Thyroid hormone alterations in trauma patients requiring massive transfusion: An observational study
Toru Hifumi, Ichiro Okada, Nobuaki Kiriu, Eiju Hasegawa, Tomoko Ogasawara, Hiroshi Kato, Yuichi Koido, Junichi Inoue, Yuko Abe, Kenya Kawakita, Masanobu Hagiike, Yasuhiro Kuroda
1Emergency Medical Center, Kagawa University Hospital, 1750-1 Ikenobe, Miki, Kita, Kagawa, 761-0793, Japan
2Division of Critical Care Medicine and Trauma, National Hospital Organization Disaster Medical Center, 3256 Midoricho, Tachikawa, Tokyo, 190-0014, Japan
3Division of Critical Care Medicine and Trauma, Yamanashi Prefectural Central Hospital, 1-1-1 Fujimicho, Kofu, Yamanashi, 400-8506, Japan
Corresponding Author:Toru Hifumi, Email: hifumitoru@gmail.com
Thyroid hormone alterations in trauma patients requiring massive transfusion: An observational study
Toru Hifumi1, Ichiro Okada2, Nobuaki Kiriu2, Eiju Hasegawa2, Tomoko Ogasawara2, Hiroshi Kato2, Yuichi Koido2, Junichi Inoue3, Yuko Abe1, Kenya Kawakita1, Masanobu Hagiike1, Yasuhiro Kuroda1
1Emergency Medical Center, Kagawa University Hospital, 1750-1 Ikenobe, Miki, Kita, Kagawa, 761-0793, Japan
2Division of Critical Care Medicine and Trauma, National Hospital Organization Disaster Medical Center, 3256 Midoricho, Tachikawa, Tokyo, 190-0014, Japan
3Division of Critical Care Medicine and Trauma, Yamanashi Prefectural Central Hospital, 1-1-1 Fujimicho, Kofu, Yamanashi, 400-8506, Japan
Corresponding Author:Toru Hifumi, Email: hifumitoru@gmail.com
BACKGROUND:Although non-thyroidal illness syndrome (NTIS) is considered a negative prognostic factor, the alterations in free triiodothyronine (fT3) levels in trauma patients requiring massive transfusion have not been reported.
METHODS:A prospective observational study comparing 2 groups of trauma patients was conducted. Group M comprised trauma patients requiring massive transfusions (>10 units of packed red blood cells) within 24 hours of emergency admission. Group C comprised patients with an injury severity score >9 but not requiring massive transfusions. Levels of fT3, free thyroxine (fT4), and thyroidstimulating hormone (TSH) were evaluated on admission and on days 1, 2, and 7 after admission. The clinical backgrounds and variables measured including total transfusion amounts were compared and the inter-group prognosis was evaluated. Results are presented as mean±standard deviation.
RESULTS:Nineteen patients were enrolled in each group. In both groups, 32 were men, and the mean age was 50±24 years. In group C one patient died from respiratory failure. The initial fT3 levels in group M (1.95±0.37 pg/mL) were signi fi cantly lower than those in group C (2.49±0.72 pg/mL; P<0.01) and remained low until 1 week after admission. Initial inter-group fT4 and TSH levels were not significantly different. TSH levels at 1 week (1.99±1.64 μIU/mL) were higher than at admission (1.48±0.5 μIU/mL) in group C (P<0.05).
CONCLUSION:Typical NTIS was observed in trauma patients requiring massive transfusions. When initial resuscitation achieved circulatory stabilization, prognosis was not strongly associated with NTIS.
Non-thyroidal illness syndrome; Massive transfusion; Trauma; Free triiodothyronine; Thyroid hormone
INTRODUCTION
Non-thyroidal illness syndrome (NTIS) can arise following any acute or chronic illness and injuries not caused by an intrinsic abnormality in thyroid function. NTIS typically describes low levels of serum free triiodothyronine (fT3) and normal to low levels of both serum free thyroxine (fT4) and thyroid-stimulating hormone (TSH).[1]The occurrence of NTIS has been considered a negative prognostic factor, showing an association with poor prognosis for survival in various severe diseases. These include respiratory failure,[2]heart failure,[3,4]liver cirrhosis,[5]septic shock,[6]burns,[1]and elderly patients undergoing emergency surgery.[7]
Some studies have evaluated thyroid hormones intrauma patients.[8–10]Grill et al[11]evaluated 18 trauma patients and reported that low T4 levels were predictive of the need for major resuscitation. Although total plasma T3 and T4 levels are meaningful indicators of thyroid metabolism, the status of their free, protein-unbound fractions is metabolically more important.[4]Moreover, T3 has a much greater biological activity than T4.[10]There is a lack of evidence on the alterations in fT3 levels in trauma patients requiring massive transfusions; therefore, we focused on fT3 alterations in this study. Decreased thyroid function has been noted in animal models of hemorrhagic shock and resuscitation, and T3 administration improves cardiovascular parameters and mortality.[12,13]
This study investigated serum thyroid hormone levels in trauma patients requiring massive transfusion to verify whether alterations in fT3, fT4, and TSH were associated with this clinical condition and whether measurement of these variables could predict poor outcomes in such patients. In addition, we discussed the validity of supplemental thyroid hormones during therapy.
METHODS
This study was approved by the institutional review board of the National Disaster Medical Center.
Patients
This was a prospective observational study of adult trauma patients admitted to hospital. Group M comprised all trauma patients requiring massive transfusion [more than 10 units of packed red blood cells (PRBC)] within 24 hours of admission to our emergency department between April 1 and December 31, 2011. Group C (controls) comprised patients hospitalized for more than 1 week with an injury severity score (ISS) >9 but not requiring massive transfusion between January 1 and March 31, 2012.
Selection of participants
All patients were 18 years old or more and survived longer than 24 hours after admission. The exclusion criteria were as follows: kidney failure requiring dialysis, pregnancy, cardiopulmonary arrest, age less than 18 years, survival for less than 24 hours, and patients supplemented with corticosteroids or thyroid hormones.
Setting
This was a single-center study conducted at the National Disaster Medical Center (Tokyo, Japan), which is a tertiary care center with 450 inpatient beds and 33 intensive care beds. The hospital has an admission rate of approximately 3 000 patients per year and is a referral center for a region with a population of approximately 1 million people.
Data collection
The following parameters were recorded at the time of admission: age, gender, type of injuries, interval between injury and admission, ISS, lactate level on admission, systolic blood pressure (SBP), transfusion required for the fi rst 24 hours, and the administration of calcium, catecholamine, glucocorticoids or insulin.
Levels of fT3, fT4, and TSH were evaluated on admission and at days 1, 2, and 7 after admission. Quantitative determinations were performed by enzyme immunoassay (Abbott Japan, Saitama, Japan). Normal hormonal values, according to the manufacturer's instructions, were as follows: fT3, 1.45–3.48 pg/mL; fT4, 0.71–1.85 ng/dL; and TSH, 0.49–4.67 μIU/mL.
The primary endpoint was any alteration in thyroid hormone levels. The secondary outcomes were the 28-day and in-hospital mortality rates.
Statistical analysis
Statistical analysis was performed using SPSS version 20 (SPSS, Chicago, Illinois, USA). Patient characteristics, thyroid hormone levels (fT3, fT4, and TSH), and mortality rates (28-day and in-hospital) were compared between patients requiring massive transfusion and controls. The Chi-square test or the Fisher's exact test were used for categorical variables. The paired Student's t test was used to compare values within a group. A P value <0.05 was considered statistically signi fi cant. The results are presented as means±standard deviation, unless otherwise stated.
RESULTS
Over the 8-month study period, the trauma service evaluated 418 injured patients. Of these, 19 patients met the inclusion criteria for group M. During the additional 3-month observational study to obtain an equivalent control group (group C; n=19), 132 injured patients were evaluated.
Descriptive statistics
The characteristics of the 38 adult patients are summarized in Table 1. Of the 38 patients included in the study, 32 were men; the mean age of the patients was 50.4±24.3 years. The two groups had similar demographics with regard to age, gender, lactate level, interval between injury and admission, and injury mechanism. The ISS score was significantly higher in group M than in group C, whereas SBP was signi fi cantly
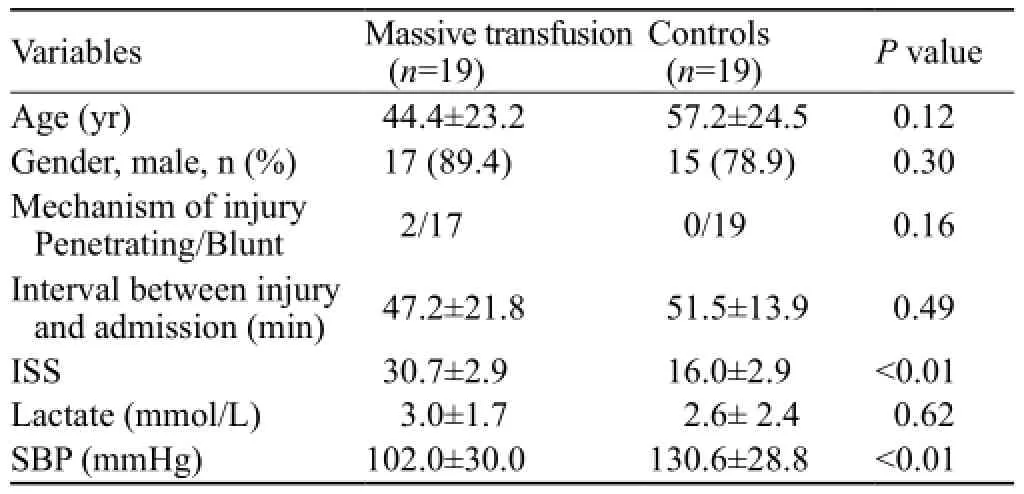
Table 1. Baseline characteristics for the massive transfusion and control groups
Values are expressed as mean±standard deviation or number of patients (%). The massive transfusion and control groups refer to groups M and C, respectively. SBP: systolic blood pressure, ISS: injury severity scoreValues are expressed as mean±standard deviation or number of patients (%). The massive transfusion and control groups refer to groups M and C, respectively. U: units, RCC: red cell concentrate, FFP: fresh frozen plasma, PC: platelet concentrates lower in group M than in group C. The transfusion requirements for the fi rst 24 hours and the administration of calcium, catecholamines, glucocorticoids and insulin are shown in Table 2. Only one patient died from respiratory failure in group C (Table 2).
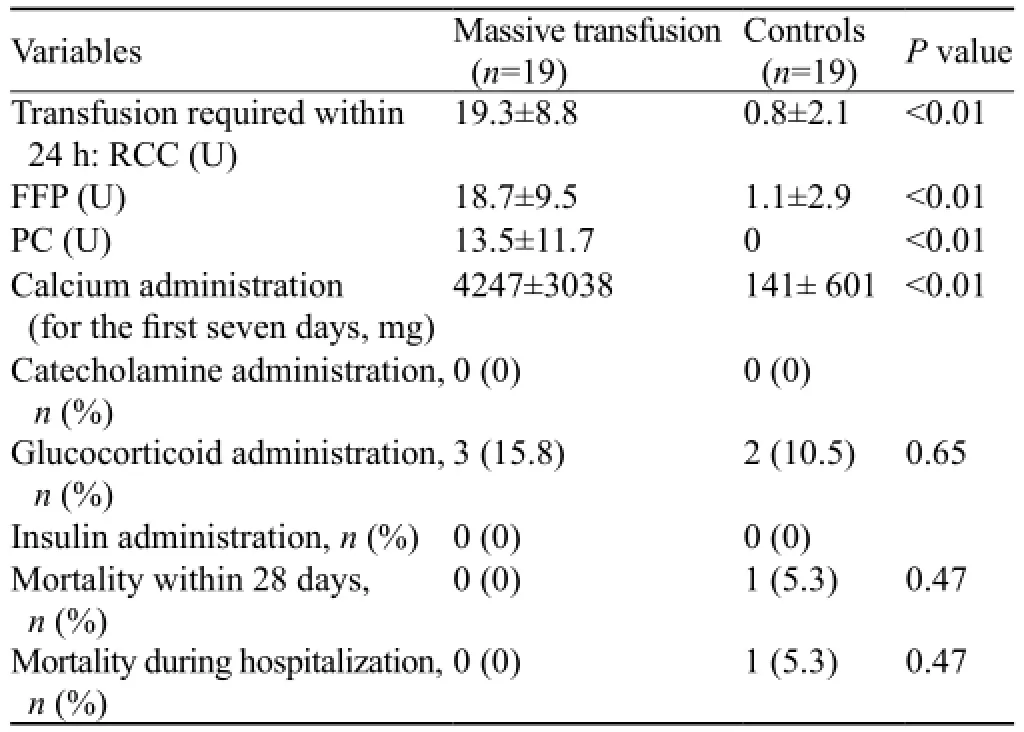
Table 2. Comparison of the 24-hour transfusion requirements, speci fi c therapeutic interventions, and outcomes between the massive transfusion and control groups
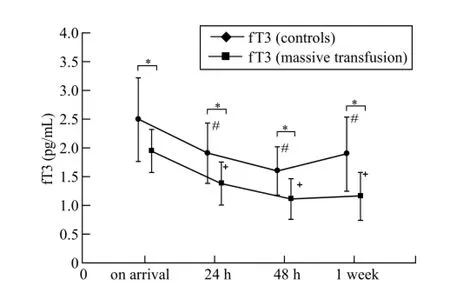
Figure 1. Serial changes in free triiodothyronine at different sampling times in the 2 groups (mean±standard deviation).*P<0.05 compared with the control group;#P<0.05 compared with data at admission in the control group;+P<0.05 compared with data at admission in the massive transfusion group. Shaded area represents normal free triiodothyronine reference range.
Comparison of thyroid hormone levels
Initial fT3 levels were significantly lower in group M than in group C (1.95±0.37 versus 2.49±0.72 pg/mL; P<0.01) and remained low until 1 week after admission (Figure 1). Initial fT4 levels between the two groups were not significantly different at admission (1.00±0.26 versus 1.15±0.23 ng/dL; P=0.08) or during the fi rst 1 week after admission (Figure 2). Initial TSH levels were higher in group M than in group C but not signi fi cantly different between the 2 groups (1.91±1.35 versus 1.49 ±0.51 μIU/ mL; P=0.4). TSH levels at 1 week after admission were higher than those at admission in group C (1.99±1.64 versus 1.48±0.5 μIU/mL; P<0.05; Figure 3).
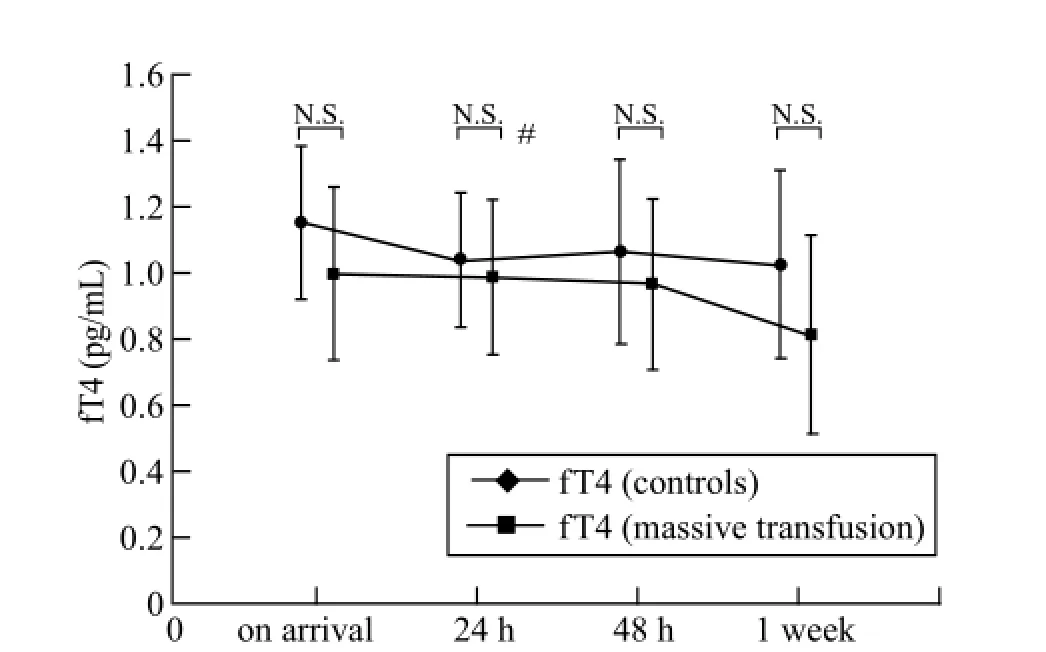
Figure 2. Serial changes in free thyroxine at different sampling times in the 2 groups (mean±standard deviation). No signi fi cant differences were observed between the two groups. Shaded area represents normal fT4 reference range.
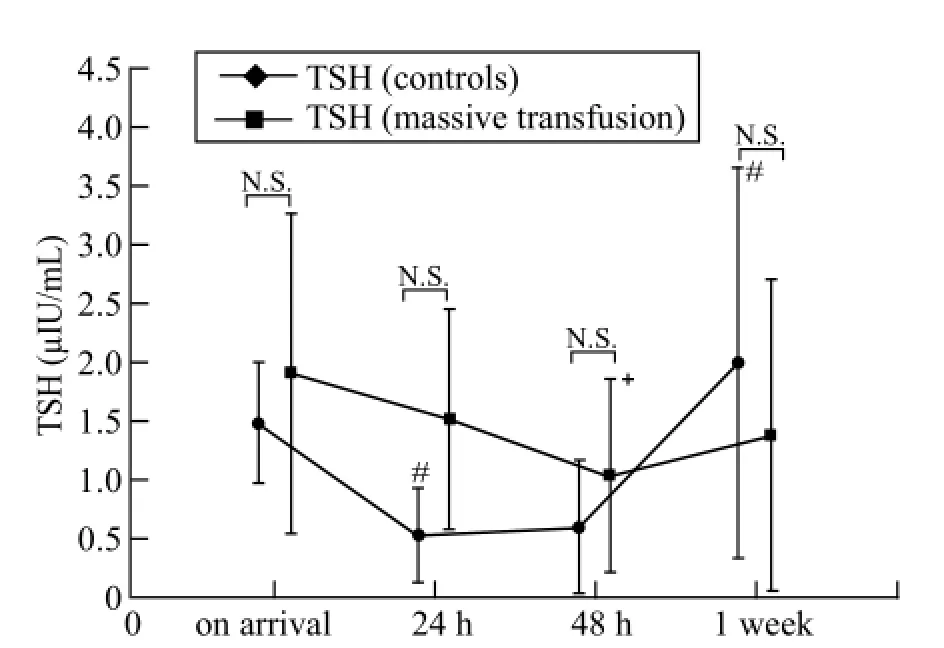
Figure 3. Serial changes in thyroid stimulating hormone levels at different sampling times in the 2 groups (mean±standard deviation).#P<0.05 compared with data at admission in the control group;+P <0.05 compared with data at admission in the massive transfusion group. Shaded area represents normal TSH reference range.
DISCUSSION
This study represents the largest and longest observation of fT3 levels 1 week after injury. Thyroid hormone levels, particularly fT3, were found to markedly change immediately after injury. In the current study, fT3 was reduced below the lower limit of the normal range, but fT4 and TSH levels were not significantly reduced, indicating that typical NTIS occurs in trauma patients requiring massive transfusion. Although group M showed NTIS, the mortality rate was not different between the two groups.
Vitek et al[14]demonstrated that alteration in thyroid hormone levels was associated with massive transfusion over a short period but neither determined fT3 levels nor compared them with a control group. Although Grill et al[11]examined fT3, all levels were below the lower limit of 0.92 pg/dL. Therefore, they did not demonstrate alterations.
Hemodilution induced by intravenous resuscitation and the loss of carrier proteins from hemorrhage could have contributed to the rapid decline in fT3.[11,15]However, in the current survey, the rate of fT3 decline from 24 hours onward in both groups was similar, at 23.4% and 28.9% in groups C and M, respectively. Moreover, fT4 levels in group M remained static despite a considerable level of resuscitation, which did not involve the administration of thyroid hormones. Hemodilution was not considered a major factor affecting thyroid hormone levels of the trauma patients in this study.
Grill et al[11]reported that trauma patients requiring more than 5 units of PRBC had T4 and T3 levels on admission that were lower than the normal range. In the current study, however, fT4 was not reduced below the normal range at any stage. This difference is likely caused by the degree of severity, as explained by Warmer and Beckett.[1]Whereas ISS levels were comparable between the present study (30.7±1.7) and that of Grill et al (28±18), lactate levels on admission varied considerably from 3.0 ±1.7 to 11.4±7.4 mmol/L. In the current study, reduced severity was therefore associated with normal fT4.
A dog hemorrhagic-shock model demonstrated an initial rise followed by a decrease of fT3, after only 20 minutes of shock.[16]Vitek et al[14]proposed a biphasic dysfunctional thyroid response in injured patients, with an initial brief rise in TSH and T3 levels followed by a subsequent reduction within 6–18 hours. In that study, the mean interval between injury and hospital admission was 96±38 min, whereas the corresponding intervals in groups M and C of our study were 47.2±21.8 and 51.5±13.9 min, respectively. However, despite the much shorter interval between injury and hospital admission in the present study, initial rises in fT3 or TSH were not observed in blunt trauma patients. This is consistent with the report of Grill et al, who observed that no biphasic response occurred in patients with penetrating trauma.[11]Therefore, we assume that the initial biphasic response does not occur in humans; if it does, the fi rst phase either occurs earlier than we have assessed to date.
TSH levels were found to be within the normal range, with no significant difference between the two groups at any time point. However, TSH levels remained relatively higher in group M than in group C for the initial 48 hours and were markedly higher in group C by day 7. The rise in TSH during recovery consistently preceded that of free T3 and free T4, suggesting that this rise is necessary in some patients to return thyroid hormone homoeostasis to normal during recovery.[16]These data also suggest that group C recovered earlier than group M, but both groups would have recovered by the second week of hospitalization. Compared with the changes after elective surgery, those in patients with shock or injury have a more rapid onset, greater intensity, and longer duration.[17]
It remains to be clarified whether low fT3 serum levels have a direct impact on outcome and prognosis in trauma patients. T3 is capable of entering mitochondria through membrane receptors, making T3 a potentially important regulator of mitochondrial activity.[18]Supplemental intravenous T3 following experimental hemorrhagic shock appeared to improve both cardiac function and survival in animal models.[13,19,20]During resuscitation, T3 may exert beneficial effects by acting on cardiovascular receptors to improve hemodynamic function at a critical stage in shock. In the current study, however, because the inclusion criteria included trauma patients surviving for longer than 24 hours after admission, the efficacy of T3 was not evaluated during the initial resuscitation period.
The limitation of this study is that the observation period of 1 week was not sufficient to confirm the recovery of thyroid hormone levels after severe trauma. Second, the control group was defined as patients with ISS >9, but an ISS >16 may have been more appropriate. Third, the current study was small, and a larger study is necessary to assess the impact of NTIS on mortality in trauma patients.
In conclusion, typical NTIS was observed in trauma patients requiring massive transfusion. When hemostasis and circulatory stabilization are achieved in traumapatients following initial resuscitation and treatment, the prognosis is not strongly associated with NTIS. Therefore, supplemental thyroid hormones cannot be considered appropriate based on our results. Further research is required into the changes in the initial resuscitation period.
Funding:This work was funded through a grant from the Marumo Fund.
Ethical approval:Not needed.
Conflicts of interest:All authors declare that they have no con fl icts of interest.
Contributors:All listed authors have contributed meaningfully to the content, writing and editing of this manuscript. The manuscript has been read and approved by all the authors, and all authors believe the manuscript to represent honest and original work.
REFERENCES
1 Warner MH, Beckett GJ. Mechanisms behind the non-thyroidal illness syndrome: an update. J. Endocrinol. 2010; 205: 1–13.
2 Scoscia E, Baglioni S, Eslami A, Iervasi G, Monti S, Todisco T. Low triiodothyronine (T3) state: a predictor of outcome in respiratory failure? Results of a clinical pilot study. Eur J Endocrinol 2004; 151: 557–560.
3 Hamilton MA, Stevenson LW, Luu M, Walden JA. Altered thyroid hormone metabolism in advanced heart failure. J Am Coll Cardiol 1990; 16: 91–95.
4 Sawin CT, Chopra D, Albano J, Azizi F. The free triiodothyronine (T3) index. Ann Intern Med 1978; 88: 474–477.
5 Rink C, Siersleben U, Haerting J, Mende T, Nilius R. Development of the low-T3-syndrome and prognosis assessment in patients with liver cirrhosis. Gastroenterol J 1991; 51: 138–141.
6 Borkowski J, Siemiatkowski A, Wolczynski S, Czaban SL, Jedynak M. Assessment of the release of thyroid hormones in septic shock-prognostic significance. Pol Merkur Lekarski 2005; 18: 45–48
7 Girvent M, Maestro S, Hernández R, Carajol I, Monné J, Sancho JJ, et al. Euthyroid sick syndrome, associated endocrine abnormalities, and outcome in elderly patients undergoing emergency operation. Surgery 1998; 123: 560–567.
8 Gou DY, Su W, Shao YC, Lu YL. Euthyroid sick syndrome in trauma patients with severe inflammatory response syndrome. Chin J Traumatol 2006; 9: 115–117.
9 Phillips RH, Valente WA, Caplan ES, Connor TB, Wiswell JG. Circulating thyroid hormone changes in acute trauma: prognostic implications for clinical outcome. J Ttrauma 1984; 24: 116–119.
10 Aun F, Medeiros-Neto GA, Younes RN, Birolini D, de Oliveira MR. The effect of major trauma on the pathways of thyroid hormone metabolism. J Trauma 1983; 23: 1048–1051.
11 Grill E, Strong M, Sonnad SS, Sarani B, Pascual J, Collins H, et al. Altered thyroid function in severely injured patients. J Surg Res 2013; 179: 132–137.
12 Facktor MA, Mayor GH, Nachreiner RF, D'Alecy LG. Thyroid hormone loss and replacement during resuscitation from cardiac arrest in dogs. Resuscitation 1993; 26: 141–162.
13 Dulchavsky SA, Lucas CE, Ledgerwood AM, Grabow D, Brown TR, Bagchi N. Triiodothyronine (T3) improves cardiovascular function during hemorrhagic shock. Circ Shock 1993; 39: 68–73.
14 Vitek V, Shatney CH. Thyroid hormone alterations in patients with shock and injury. Injury 1987; 18: 336–341.
15 Hoffenberg R, Ramsden DB. The transport of thyroid hormones. Clin Sci (Lond) 1983; 65: 337–342.
16 Hamblin PS, Dyer SA, Mohr VS, Le Grand BA, Lim CF, Tuxen DV, et al. Relationship between thyrotropin and thyroxine changes during recovery from severe hypothyroxinemia of critical illness. J Clin Endocrinol Metab 1986; 62: 717–722.
17 Vitek V, Shatney CH, Lang DJ, Cowley RA. Thyroid hormone responses in hemorrhagic shock: study in dogs and preliminary fi ndings in humans. Surgery 1983; 93: 768–777.
18 Sterling K, Brenner MA, Sakurada T. Rapid effect of triiodothyronine on the mitochondrial pathway in rat liver in vivo. Science 1980; 210: 340–342.
19 Shigematsu H, Smith RA, Shatney CH. Triiodothyronine increases survival in canine hemorrhagic shock. Resuscitation 1987; 15: 233–243.
20 Yuan XQ, Shatney CH, Dewitt DS, Prough DS, Smith RA. Triiodothyronine (T3) antagonizes adverse effects of high circulating reverse-T3 (rT3) during hemorrhagic shock. Am Surg 1988; 54: 720–725.
Received May 20, 2014
Accepted after revision October 9, 2014
World J Emerg Med 2014;5(4):270–274
10.5847/wjem.j.issn.1920–8642.2014.04.005
 World journal of emergency medicine2014年4期
World journal of emergency medicine2014年4期
- World journal of emergency medicine的其它文章
- Instructions for Authors
- A man with a fracture from minor trauma
- A minimally invasive multiple percutaneous drainage technique for acute necrotizing pancreatitis
- Effects of mild hypothermia on the ROS and expression of caspase-3 mRNA and LC3 of hippocampus nerve cells in rats after cardiopulmonary resuscitation
- Simvastatin inhibits apoptosis of endothelial cells induced by sepsis through upregulating the expression of Bcl-2 and downregulating Bax
- Heat-related illness in Jinshan District of Shanghai: A retrospective analysis of 70 patients
