18FDG和99mTc-MIBI雙核素心肌顯像對冠狀動脈閉塞性缺血性心肌病治療的臨床價值
趙曼,徐予,朱中玉,安松濤,趙先鋒,陳芳
(河南省人民醫院心內科,河南 鄭州 450000)
18FDG和99mTc-MIBI雙核素心肌顯像對冠狀動脈閉塞性缺血性心肌病治療的臨床價值
趙曼,徐予,朱中玉,安松濤,趙先鋒,陳芳
(河南省人民醫院心內科,河南 鄭州 450000)
目的對單支或多支冠狀動脈完全閉塞性缺血性心肌病患者,進行99mTc-mibi/18F-FDG雙核素心肌斷層顯像檢測,以評價其對藥物治療或經皮冠狀動脈介入治療(PCI)術治療冠狀動脈閉塞性缺血性心肌病預測價值。方法139例冠狀動脈造影證實為單支或多支冠狀動脈完全閉塞缺血性心肌病患者行18F-FDG/99mTc-MIBI雙核素心肌斷層顯像,根據其結果分為有存活心肌組及無存活心肌組。2組分別根據是否進行PCI治療再分為2個亞組:PCI+優化藥物治療亞組和優化藥物治療亞組,治療12個月。以治療前、后超聲左室射血分數(LVEF)、血漿NT-B型腦鈉肽前體(NT-proBNP)水平評價治療療效。結果存活心肌組接受PCI+優化藥物治療亞組54例,優化藥物治療亞組24例。治療前LVEF、NT-proBNP水平差異無統計學意義。與治療前比較,兩亞組治療后LVEF均有增加,血NT-proBNP水平均顯著下降,差異有統計學意義。但PCI+優化藥物治療組LVEF、NT-proBNP水平均較優化藥物治療組進一步改善,差異有統計學意義。無存活心肌組中PCI+優化藥物治療亞組27例,優化藥物治療亞組34例。與治療前比較,兩亞組治療后LVEF、血NT-proBNP之間差異均無統計學意義;兩亞組治療后比較,差異無統計學意義。結論藥物治療或PCI術治療僅對經雙核素心肌斷層顯像證實有存活心肌的冠狀動脈閉塞性缺血性心肌病患者有顯著療效。
雙核素心肌灌注/代謝顯像技術;經皮冠狀動脈支架術;左心室射血分數;存活心肌;NT-proBNP
對冠狀動脈閉塞性缺血性心肌病患者經皮冠狀動脈介入治療(percutaneous coronary intervention,PCI),仍有1/4~1/3的病例心功能和預后沒有得到改善,但其部分病例僅經藥物優化治療,心功能卻比較穩定,甚至得到一定程度的改善[1]。已有研究表明,藥物治療或PCI術治療后心功能改善均與冠狀動脈閉塞相應心室壁內是否有存活心肌有關[2-7],目前國內相關報道甚少。本文對經冠狀動脈造影(coronary angiography,CAG)證實為單支或多支冠狀動脈完全閉塞性缺血性心肌病患者,進行99mTc-mibi/18F-FDG雙核素心肌斷層顯像(dual imaging using isotope stimultaneous acquisition,DISA)檢測,以評價其對藥物治療或PCI治療術治療冠狀動脈閉塞性缺血性心肌病預測價值。
1 資料與方法
1.1 研究對象
選取2011年8月-2014年1月在河南省人民醫院經CAG結果證實為單支或多支冠狀動脈完全閉塞缺血性心肌病患者139例。入選標準:①至少一支冠狀動脈完全閉塞,冠狀動脈遠端血流TIMI 0級;②心功能不全(NYHA分級Ⅱ~Ⅲ級);③超聲心動圖顯示左室舒末內徑女性>50 mm,男性>55 mm,LVEF<45%。排除標準:①急性ST段抬高型心肌梗死;②合并嚴重肺或腎臟疾病;③嚴重心臟瓣膜疾病;④6個月內腦血管疾病史。
1.2 研究方法
1.2.199mTc-MIBI/FDG雙核素SPECT心肌顯像所有患者檢查日均晨起禁食,靜脈注射99mTc-MIBI 740~1 110 MBq,20 min后進脂餐,30 min后測定患者的血糖濃度,將血糖濃度控制在7.9~8.8 mmol/L之間。如果患者血糖濃度低于7.8 mmol/L,則口服葡萄糖補充;如果血糖濃度高于8.9 mmol/L,則需要皮下注射胰島素降低血糖濃度。在血糖控制10~15 min后,靜脈注射18F-FDG 185~370 MBq,1 h后行DISA顯像。獲得短軸、垂直長軸、水平長軸的心肌灌注及心肌代謝對照圖像。由2位以上醫師盲法對灌注及代謝圖像進行評價。灌注圖像評分標準分為5級,分別為:正常;放射性分布輕度減低;中度減少;明顯減低;放射性分布缺損。以放射性分布缺損存在是否分為相應閉塞血管心肌存活組和無心肌存活組。
1.2.2 病例分組與治療所有患者均行優化藥物治療,如ACEI類藥物、β受體阻滯劑、螺內酯、他汀類藥物、阿司匹林腸溶片等,必要時加服地高辛等。2組分別根據是否進行PCI治療再分為2個亞組:PCI+優化藥物治療亞組和優化藥物治療亞組。PCI+優化藥物治療組行相應閉塞血管PCI治療,PCI術后TIMI血流均達Ⅲ級。治療后1、3、6和12個月定期門診隨訪,觀察12個月。
1.2.3 超聲心功能及NT-proBNP測定入組前和治療12個月分別進行常規心臟超聲心動圖(ultrasonic cardiography,UCG)及NT-proBNP檢測。在左側臥位下,應用彩色超聲檢測儀(飛利浦IE33)經胸行心臟彩超檢查,超聲二維左室長軸切面檢測左室舒張末內徑(LVEDD)和左室收縮末內徑(LVESD),左室射血分數(left ventricular ejection fraction,LVEF),取5個心動周期均值。經肘靜脈采血,靜脈血注入預先加入乙二胺四乙酸(EDTA)的試管中,應用羅氏Cobas E601診斷儀檢測NT-proBNP。
1.3 統計學方法
采用SPSS 16.0統計軟件進行數據分析,計量資料用均數±標準差(±s)表示,心肌存活組及無心肌存活組包括LVEF、NT-proBNP比較用t檢驗,P<0.05為差異有統計學意義。
2 結果
2.1 心肌存活組和無心肌存活組一般臨床資料
心肌存活組78例,非心肌存活組61例,兩組除PCI手術比例有明顯差異外,其他各指標之間差異均無統計學意義(P>0.05),見表1。
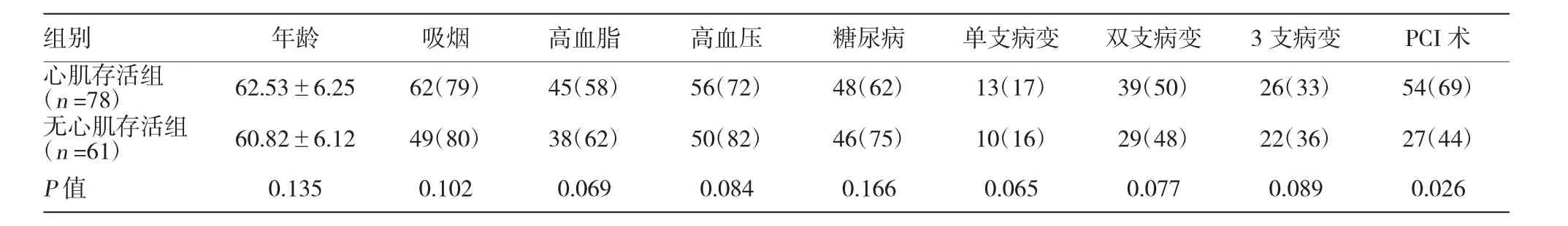
表1 心肌存活組和非心肌存活組治療前一般臨床資料例(%)
2.2 存活心肌組PCI+優化藥物治療與優化藥物治療療效比較
存活心肌組中接受PCI+優化藥物治療亞組54例、優化藥物治療亞組24例。兩個亞組心血管危險因素和冠狀動脈病變無明顯差異(P>0.05),比較治療前LVEF、NT-proBNP水平,差異均無統計學意義。2個亞組隨訪12個月后,與治療前比較,LVEF均有增加,血NT-proBNP水平均顯著下降,差異有統計學意義。但治療后12個月后,PCI+優化藥物治療組LVEF、NT-proBNP水平均較優化藥物治療組進一步改善,差異有統計學意義(P<0.05),見表2。
表2 存活心肌組PCI+優化藥物治療與優化藥物治療療效比較(±s)
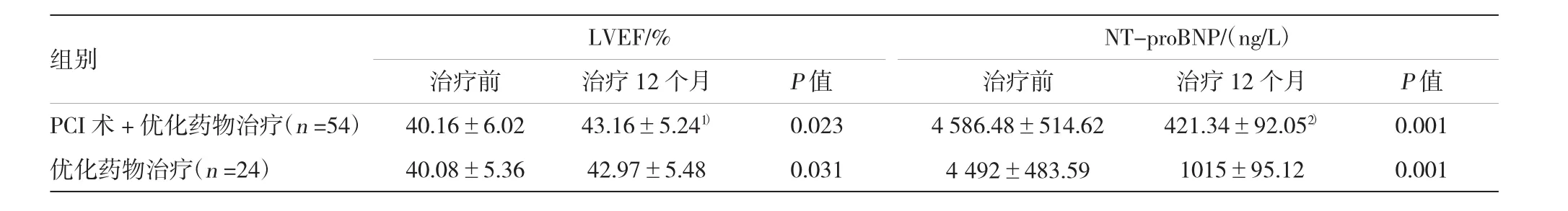
表2 存活心肌組PCI+優化藥物治療與優化藥物治療療效比較(±s)
注:1)與治療12個月后2組比較,P=0.038;2)與治療組比較,P=0.003
LVEF/%NT-proBNP/(ng/L)治療前治療12個月治療前治療12個月P值PCI術+優化藥物治療(n=54)40.16±6.0243.16±5.241)0.0234 586.48±514.62421.34±92.052)0.001優化藥物治療(n=24)40.08±5.3642.97±5.480.0314 492±483.591015±95.120.001組別P值
2.3 無存活心肌組PCI+優化藥物治療與優化藥物治療療效比較
無存活心肌組中PCI+優化藥物治療亞組27例、優化藥物治療亞組34例。與治療前比較,2個亞組隨訪12個月后LVEF、血NT-proBNP差異均無統計學意義;2個亞組治療后比較,差異亦無統計學意義,見表3。
表3 無存活心肌組PCI+優化藥物治療與優化藥物治療療效比較(±s)
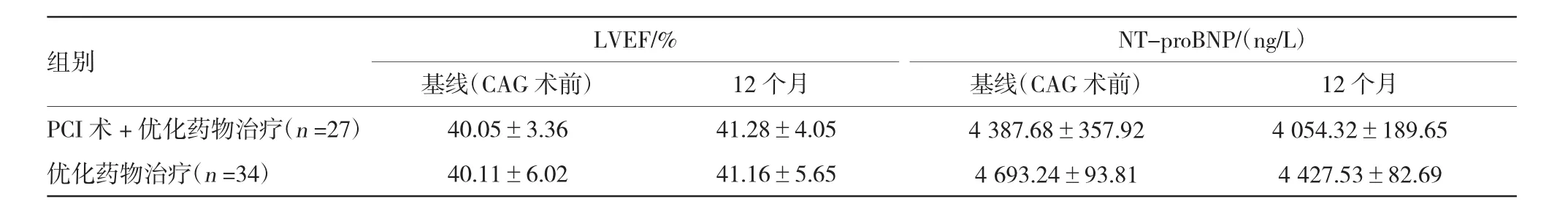
表3 無存活心肌組PCI+優化藥物治療與優化藥物治療療效比較(±s)
LVEF/%NT-proBNP/(ng/L)基線(CAG術前)基線(CAG術前)12個月PCI術+優化藥物治療(n=27)40.05±3.3641.28±4.054 387.68±357.924 054.32±189.65優化藥物治療(n=34)40.11±6.0241.16±5.654 693.24±93.814 427.53±82.69組別12個月
3 討論
99mTc-MIBI/18F-FDG雙核素同步心肌顯像可同時獲得心肌血流灌注及代謝圖像,可較準確地估價心肌灌注及代謝水平,判斷存活心肌的部位及范圍,克服單純應用FDG顯像無法區分正常和缺血心肌的局限性。其他學者應用99mTc/18F-FDG雙核素同步心肌顯像檢測存活心肌,證明DISA法SPECT顯像對檢測心肌存活性有重要價值,能有效地識別存活心肌且方法簡便[5]。國外進一步相關研究亦說明雙核素心肌顯像可以無創、快捷而又準確地觀察PCI后心肌的灌注及代謝變化[8-12]。
本研究結果顯示,單支或多支冠狀動脈完全閉塞的缺血性心肌病患者中,經18F-FDG/99mTc-MIBI雙核素心肌斷層顯像檢測,證實僅有存活心肌的患者接受PCI+優化藥物治療或單純優化藥物治療,均可顯著提高LVEF、降低血NT-proBNP水平,且聯合治療療效進一步提高;反之,PCI+優化藥物治療或單純優化藥物治療對無存活心肌的患者,上述心功能指標均無顯著性改善。本研究結果提示,對單支或多支冠狀動脈完全閉塞的缺血性心肌病患者,應進行雙核素心肌斷層顯像檢測評估存活心肌;對有存活心肌的患者推薦PCI+優化藥物治療,對無存活心肌的患者,基于PCI+優化藥物治療效果比較差異無統計學意義,僅推薦優化藥物治療。本研究支持近期國外研究結果,VAN等[13]研究證實,僅具有存活心肌的患者經血運重建后LVEF值明顯提高,而無心肌存活患者雖經血運重建,LVEF卻無明顯改善。COURAGE核素亞組研究[14]中,105例輕度缺血的患者在隨訪1年后再次接受核素檢查,結果顯示PCI+藥物治療組較單獨優化藥物治療組有更多的顯著缺血降低。隨后COURAGE核素亞組對心肌灌注顯像中度以上缺血的468例患者的分析顯示與單獨藥物治療相比,PCI+藥物治療組并未降低死亡[15]。另外,國外已有研究顯示冠心病患者存活心肌數量越多,心功能改善越顯著,反之亦然[16-18]。
本研究結果有一定的局限性,入選病例數偏少,觀察時間僅限12個月,故需要大樣本的多中心研究、且更長時間隨訪進一步證實。
總之,合理應用雙核素心肌顯像不僅可以指導患者治療方案,而且可以節約大量醫療費用,這在我國目前情況下尤為迫切和必要。
[1]ZHANG XL,LIU XJ,HU SS,et al.Impact of viable myocardium assessed by99Tcm-MIBI SPECT and 18F-FDG PET imaging on clinical outcome of patients with left ventricular aneurysm underwent revascularization[J].Chinese Journal of Cardiology,2008, 36(11):999-1003.
[2]BELLER GA,HEEDE RC.SPECT imaging for detecting coronary artery disease and determining prognosis by noninvasive assessment of myocardial perfusion and myocardial viability[J].Cardiovasc Transl Res,2011,4(4):416-424.
[3]HOLLY TA,BONOW RO,ARNOLD JM,et al.Myocardial viability and impact of surgical ventricular reconstruction on outcomes of patients with severe left ventricular dysfunction undergoing coronary artery bypass surgery:Results of the Surgical Treatment for Ischemic Heart Failure trial[J].2014,148(6):2677-2684.
[4]YAP J,TAN RS.Myocardial viability in ischemic left ventricular dysfunction[J].N Engl J Med,2011,365(5):472.
[5]BONOW RO,MAURER G,LEE KL,et al.Myocardial viability and survival in ischaemic left ventricular dysfunction[J].NEJM, 2011,69(10):1095-1096.
[6]MYLONAS I,BEANLANDS RS.Radionuclide Imaging of Viable Myocardium:is it Underutilized[J].Curr Cardiovasc Imaging Rep, 2011,4(3):251-261.
[7]LI LQ,LIU XH,ZHANG J,et al.Influences of percutaneous coronary intervention on myocardial activity in myocardial infarction patients with different viable myocardium[J].Chinese Journal of Department of Internal Medicine,2013,52(10):811-814.
[8]HUANG ZK,LOU C,SHI GH,et al.Value of(99m)Tc-MIBI/(18) F-FDG dual-isotope simultaneous acquisition in diagnosis and treatment of myocardial infarction[J].Journal of Zhejiang University,2010,39(5):530-533.
[9]ALLMAN KC.Noninvasive assessment myocardial viability:current status and future directions[J].Nucl Cardiol,2013,20(4):618-637.
[10]EL-MAGHRABY T.The use of nuclear imaging to assess the myocardial viability[J].Saudi Heart Assoc,2010,22(3):157-158.
[11]CHOPRA HK,SAMBI RS,KRISHNA CK,et al.Techniques to assess myocardial viability[J].Indian Heart J,2011,63(1):39-44.
[12]WEI H1,TIAN C,SCHINDLER TH,et al.The impacts of severe perfusion defects,akinetic/dyskinetic segments,and viable myocardium on the accuracy of volumes and LVEF measured by gated mTc-MIBI SPECT and gated F-FDG PET in patients withleftventricularaneurysm:cardiacmagneticresonance imaging as the reference[J].J Nucl Cardiol,2014,21(6):1230-1244.
[13]VAN LOON RBI,VEEN G,BAUR LH,et al.Improved clinical outcome after invasive management of patients with recent myocardial infarction and provenmyocardial viability:primary results of a randomized controlled trial(VIAMI-trial)[J].Trials,2012,3 (13):1.
[14]SHAW LJ,BERMAN DS,MARON DJ,et al.COURAGE Investigators.Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden:results from the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation(COURAGE)trial nuclear substudy[J]. Circulation,2008,117(10):1283-1291.
[15]SHAW LJ,WEINTRAUB WS,MARON DJ,et al.Baseline stress myocardial perfusion imaging results and outcomes in patients with stable ischemic heart disease randomized to optimal medical therapy with or without percutaneous coronary intervention[J].Am Heart J,2012,164(2):243-250.
[16]BAX J,EROEN J,FRANS C,et al.Relationship between preoperative viability and postoperative improvement in LVEF and heart failure symptoms[J].Nucl Med,2001,42(2):79.
[17]PEOVSKA I,MAKSIMOVIC J,VAVLUKIS M,et al.Relationship between myocardial viability and improvement in left ventricular function and heart failure symptoms after coronary artery bypass surgery[J].Prilozi,2007,28(1):97-112.
[18]UEBLEIS C,HELLWEGER S,LAUBENDER RP,et al.The amount of dysfunctional but viable myocardium predicts long term survival in patients with ischemic cardiomyopathy and left ventricular dysfunction[J].Int J Cardiovasc Imaging,2013,29(7): 1645-1653.
(張蕾 編輯)
Predictive value of radionuclide myocardial perfusion/ metabolic imaging technology(99mTc-MIBI/18F-fluorodeoxyglucose)in treatment for coronary artery occlusive ischemic cardiomyopathy
Man ZHAO,Yu XU,Zhong-yu ZHU,Song-tao AN,Xian-feng ZHAO,Fang CHEN
(Department of Cardiology,Henan Provincial People's Hospital,Zhengzhou, Henan 450000,P.R.China)
【Objective】To evaluate the predictive value of radionuclide myocardial perfusion/metabolic imaging technology[99mTc-MIBI/18F-fluorodeoxyglucose(18F-FDG)]in the treatment for coronary artery occlusive ischemic cardiomyopathy.【Methods】Totally 139 patients with ischemic cardiomyopathy associated with single or multiple coronary artery occlusion confirmed by coronary artery angiography were enrolled in this study.These patients were divided into survival myocardium and non-survival myocardium groups according to the99mTc-MIBI/18F-FDG dual isotope SPECT myocardial imaging.According to whether receiving percutaneous coronary intervention(PCI)treatment,both groups were further divided into two subgroups:PCI+optimal medical therapy and simple optimal medical therapy subgroups.The course of treatment lasted for 12 months.Left ventricular ejection fraction(LVEF)and plasma level of N-terminal probrain natriuretic peptide(NT-proBNP)before and after treatment were used to evaluate the treatment efficacy.【Results】In the survival myocardium group,LVEF was increased and the NT-proBNP level decreasedsignificantly after treatment in both subgroups.However,compared with the patients only receiving optimal medical therapy,LVEF and NT-proBNP level were further significantly improved after treatment in the patients receiving optimal medical therapy combined with PCI.In the non-survival myocardium group,no significant difference was found in LVEF or NT-proBNP level in both subgroups after treatment compared to thatbeforetreatment,therewasnosignificantdifferencebetweenbothsubgroupsaftertreatment.【Conclusions】DrugtreatmentorPCItreatmentisobviouslyeffectiveonlyforthesubjectswiththe myocardial viability among the patients with ischemic cardiomyopathy associated with single or multiple coronary artery occlusion.
radionuclide myocardial perfusion/metabolic imaging examination;PCI;left ventricular ejection fraction;viable myocardium;N-terminal pro-brain natriuretic peptide
R541.4
B
1005-8982(2015)30-0053-04
2015-06-14

