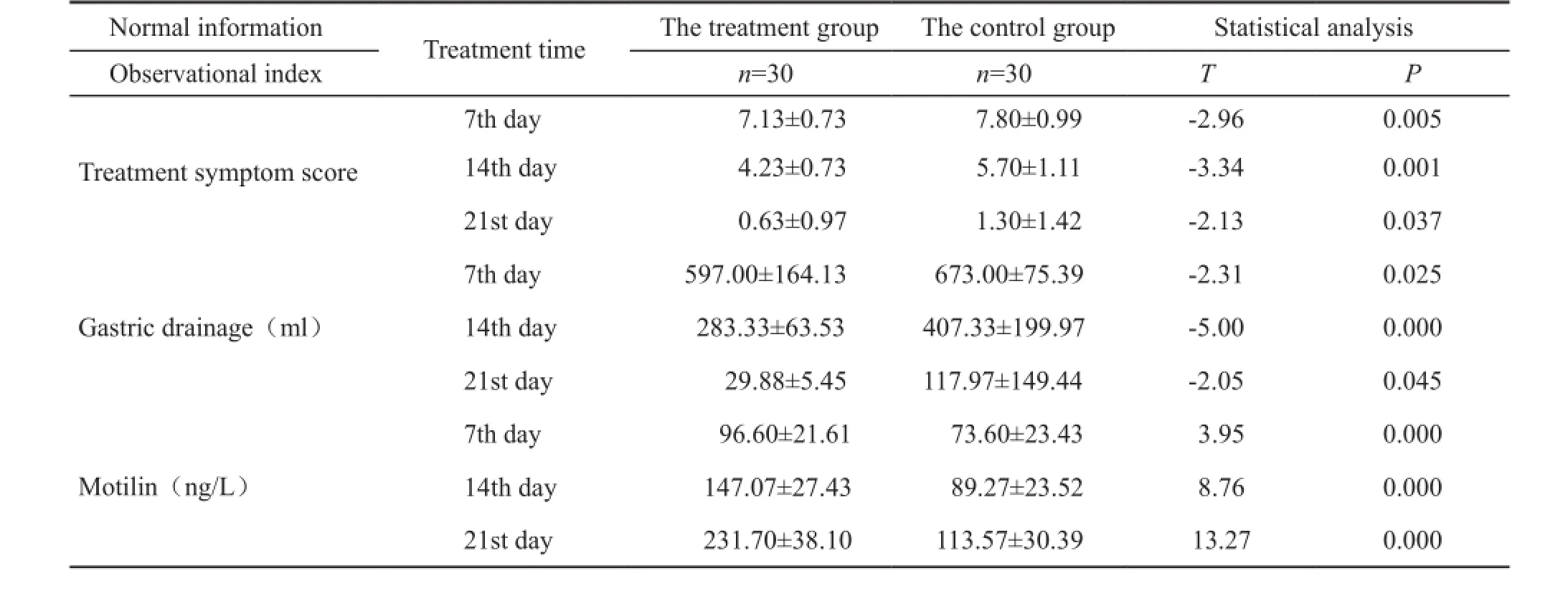
Table 3. Comparison of GCS score, stomach drainage and motilin between the two groups
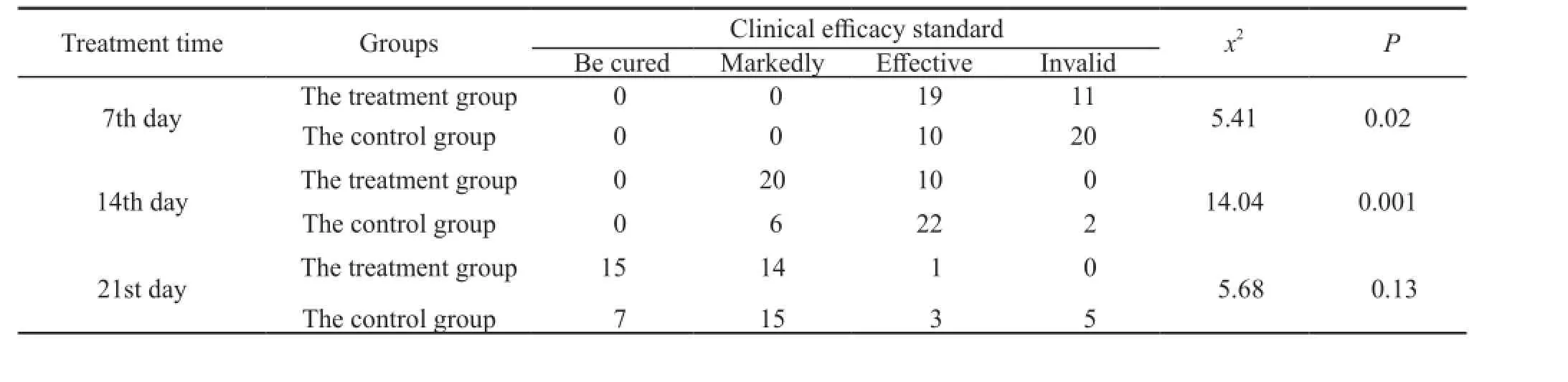
Table 4. Comparison of the ef f ect of treatment control two groups
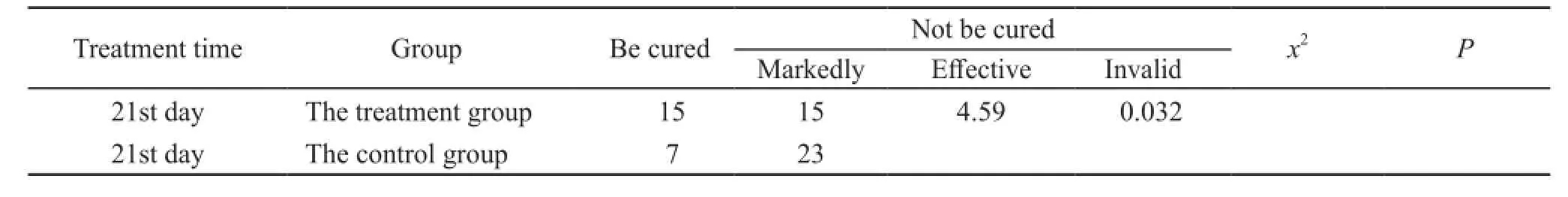
Table 5. Comparison of the cure rate in 21 days between the two groups
Adverse reactions
No adverse reactions were found in this study.
DISCUSSION
Postsurgical gastroparesis syndrome is a common early postoperative complication. According to foreign reports, the incidence is 5%~13%. PGS occurrence causes nutritional disorders after operation, and may induce other complications, even endanger the patient’s life1-5. PGS is a very common problem, with complex pathogenesis. Surgical factors are reported as the main factor in the existing literature6-9, including surgical vagotomy and cutting off nerve plexus of gastric wall by surgery, which cause the injury of gastric wall and thoracostomach and affect gastric emptying. To treat PGS the following methods are currently used: fasting, continuous gastrointestinal decompression, gastric lavage, nutritional support, promote gastrointestinal motility drugs, endoscopic therapy, psychological intervention, surgical treatment, but the ef f ect is not satisfying. In recent years, there are a lot of research on PGS both at home and abroad. The use of western medicine, traditional Chinese medicine and acupuncture and moxibustion therapy have shown significant effects. According to a large number of domestic reports, Cui Wenjun10, Qiao Xiting11, Zhang Cuiyan12and Cui Xincheng13reported the total ef f ective rate was 100%.
The scope of moxibustion treating diseases has been beyond the scope of cold syndrome. It can warm channel and expelling cold, activate meridians to stop pain, reduce swelling and resolve mass, draw out poison and bring down fever, warm spleen and stomach for dispelling cold, invigorate spleen-stomach and replenish Qi, ascend up spleen-qi and Yang, recuperate depleted Yang to treat collapse, prevent from diseases and keep health care and have other functions, and can be widely used for various diseases of various clinical departments, involving the cold syndrome, heat syndrome, deficiency syndrome and sthenia syndrome. Though folium artemisiae argyi burns during the moxibustion, yet the medicinal property still exists. The medicinal property can enter the body through the acupoint on the body surface and permeate the channels, producing the therapeutical effect. It also can directly kill the exogenous evil on the body surface, and these therapeutical ef f ects are inseparable from the heat action producing during the burning of moxibustion. The heat producing during the moxibustion is just perfect. People will feel very comfortable, heat acting on acupoint will inf l uence its surface and can enter the body through the acupoint, acting upon the channel Qi, permeating muscles and bones, viscera and even the whole body, playing the role of the whole regulation, and achieving the purpose of treating the disease. Li Qiaomei14found that moxibustion on Zhongwan, Shenque, Zusanli on postoperative abdominal distension has a signif i cant ef f ect.
TCM holds that PGS is mainly related with postoperative deficiency of Qi and blood, discord of stomach and intestine, disturbance of Qi activity, and disturbance in ascending and descending. Deficiency of Qi and blood leads to the failure of promoting the circulation of Qi. The relief of Fu-qi proves the normal function, while the obstruction of Fu-qi will cause the disorder of intestines Fu-qi activity and lead to Qi stagnation and lump in the abdomen. The treatment shall regulate the stomach and intestine, replenish blood and invigorate the circulation of blood, and regulate and relax the bowels. In traditional treatment methods, Shenque, Guanyuan, Qihai and Zhongwan acupoints can regulate intestines, promote the circulation of Qi and remove stagnation, are the commonly-used acupoints for the treatment of digestive system diseases, and have the function of regulating middle energizer and harmonizing stomach, and regulating Qi-flowing for strengthening spleen. Postoperative patient more suf f ers from the def i cient Qi and blood. With Qi as the commander of blood, Qihai has the function of tonifying Qi, strengthening cell, and regulating Ren channel, and is commonly used for diseases of Qi def i ciency, weakness and tiredness.
Guanyuan acupoint is the confluent acupoint of Ren channel and Sanyin channels of foot, so it can regulate Sanyin channels - liver, spleen and kidney, and has the function of strengthening the spleen and reinforcing deficiency, nourishing the liver and removing excretion, and nourishing the kidney and strengthening the essence. Zhongwan acupoint is the front-mu point of stomach and Hui point of Fu organs, can treat all diseases of Fu organs, and has the function of removing excretion for keeping middle jiao, regulating the middle warmer, promoting the circulation of Qi, and relaxing the bowels. Shenque acupoint, located in themiddle of abdomen and with sunken appearance, is the place of collecting channel Qi of human body and hub of lower jiao, keep adjacent to the stomach and large and small intestine inside and extends to all the limbs and bones outside, and has the function of clearing and activating the channels and collaterals, regulating Qi and blood, strengthening the spleen and stomach, nursing intestines and producing anti-diarrhea ef f ect15. The heat produced from moxa burning will directly act on the acupoints through the direct moxibustion, and heat from moxa fire will enter the body through the acupoints, acting upon channel Qi, permeating muscles and bones, viscera and even the whole body, playing the role of entire regulation, thus speeding up the postoperative rehabilitation.
According to the research founding the traditional acupoint moxibustion therapy is obviously superior to the control group in the clinical effect, greatly improving the patient’s clinical syndrome, shortening the course of disease, and giving full play to the overall regulating ef f ect. Patient compliance is good, and side ef f ect is less, ref l ecting the superiority and irreplaceability of individualized treatment of traditional Chinese medicine.
The research can ef f ectively promote the recovery of PGS. It starts from the overall, focuses on the local, produces signif i cant curative ef f ect and less side ef f ects, reduces the pain of patients suffering from postoperative gastroplegia, improves the life quality of patients, has high replicability, opens up the latest methods of traditional Chinese medicine treatment of PGS, expands the application range of acupoint moxibustion, conducts the organic combination of the external treatment technology, and is targeted to be used for the treatment of special diseases, which is the future development direction and is worthy of popularization and application16.
REFERENCES
1 Qin XY,Liu FL. The pathogenesis and treatment of postoperative gastric paralysis syndrome. Diagnosis theory and Practice,2006,5(1):13.
2 Liu YF, Wang WY, Zhou L,et al. Research progress in diagnosis and treatment of patients with gastric paralysis syndrome after abdominal surgery. Chinese Journal of Coal Industry Medicine,2012,15(4):623-626.
3 Camilleri M, Parkman HP, Shafi MA, et al. Clinical guideline: management of gastroparesis. Am J Gastroenterol, 2013,108(1):18-37.
4 Hasler WL.Gastroparesis:pathogenesis,diagnosis and managemen.Nat Rev Gastroenterol Hepatol,2011,8(8):438-453.
5 Briley LC, Harrell SP, Woosley A, et al. National survey of physicians’perception of the cause, complications, and management of gastroparesis. South Med J,2011, 104(6):412-417.
6 Li Q, He JT, Yang XJ, et al. Analysis of gastric emptying disturbance after resection of esophageal carcinoma. Chinese Journal of Thoracic and Cardiovascular Surgery, 2005,21(5):305.
7 Yan Wl, He PK. Diagnosis and treatment of postoperative thoracic gastric emptying disorder after resection of esophageal and cardiac carcinoma. Chinese Journal of Clinical Oncology,2000,27(11):868-869.
8 Wang YG, Zhang RG, Zhang DW. 27 cases of gastric emptying disorder after resection of esophageal carcinoma. Chinese Journal of Thoracic and Cardiovascular Surgery, 1998,14(4):224-226.
9 Niu JY, Li JH. Study on gastric emptying disturbance after esophageal carcinoma operation. Journal of Changzhi Medical College,2006,20(1):24.
10 Cui WJ, Wang B, Cui XB. Clinical analysis of gastric paralysis syndrome. Chinese Journal of Practical Nervous Diseases,2009,12(20):72.
11 Qiao XT, Dai YH, Qiu CL, et al. Clinical observation of 32 cases of gastric paralysis syndrome after resection of gastric cancer with modified Da Cheng Qi decoction combined with acupuncture. Guiding Journal of Traditional Chinese Medicine and Pharmacy,2013,19(9):8-10.
12 Zhang CY. Observation of therapeutic ef f ect of acupuncture on postoperative gastric paralysis. Acupuncture Research, 2010,35(6):458-461.
13 Cui XC, Liu HS. Lingguizhugan decoction in the treatment of postoperative gastroparesis syndrome in 26 cases. Hebei Journal of Traditional Chinese Medicine,2006,28(9):688.
14 Li QM, Gao SH, Wang F. Clinical observation of postoperative abdominal distention by moxibustion. Clinical Journal of Chinese Medicine,2014,16(6):42-43.
15 Dai Xi. Discussing the effect of Shenque acupoint moxibustion against diarrhea and enterocinesia. Clinical Journal of Chinese Medicine,2012,14(4):36-37.
16 Sun Qun. Efficacy observation on treating functional dyspepsia with Point application and Moxibustion. Clinical Journal of Chinese Medicine,2013,4(5):29-31.
(Accepted: May 23, 2016)
*Corresponding author: E-mail: duandoctor@126.com; Mobile phone: +86-13503900642
METHODS:60 patients with PGS after resection of esophageal cardia cancer, admitted to the second affiliated hospital to Nanyang medical college from August 2012 to August 2015, were selected and studied randomly. They were divided into the treatment group and the control group by single blind controlled method, 30 cases in each group. The gastric paralysis main symptom index (GCSI, by symptom ratings quantitative score table) score, drainage volume of gastric juice and value of motilin were recorded respectively at 1, 7, 14 and 21 days after treatment in two groups. Apart from conventional therapies, acupoints moxibustion was given on Shenque, Guanyuan, Qihai, Zhongwan acupoints, twice a day, 30 minutes once, 7 days as a course of treatment and for 3 courses in the treatment group. In the control group, the conventional therapies were given, 7 days as a course of treatment and for 3 courses.
RESULTS:The GCSI score, drainage volume of gastric juice, value of motilin in the treatment group were better than that of the control group at 7, 14, 21days respectively, and there were signif i cant dif f erences between two groups (P<0.05). The treatment group had a more sigi curative ef f ect than that in the control group at 7, 14 days respectively (P<0.05), but there was no signif i cant dif f erence at 21 day between the two groups (x2=5.68,P<0.13); nevertheless, there were more recovery cases in the treatment group than those in the control group at 21 day (x2=4.59,P<0.032). The total effective rate was 100.00% in treatment group, and 83.00% in the control group (P<0.05).
CONCLUSIONS:Acupoints moxibustion has the advantage of addressing both the symptoms and root causes of PGS after resection of esophageal cardia cancer.
 World Journal of Integrated Traditional and Western Medicine
2016年3期
World Journal of Integrated Traditional and Western Medicine
2016年3期
- World Journal of Integrated Traditional and Western Medicine的其它文章
- Effects of Kaiqiao Huazhuo prescription on the content of Matrix metallopro teinases-9 in brain of focal cerebral ischemia rats
- A medical understanding on the wuxing theory in cell
- Meta-analysis about Western Medicine combined with activating blood drugs on modulating blood glucose and lipids in diabetic patients
- A randomized, controlled trial of Shutangluo fang in treating painful diabetic peripheral neuropathy
- INSTRUCTION FOR AUTHORS
- Analysis of the features of TCM and western medicine in the diagnosis and treatment of subclinical hypothyroidism characteristics
